J Korean Ophthalmol Soc.
2015 Jan;56(1):142-147. 10.3341/jkos.2015.56.1.142.
Multimodality Diagnostic Imaging in Unilateral Acute Idiopathic Maculopathy
- Affiliations
-
- 1Saevit Eye Hospital, Goyang, Korea. kiseok-kim@daum.net
- KMID: 2216169
- DOI: http://doi.org/10.3341/jkos.2015.56.1.142
Abstract
- PURPOSE
To report multimodality diagnostic imaging in a case of unilateral acute idiopathic maculopathy.
CASE SUMMARY
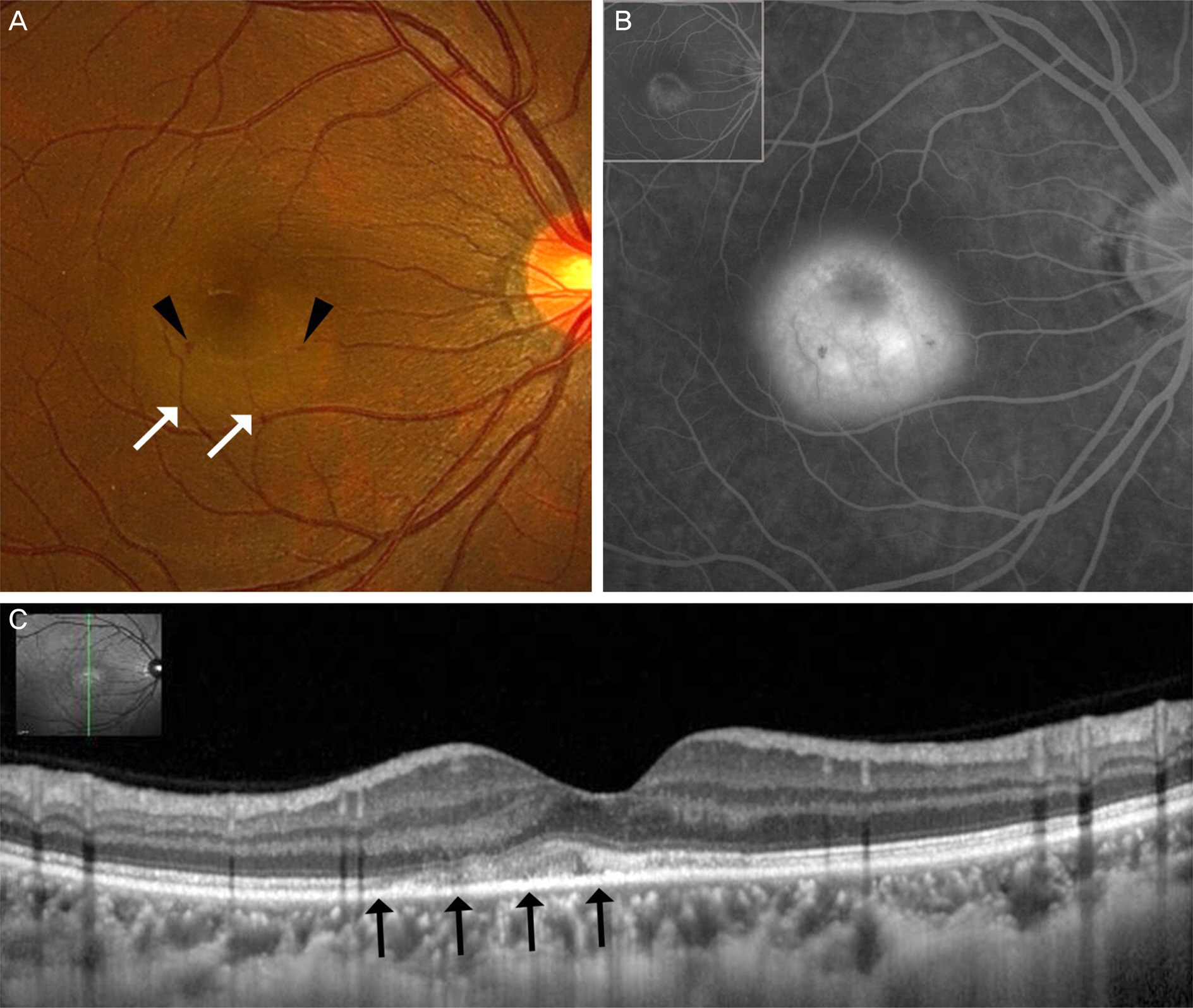
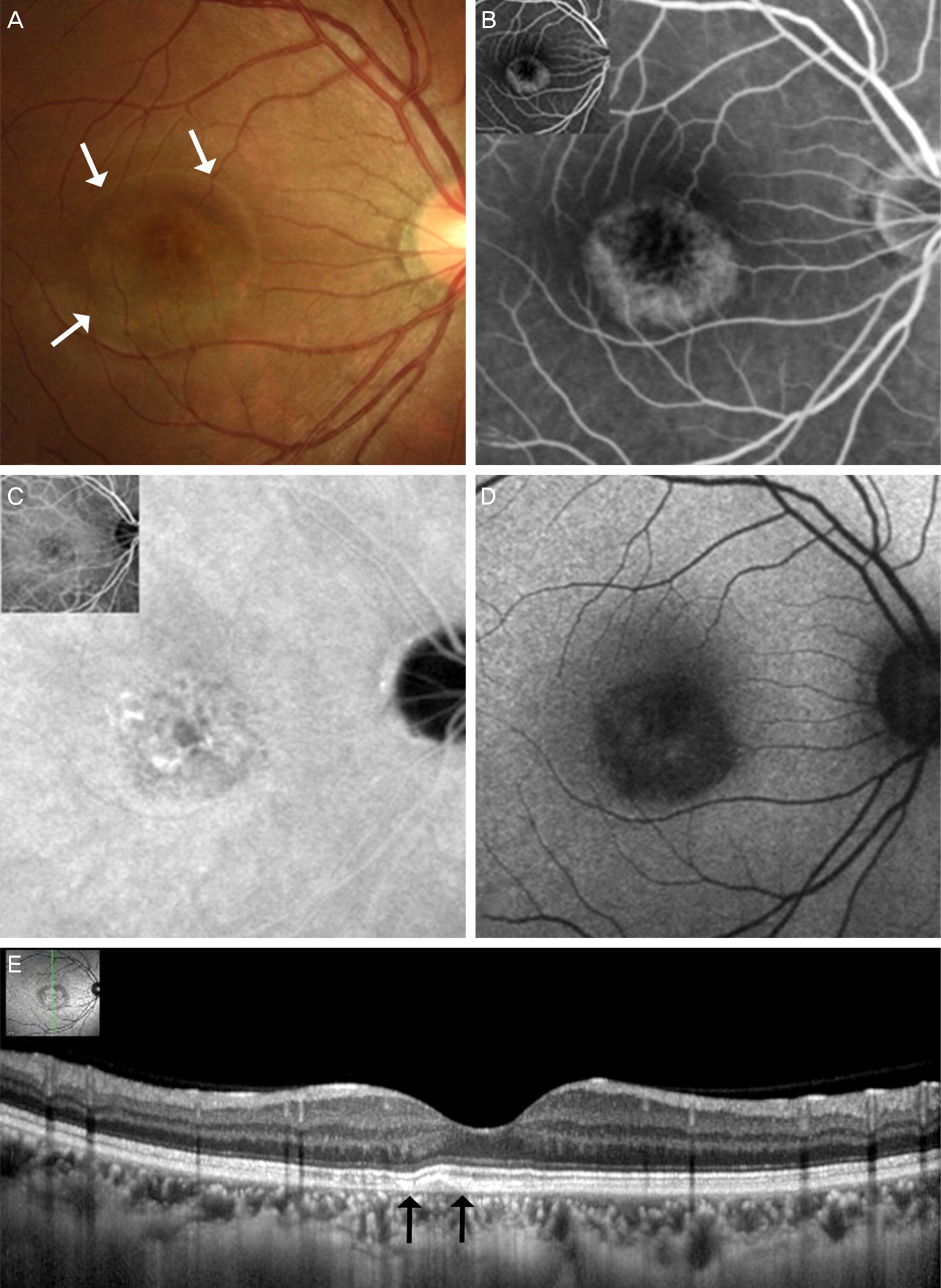
A 32-year-old woman with reduced vision in the right eye had experienced fatigue and flu-like symptoms, including sore throat and fever a few days before. Her best corrected visual acuity (BCVA) was 1.0 in the right eye. There were no cells in the anterior chamber and vitreous. Fundus photographs of the right eye on presentation showed gray-white thickening of the fovea and retinal hemorrhage next to the fovea. Fluorescein angiography demonstrated ring-shaped mottled hyperfluorescence in the early phase and dye pooling in the late phase. Spectral-domain optical coherence tomography (OCT) showed abnormal hyper-reflective thickening at the level of the outer retina and retinal pigment epithelium (RPE) and detachment of the neurosensory retina in the foveal lesion. The inner segment/outer segment junction and photoreceptor elevation/disruption was noted. Nineteen months after onset, the BCVA of the right eye was 1.0 and fundus photographs showed increased retinal pigment hyperplasia, and residual RPE changes resembling a bull's eye maculopathy. The OCT of the right macula showed that the inner segment/outer segment junction elevation/disruption almost completely regressed. The patient was diagnosed with unilateral acute idiopathic maculopathy.
CONCLUSIONS
We report a typical case with flu-like symptoms of unilateral acute idiopathic maculopathy. It is a very rare macular disease and a case such as ours with long-term follow-up using multimodality diagnostic imaging has not been previously reported.
MeSH Terms
Figure
Reference
-
References
1. Yannuzzi LA, Jampol LM, Rabb MF. . Unilateral acute idiopathic maculopathy. Arch Ophthalmol. 1991; 109:1411–6.
Article2. Beck AP, Jampol LM, Glaser DA, Pollack JS. Is coxsackievirus the cause of unilateral acute idiopathic maculopathy? Arch Ophthalmol. 2004; 122:121–3.
Article3. Kim IT, Jang SD. Unilateral idiopathic maculopathy. J Korean Ophthalmol Soc. 1999; 40:1260–8.4. Choi KS, Kim JS. Bilateral acute idiopathic maculopathy. J Korean Ophthalmol Soc. 2000; 41:1626–30.5. Lee SS, Kim EC, Kim YY, Kim SD. Unilateral acute idiopathic maculopathy: A case of atypical presentation. J Korean Ophthalmol Soc. 2000; 41:1796–800.6. de la Fuente MA, Cuadrado R. Unilateral acute idiopathic macul-opathy: angiography, optical coherence tomography and micro-perimetry findings. J Ophthalmic Inflamm Infect. 2011; 1:125–7.
Article7. Jung CS, Payne JF, Bergstrom CS. . Multimodality diagnostic imaging in unilateral acute idiopathic maculopathy. Arch Ophthalmol. 2012; 130:50–6.
Article8. Aggio FB, Farah ME, Meirelles RL, de Souza EC. STRATUSOCT and multifocal ERG in unilateral acute idiopathic maculopathy. Graefes Arch Clin Exp Ophthalmol. 2006; 244:510–6.
Article9. Matsushita E, Fukuda K, Nakahira A. . Resolution of photo-receptor outer segment damage in a patient with unilateral acute idiopathic maculopathy observed using spectral-domain optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2012; 250:765–8.
Article10. Milani P, Cacioppo V, Raimondi G, Scialdone A. Spectral domain OCT and autofluorescence imaging of unilateral acute idiopathic maculopathy. Eur J Ophthalmol. 2012; 22:499–502.
Article11. Ooto S, Hangai M, Yoshimura N. Photoreceptor restoration in unilateral acute idiopathic maculopathy on adaptive optics scanning laser ophthalmoscopy. Arch Ophthalmol. 2011; 129:1633–5.
Article12. Srour M, Querques G, Rostaqui O, Souied EH. Early spectral-do-main optical coherence tomography findings in unilateral acute idiopathic maculopathy. Retina. 2013; 33:2182–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bilateral Acute Idiopathic Maculopathy
- Unilateral Acute Idiopathic Maculopathy: A Case of Atypical Presentation
- Idiopathic Orbital Inflammation Presenting as Unilateral Dacryoadenitis in a Child
- Evaluation of Recurrent or Idiopathic Pancreatitis
- Clinical Analysis on Focal Laser Treatment of Diabetic Maculopathy