J Korean Ophthalmol Soc.
2013 Jan;54(1):97-103. 10.3341/jkos.2013.54.1.97.
Comparison of the Efficacy between Time and Spectral Domain Optical Coherence Tomography for the Identification of Vitreomacular Interface
- Affiliations
-
- 1Department of Ophthalmology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea.
- 2Gongduck Seoul Eye Clinic, Seoul, Korea. imoon58@netsgo.com
- KMID: 2216456
- DOI: http://doi.org/10.3341/jkos.2013.54.1.97
Abstract
- PURPOSE
To compare the efficacy of time domain (TD) and spectral domain (SD) optical coherence tomography (OCT) in determining vitreomacular interface (VMI).
METHODS
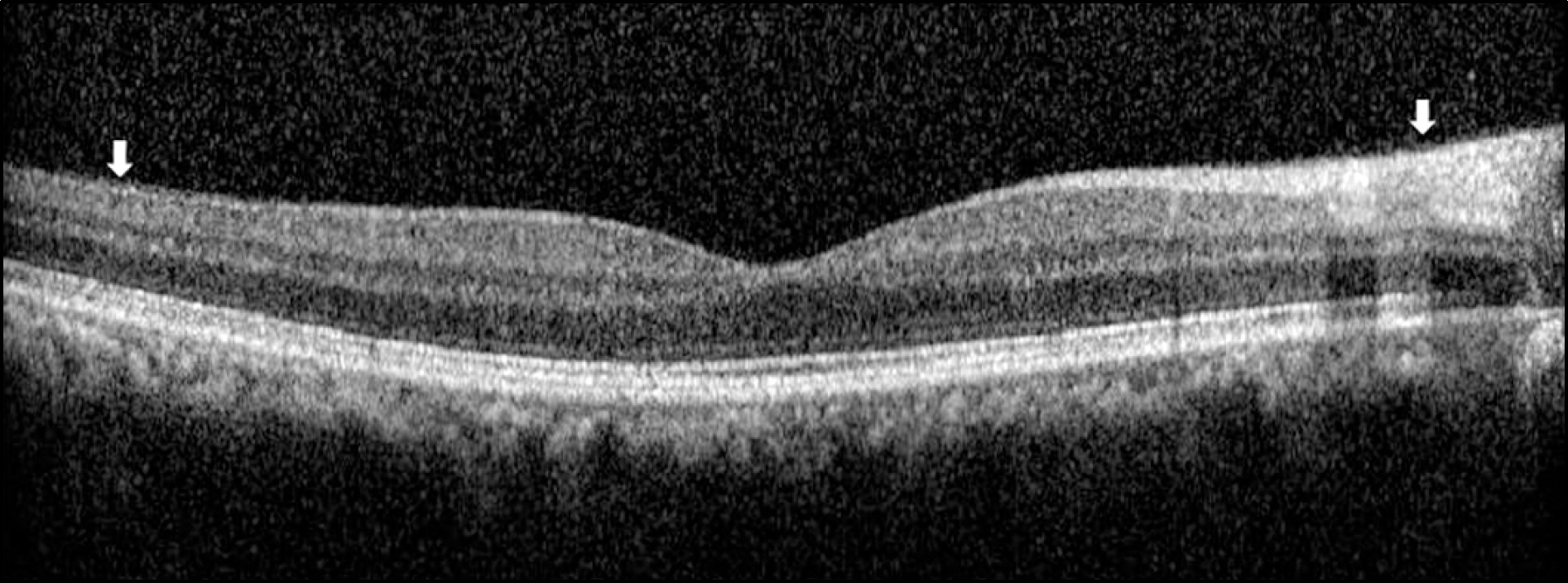
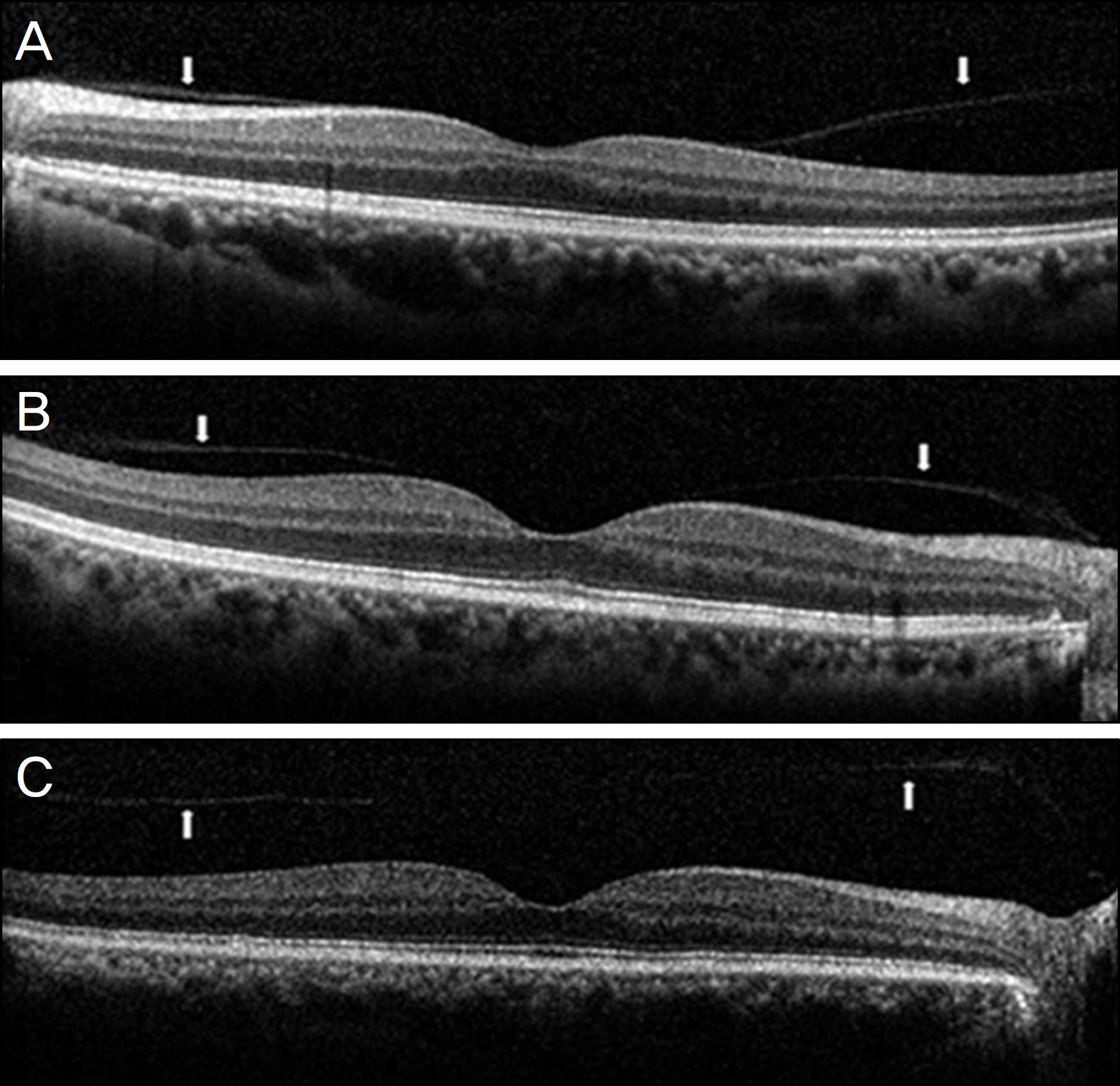
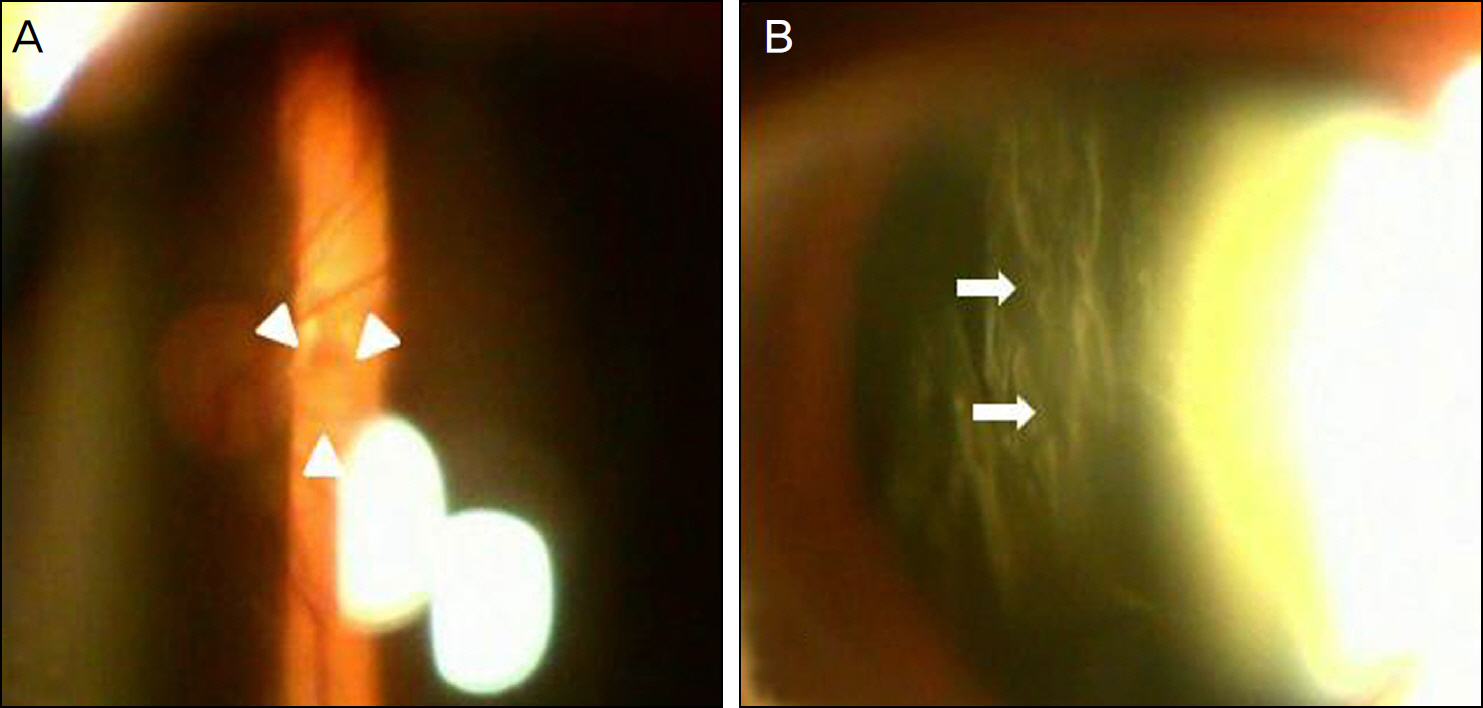
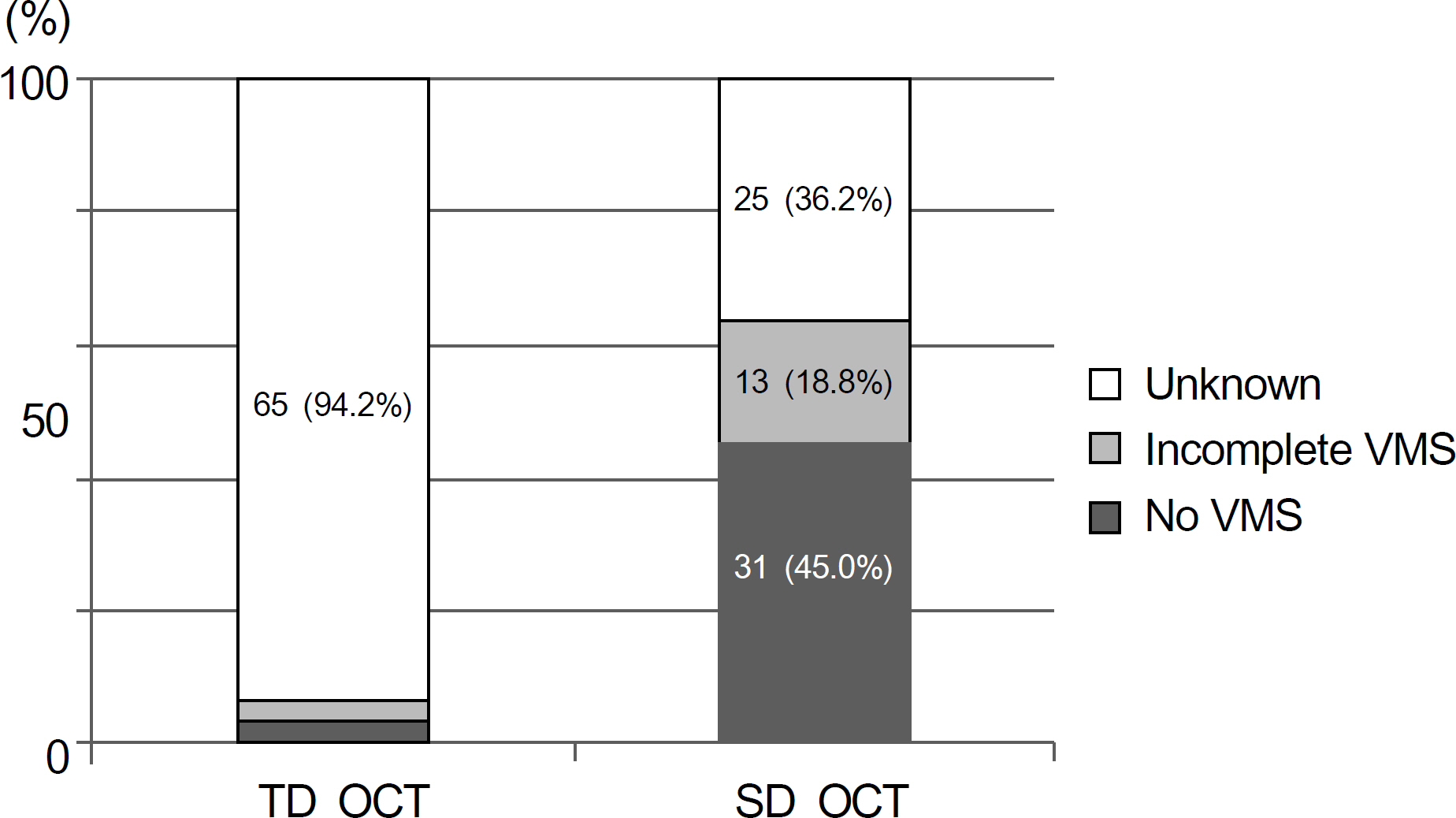
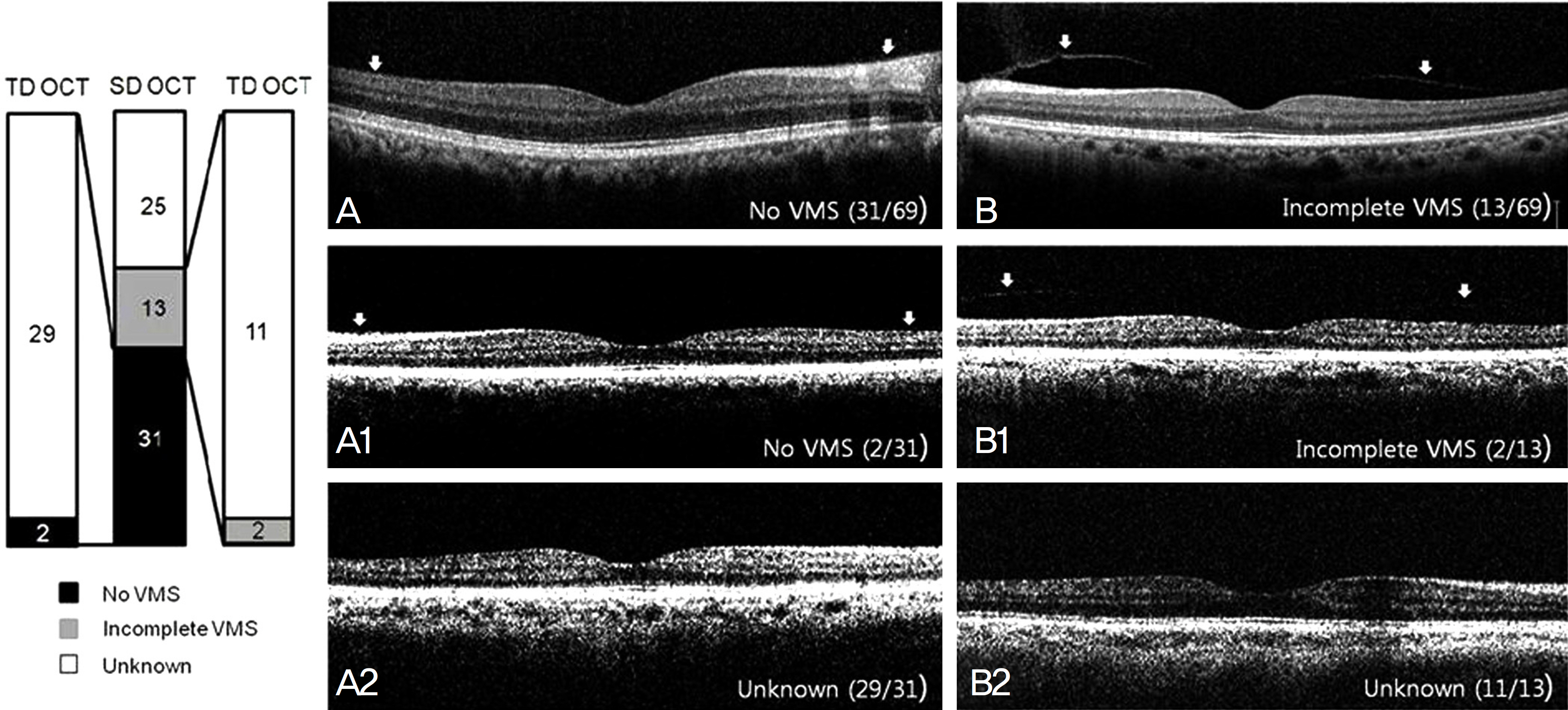
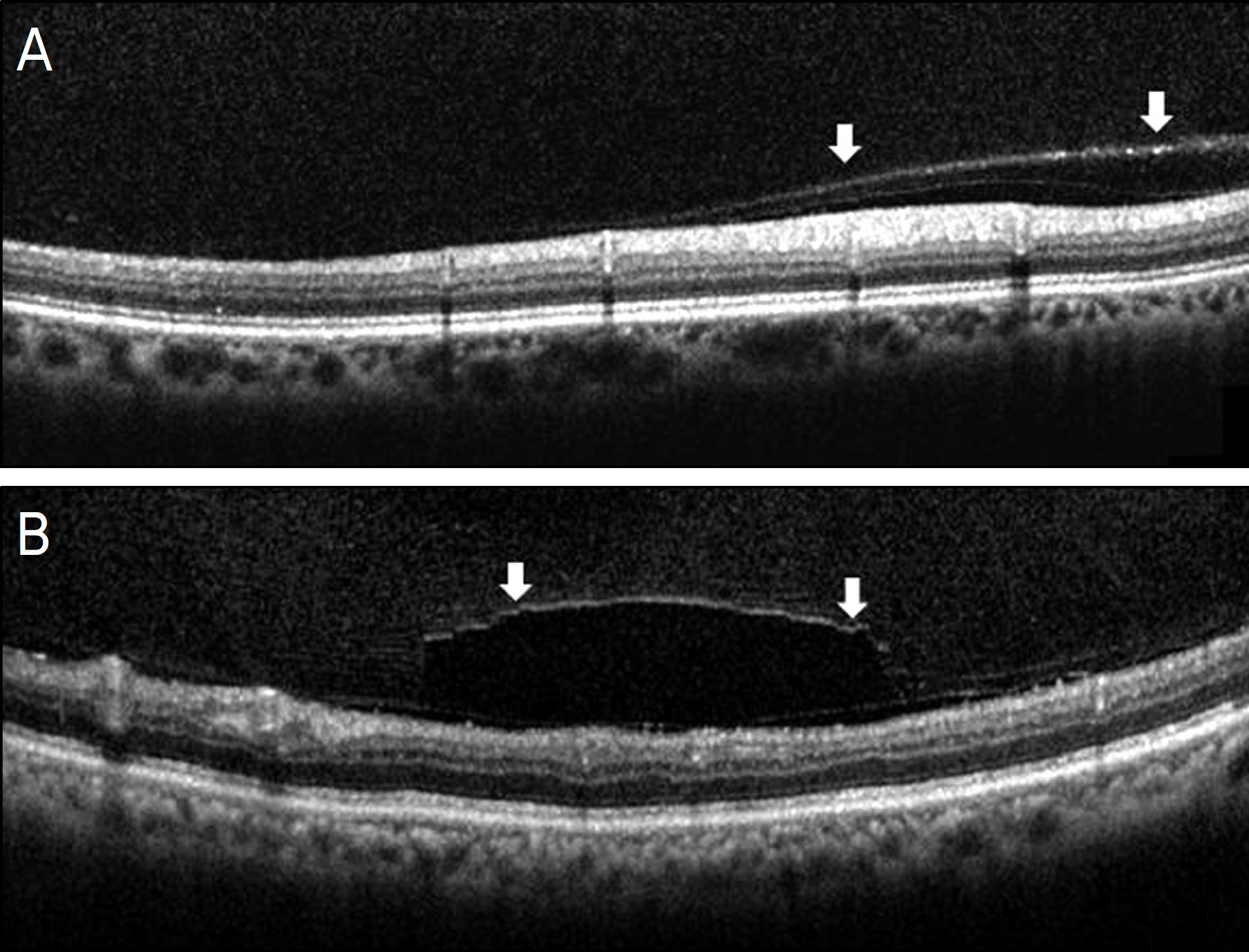
VMIs were evaluated with TD and SD OCT images crossing the fovea horizontally in 69 eyes (mean age 52.7 +/- 15.4 years) and were classified as follows: (1) no vitreomacular separation (VMS), (2) incomplete VMS, and (3) unknown.
RESULTS
In TD OCT, no VMS was observed in 2 eyes (2.9%), incomplete VMS in 2 eyes (2.9%), and unknown in 65 eyes (94.2%). In SD OCT, no VMS was observed in 31 eyes (45.0%), incomplete VMS in 13 eyes (18.8%), and unknown in 25 eyes (36.2%). In 31 eyes with no VMS on SD OCT, 29 eyes (93.5%) presented unknown on TD OCT (p<0.0001). In 13 eyes with incomplete VMS on SD OCT, 2 eyes (15.4%) showed incomplete VMS and 11 eyes (84.6%) showed unknown on TD OCT (p<0.0001). TD OCT was also non-informative in all 25 eyes with unknown on SD OCT.
CONCLUSIONS
SD OCT allows better visualization of VMI than TD OCT, especially in patients with no VMS.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Evaluation of the Cortical Vitreous Using Swept-Source Optical Coherence Tomography in Normal Eyes
Seung Hun Park, Jung Wook Lee, Min Ji Lee, Ju Hyang Lee, In Seok Song, Byung Ro Lee
J Korean Ophthalmol Soc. 2016;57(4):595-600. doi: 10.3341/jkos.2016.57.4.595.
Reference
-
References
1. Patronas M, Kroll AJ, Lou PL, Ryan EA. A review of vitreoretinal interface pathology. Int Ophthalmol Clin. 2009; 49:133–43.
Article2. Voo I, Mavrofrides EC, Puliafito CA. Clinical applications of abdominal coherence tomography for the diagnosis and management of macular diseases. Ophthalmol Clin North Am. 2004; 17:21–31.3. Fisher YL, Slakter JS, Friedman RA, Yannuzzi LA. Kinetic ultrasound evaluation of the posterior vitreoretinal interface. Ophthalmology. 1991; 98:1135–8.
Article4. Hoehn F, Mirshahi A, Hattenbach LO. Optical coherence abdominal for diagnosis of posterior vitreous detachment at the macular region. Eur J Ophthalmol. 2009; 19:442–7.5. Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science. 1991; 254:1178–81.
Article6. Tammewar AM, Bartsch DU, Kozak I, et al. Imaging abdominal interface abnormalities in the coronal plane by abdominal combined scanning laser and optical coherence tomography. Br J Ophthalmol. 2009; 93:366–72.7. Drexler W, Fujimoto JG. State-of-the-art retinal optical coherence tomography. Prog Retin Eye Res. 2008; 27:45–88.
Article8. Luviano DM, Benz MS, Kim RY, et al. Selected clinical abdominals of spectral domain and time domain optical coherence tomography. Ophthalmic Surg Lasers Imaging. 2009; 40:325–8.9. Yi K, Chen TC, de Boer JF. Spectral domain optical coherence tomography. Techniques in Ophthalmology. 2006; 4:170–4.
Article10. Mirza RG, Johnson MW, Jampol LM. Optical coherence abdominal use in evaluation of the vitreoretinal interface: a review. Surv Ophthalmol. 2007; 52:397–421.11. Brennen PM, Kagemann L, Friberg TR. Comparison of Stratus OCT and Cirrus HD-OCT imaging in macular diseases. Ophthalmic Surg Lasers Imaging. 2009; 40:25–31.12. Nigam N, Bartsch DU, Cheng L, et al. Spectral domain optical abdominal tomography for imaging ERM, retinal edema, and abdominal interface. Retina. 2010; 30:246–53.13. Ishikawa H, Gürses-Ozden R, Hoh ST, et al. Grayscale and pro-portion-corrected optical coherence tomography images. Ophthalmic Surg Lasers. 2000; 31:223–8.
Article14. Perichon JY, Brasseur G, Uzzan J. [Ultrasonographic study of abdominal vitreous detachment in emmetropic eyes]. J Fr Ophthalmol. 1993; 16:538–44.15. Zeimer R, Shahidi M, Mori M, et al. A new method for rapid abdominal of the retinal thickness at the posterior pole. Invest Ophthalmol Vis Sci. 1996; 37:1994–2001.16. Legarreta JE, Gregori G, Punjabi OS, et al. Macular thickness measurements in normal eyes using spectral domain optical abdominal tomography. Ophthalmic Surg Lasers Imaging. 2008; 39(4 Suppl):S43–9.17. Uchino E, Uemura A, Ohba N. Initial stages of posterior vitreous detachment in healthy eyes of older persons evaluated by optical coherence tomography. Arch Ophthalmol. 2001; 119:1475–9.
Article18. Johnson MW. Posterior vitreous detachment: evolution and abdominals of its early stages. Am J Ophthalmol. 2010; 149:371–82. e1.19. Gaudric A, Haouchine B, Massin P, et al. Macular hole formation: new data provided by optical coherence tomography. Arch Ophthalmol. 1999; 117:744–51.20. Weber-Krause B, Eckardt C. [Incidence of posterior vitreous abdominal in the elderly]. Ophthalmologe. 1997; 94:619–23.21. Yonemoto J, Ideta H, Sasaki K, et al. The age of onset of posterior vitreous detachment. Graefes Arch Clin Exp Ophthalmol. 1994; 232:67–70.22. Kishi S, Demaria C, Shimizu K. Vitreous cortex remnants at the fovea after spontaneous vitreous detachment. Int Ophthalmol. 1986; 9:253–60.
Article23. Gupta P, Yee KM, Garcia P, et al. Vitreoschisis in macular diseases. Br J Ophthalmol. 2011; 95:376–80.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and Treatment of Vitreomacular Traction Syndrome Using Optical Coherence Tomography
- A Case of Ocular Toxoplasmosis Imaged with Spectral Domain Optical Coherence Tomography
- Fundus Autofluorescence, Fluorescein Angiography and Spectral Domain Optical Coherence Tomography Findings of Retinal Astrocytic Hamartomas in Tuberous Sclerosis
- Spectral Domain Optical Coherence Tomography Findings of Butterfly Shaped Pigment Dystrophy
- Comparison of Spectral-Domain and Time-Domain Optical Coherence Tomography in Solar Retinopathy