J Korean Ophthalmol Soc.
2013 Feb;54(2):338-345. 10.3341/jkos.2013.54.2.338.
The Wound Healing Effects of AmniSite-Lens in Rabbits
- Affiliations
-
- 1Department of Ophthalmology, Chung-Ang University College of Medicine, Seoul, Korea. jck50ey@kornet.net
- KMID: 2216672
- DOI: http://doi.org/10.3341/jkos.2013.54.2.338
Abstract
- PURPOSE
The effects of AmniSite-Lens on wound healing were evaluated for a burn wound on a rabbit cornea.
METHODS
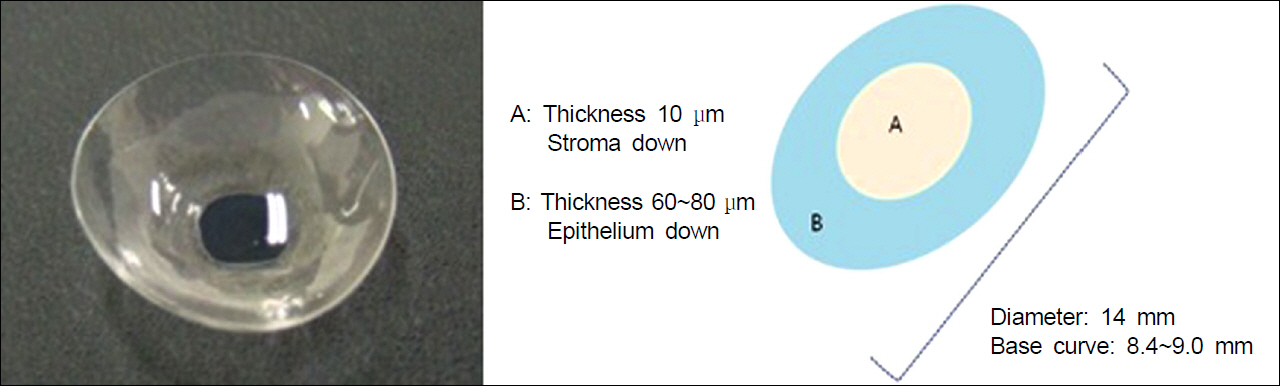
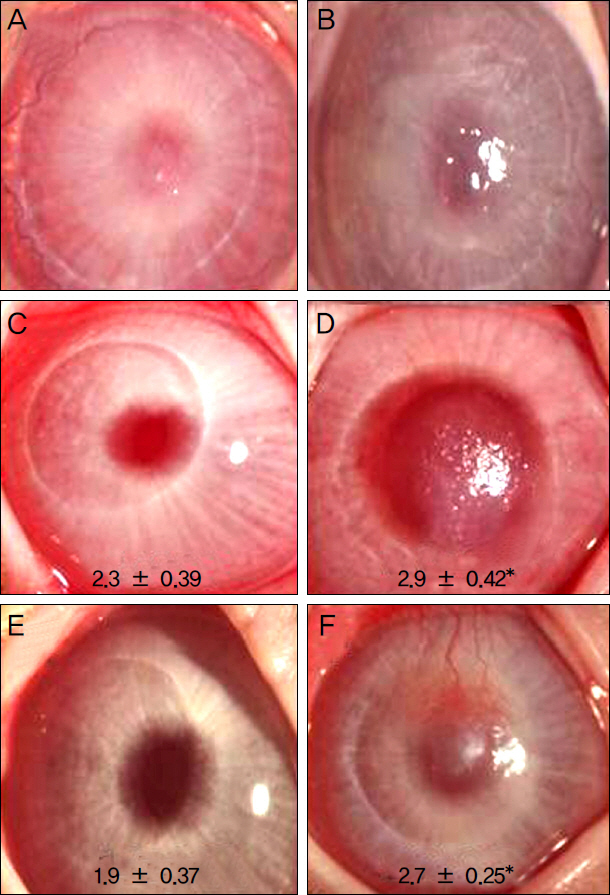
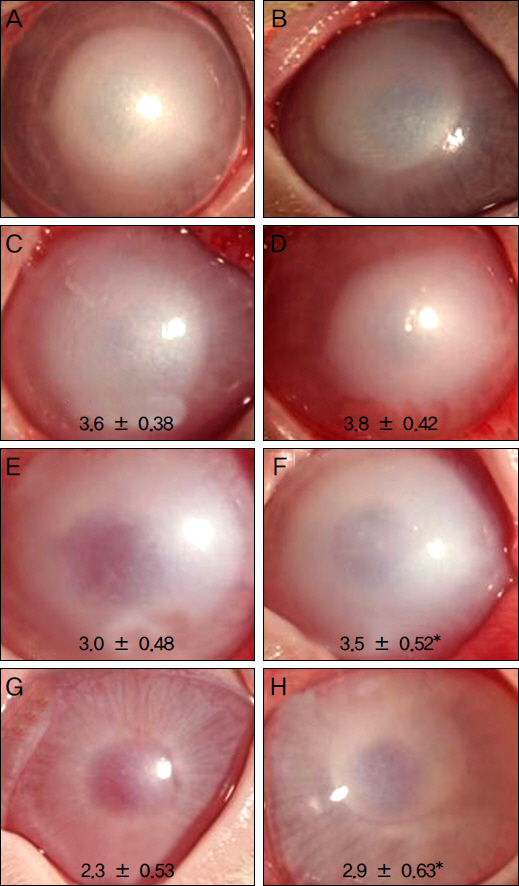
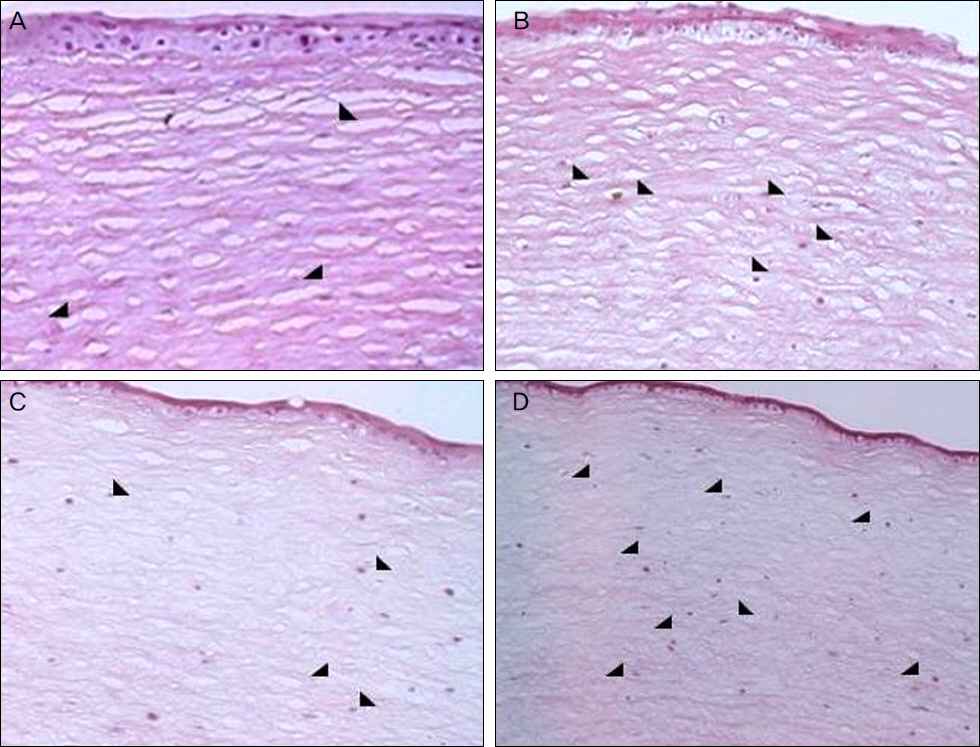
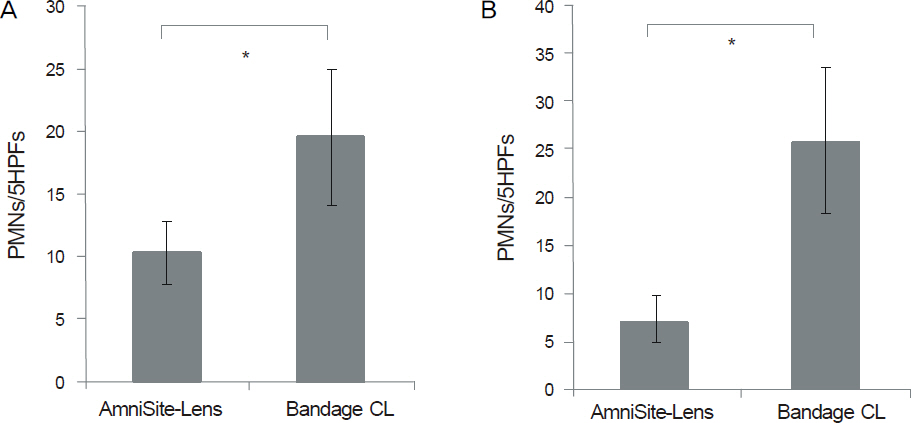
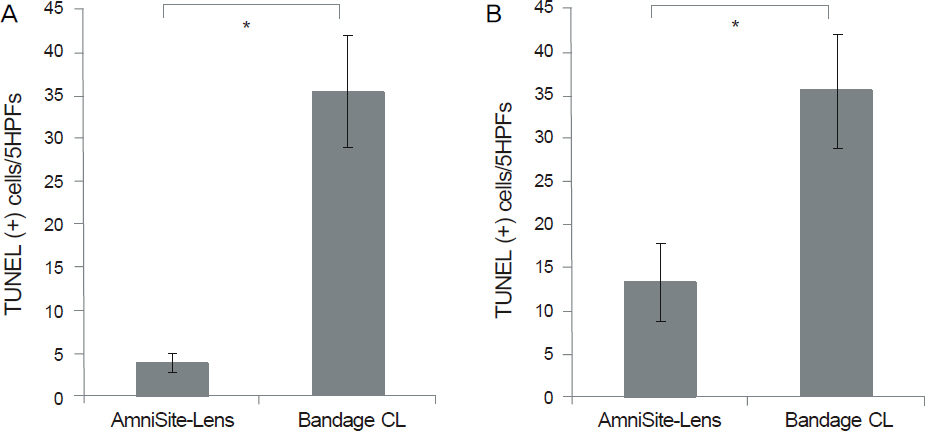
A chemical burn was inflicted on the cornea of rabbits using 0.1N NaOH and a superficial keratectomy with trephine was performed. The control group consisted of rabbits with a bandage contact lens (Focus Lens) after the operation. In the other group, the AmniSite-Le was applied on the rabbits' cornea. The rabbits were evaluated for the following: 1) the time of epithelialization; 2) the grade of corneal opacity; and 3) the histological analysis by evaluation of inflammatory reaction and apoptotic keratocytes.
RESULTS
In the alkali-burn model, the time of epithelialization in the AmniSite-Lens group was not statistically significant compared with the bandage contact lens group. There was no difference of corneal opacity at postoperative week 1. The corneal opacity in the AmniSite-Lens group was clearer than the bandage contact lens group at postoperative weeks 4 and 8 and the difference of corneal opacity was statistically significant. In the keratectomy model, the time of epithelialization in the AmniSite-Lens group was not statistically significant compared with the bandage contact lens group. The corneal opacity in the AmniSite-Lens group was clearer than the bandage contact lens group at postoperative weeks 1 and 4 and the difference of corneal opacity was statistically significant.
CONCLUSIONS
The AmniSite-Lens has both the wound healing effect of an amniotic membrane and the convenience of a bandage contact lens.
Keyword
Figure
Reference
-
References
1. Shimmura S, Shimazaki J, Ohashi Y, Tsubota K. Antiinflammatory effects of amniotic membrane transplantation in ocular surface disorders. Cornea. 2001; 20:408–13.
Article2. Kim JS, Kim JC, Na BK, et al. Amniotic membrane patching promotes healing and inhibits proteinase activity on wound healing following acute corneal alkali burn. Exp Eye Res. 2000; 70:329–37.
Article3. Gris O, del Campo Z, Wolley-Dod C, et al. Amniotic membrane implantation as a therapeutic contact lens for the treatment of epithelial disorders. Cornea. 2002; 21:22–7.
Article4. Takano Y, Fukagawa K, Miyake-Kashima M, et al. Dramatic healing of an allergic corneal ulcer persistent for 6 months by amniotic membrane patching in a patient with atopic keratoconjunctivitis: a case report. Cornea. 2004; 23:723–5.5. Choi YS, Kim JY, Wee WR, Lee JH. Effect of the application of human amniotic membrane on rabbit corneal wound healing after excimer laser photorefractive keratectomy. Cornea. 1998; 17:389–95.
Article6. Woo HM, Kim MS, Kweon OK, et al. Effects of amniotic membrane on epithelial wound healing and stromal remodelling after excimer laser keratectomy in rabbit cornea. Br J Ophthalmol. 2001; 85:345–9.
Article7. Seo JW, Ko BW, Lee DJ, Park WC. The effects of amniotic membrane contact lens for cornea wound healing. J Korean Ophthalmol Soc. 2009; 50:989–95.
Article8. De Rotth A. Plastic repair of conjunctival defects with fetal membranes. Arch Ophthalmol. 1940; 23:525–5.
Article9. Batlle JF, Perdomo FJ. Placental membranes as a conjunctival substitute. Ophthalmology. 1993; 100:107.10. Kim JC, Tseng SC. Transplantation of preserved human amniotic membrane for surface reconstruction in severely damaged rabbit corneas. Cornea. 1995; 14:473–84.
Article11. Nakamura T, Inatomi T, Sekiyama E, et al. Novel clinical application of sterilized, freeze-dried amniotic membrane to treat patients with pterygium. Acta Ophthalmol Scand. 2006; 84:401–5.
Article12. Park M, Kim S, Kim IS, Son D. Healing of a porcine burn wound dressed with human and bovine amniotic membranes. Wound Repair Regen. 2008; 16:520–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Freeze-dried bovine amniotic membrane as a cell delivery scaffold in a porcine model of radiation-induced chronic wounds
- The Effects of Amniotic Membrane Contact Lens for Cornea Wound Healing
- Corneal Epithelial Wound Healing After Excimer Laser Photorefractive Keratectomy
- Corneal wound Healing Following Excimer Laser Photorefractive Keratectomy Using Pressure Patch, T-lens and Collagen Shield on Rabbit Cornea
- Experimental study of the effects of fibrin adhesive on wound healing process in rabbits