J Rheum Dis.
2013 Oct;20(5):336-341. 10.4078/jrd.2013.20.5.336.
Primary Sjogren's Syndrome Presenting with Rapidly Progressive Cognitive Impairment
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea.
- 2Department of Internal Medicine, Capital Armed Forces General Hospital, Seongnam, Korea.
- 3Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. yn35@snu.ac.kr
- KMID: 2223013
- DOI: http://doi.org/10.4078/jrd.2013.20.5.336
Abstract
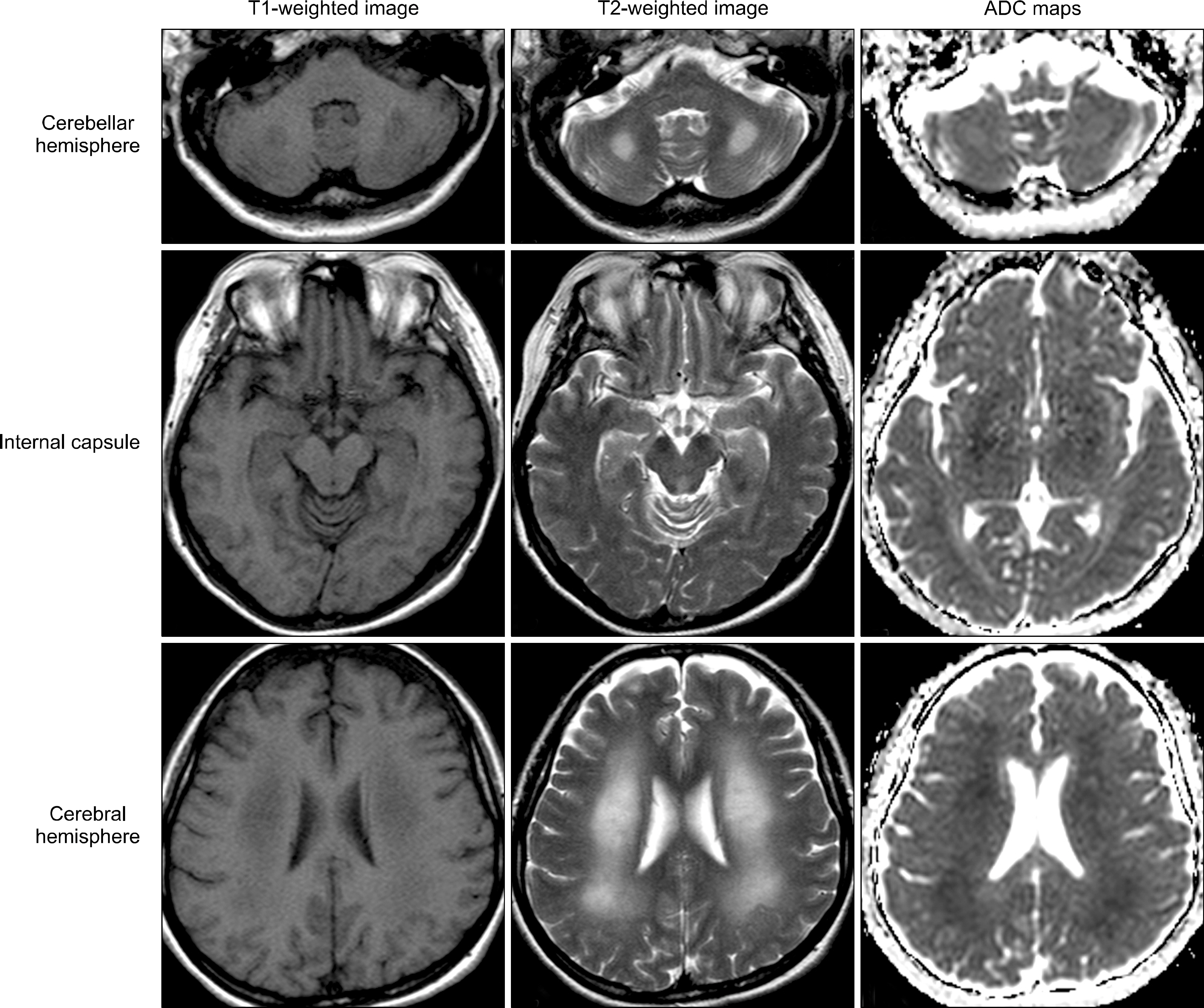
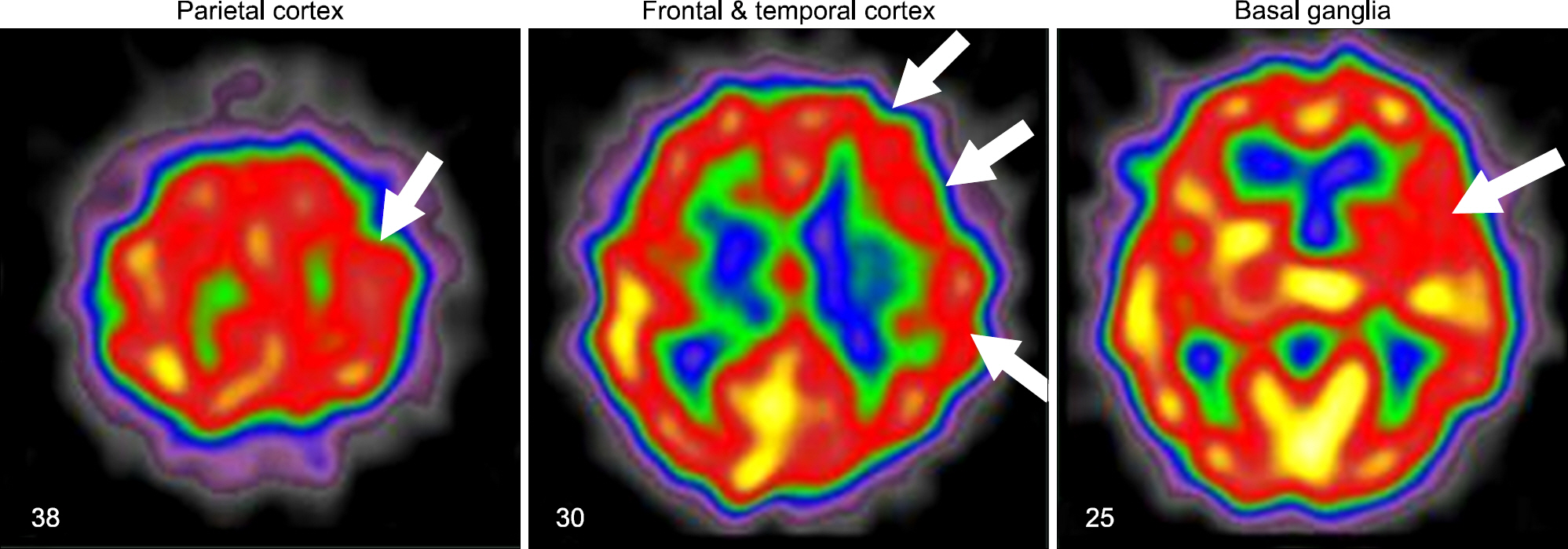
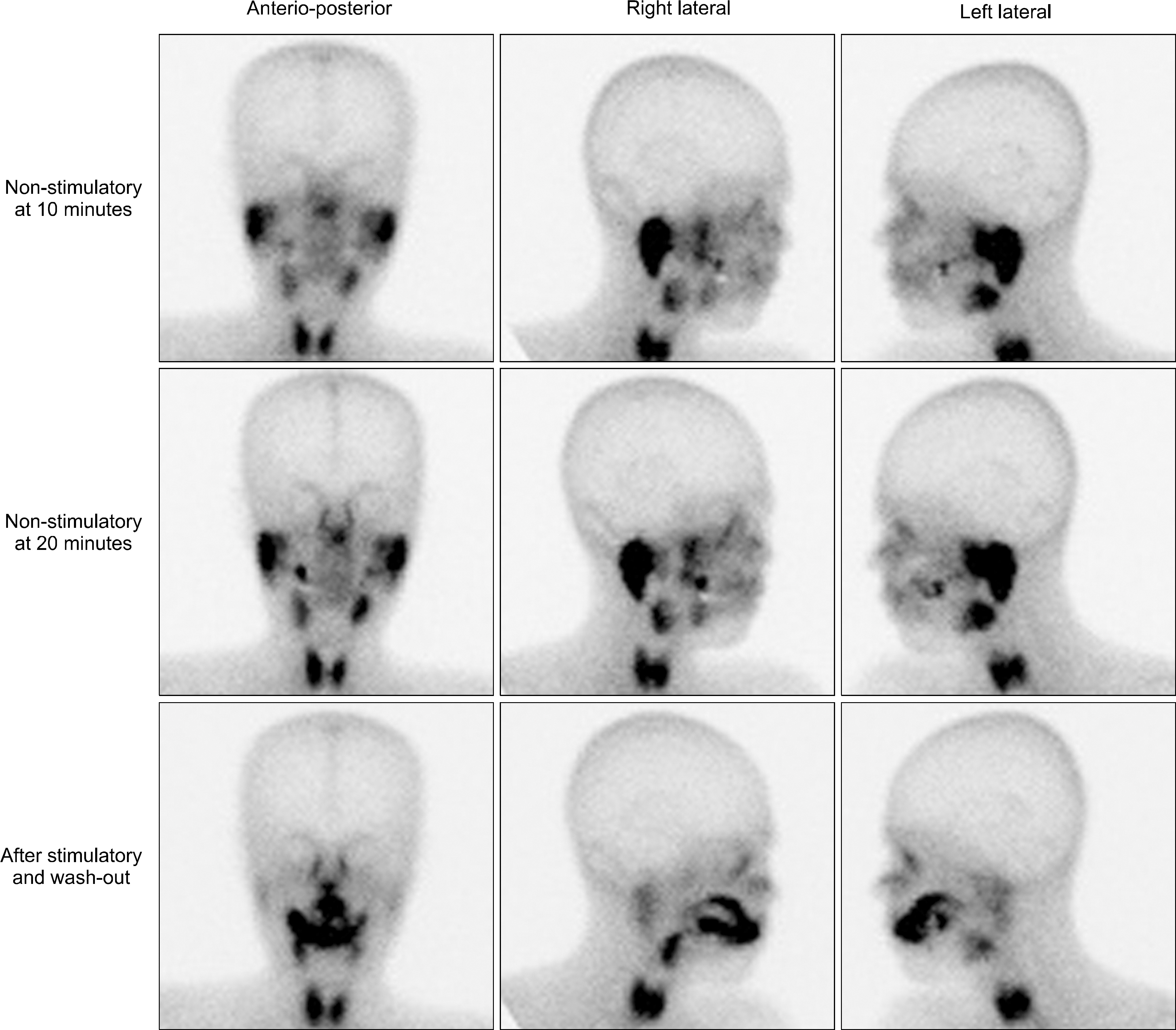
- Primary Sjogren's syndrome (pSS) is characterized by chronic inflammation and dysfunction in exocrine organs; however, it also has protean clinical features, including neuropsychiatric symptoms. A major neurological manifestation is peripheral neuropathy and involvement of the central nervous system is uncommonly described in pSS. A 52-year-old female was admitted because of depression, dysarthria, gait abnormality, and memory disturbance, which had developed over two months, and was diagnosed as pSS. She was treated successfully with high-dose glucocorticoid and cyclophosphamide pulse therapy without recurrence during the follow-up period of two years. Herein, we describe the first Korean case of pSS presenting with rapidly progressive cognitive impairment along with a review of the literature.
MeSH Terms
Figure
Reference
-
References
1. Chai J, Logigian EL. Neurological manifestations of primary Sjögren's syndrome. Curr Opin Neurol. 2010; 23:509–13.2. Segal B, Carpenter A, Walk D. Involvement of nervous system pathways in primary Sjögren's syndrome. Rheum Dis Clin North Am. 2008; 34:885–906.
Article3. Caselli RJ, Scheithauer BW, Bowles CA, Trenerry MR, Meyer FB, Smigielski JS, et al. The treatable dementia of Sjögren's syndrome. Ann Neurol. 1991; 30:98–101.
Article4. Kawashima N, Shindo R, Kohno M. Primary Sjögren's syndrome with subcortical dementia. Intern Med. 1993; 32:561–4.5. Johnstone B, Pepmuelle PH, Vieth AZ, Komatireddy G. Effective treatment of neuropsychological deficits in Sjögren's syndrome. Appl Neuropsychol. 1996; 3:122–7.6. Michel L, Toulgoat F, Desal H, Laplaud DA, Magot A, Hamidou M, et al. Atypical neurologic complications in patients with primary Sjögren's syndrome: report of 4 cases. Semin Arthritis Rheum. 2011; 40:338–42.
Article7. Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, et al. European Study Group on Classification Criteria for Sjögren's Syndrome. Classification criteria for Sjögren's syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis. 2002; 61:554–8.8. Shiboski SC, Shiboski CH, Criswell L, Baer A, Challacombe S, Lanfranchi H, et al. Sjögren's International Collaborative Clinical Alliance (SICCA) Research Groups. American College of Rheumatology classification criteria for Sjögren's syndrome: a data-driven, expert consensus approach in the Sjögren's International Collaborative Clinical Alliance cohort. Arthritis Care Res (Hoboken). 2012; 64:475–87.9. Seo SH, Kim HS, Kwok SK, Ju JH, Kim SH, Yoon CH, et al. Extraglandular manifestations and autoantibodies of Korean patients with primary Sjögren's syndrome. J Korean Rheum Assoc. 2007; 14:43–50.
Article10. Cho JH, Kim SM, Kim JH, Chu CK, Lee MH, Shin HW, et al. Two cases of primary Sjögren's syndrome presenting as relapsing-remitting multiple sclerosis. J Korean Neurol Assoc. 2004; 22:410–13.11. Choi HJ, Shin K, Kang EH, Im CH, Lee YJ, Lee EB, et al. Primary Sjögren's syndrome presenting as acute transverse myelitis. Korean J Med. 2005; 68:463–6.12. Min JH, Kim HJ, Kim BJ, Lee KW, Sunwoo IN, Kim SM, et al. Brain abnormalities in Sjogren syndrome with recurrent CNS manifestations: association with neuromyelitis optica. Mult Scler. 2009; 15:1069–76.
Article13. Kim MJ, Lee MC, Lee JH, Chung SJ. Cerebellar degener-ation associated with Sjögren's syndrome. J Clin Neurol. 2012; 8:155–9.
Article14. Delalande S, de Seze J, Fauchais AL, Hachulla E, Stojkovic T, Ferriby D, et al. Neurologic manifestations in primary Sjögren syndrome: a study of 82 patients. Medicine (Baltimore). 2004; 83:280–91.15. Alexander EL, Ranzenbach MR, Kumar AJ, Kozachuk WE, Rosenbaum AE, Patronas N, et al. Anti-Ro(SS-A) autoantibodies in central nervous system disease associated with Sjögren's syndrome (CNS-SS): clinical, neu-roimaging, and angiographic correlates. Neurology. 1994; 44:899–908.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebellar Degeneration Associated with Sjogren's Syndrome
- Distal Renal Tubular Acidosis with Nephrocalcinosis in a Patient with Primary Sjogren's Syndrome
- Two Cases of Primary Sjogren's Syndrome Presenting as Relapsing-Remitting Multiple Sclerosis
- A Case of Sjogren's Syndrome with Hyperthyroidism
- A Case of Primary Sjiigren's Syndrome with Hypokalemic Paralysis and Renal Tubular Acidosis