J Korean Ophthalmol Soc.
2012 Jan;53(1):87-93. 10.3341/jkos.2012.53.1.87.
Comparison of Choroidal Thickness in Eyes with Central Serous Chorioretinopathy, Asymptomatic Fellow Eyes and Normal Eyes
- Affiliations
-
- 1Department of Ophthalmology, Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. ophkim@hallym.or.kr
- 2Department of Ophthalmology, Hangang Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- KMID: 2215249
- DOI: http://doi.org/10.3341/jkos.2012.53.1.87
Abstract
- PURPOSE
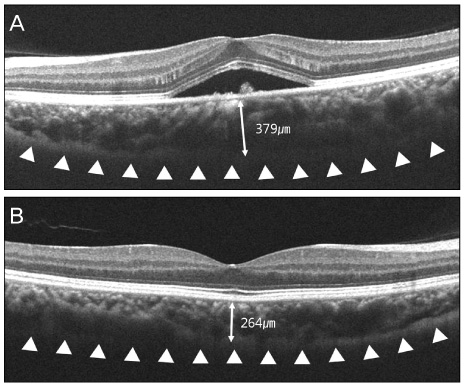
To compare the choroidal thickness in central serous chorioretiopathy (CSC) patients and normal controls using spectral domain optical coherence tomography (SD-OCT).
METHODS
The authors compared the choroidal thickness in eyes with CSC, fellow eyes and in normal eyes. In addition, the authors attempted to determine any correlation between choroidal thickness and other factors such as age, height of serous retinal detachment, and spherical equivalent. Choroidal thickness was measured using a perpendicular line from the outer margin of the subfoveal retinal pigment epithelium to the inner surface of the sclera.
RESULTS
Twenty-five eyes of 25 CSC patients, 17 fellow eyes and 29 age-matched normal eyes were examined and categorized as group 1, group 2 and group 3, respectively. Subfoveal choroidal thickness was 370.64 +/- 58.06 microm in group 1, 301.85 +/- 47.83 microm in group 2, and 261.84 +/- 48.22 microm in group 3. The choroidal thickness in group 1 was significantly greater than those in group 2 and group 3, and the choroidal thickness in group 2 was significantly greater than that in group 3 (p = 0.001, p < 0.001, p = 0.004, respectively), where the choroidal thickness showed a negative correlation with age (p = 0.015).
CONCLUSIONS
The choroidal thickness was greater in eyes with CSC and in their fellow eyes compared to that in normal eyes. The results suggest that CSC may be caused by choroidal vascular hyperpermeability and increased hydrostatic pressure in the choroid.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
The Posterior Choroidal Profiles Measured by Spectral Domain Optical Coherence Tomography in Healthy Korean Children
Jee Hyun Kim, Jin Seon Kim, Kyoo Won Lee, Jung Ho Lee
J Korean Ophthalmol Soc. 2013;54(11):1708-1714. doi: 10.3341/jkos.2013.54.11.1708.Changes in Choroidal Thickness after Panretinal Photocoagulation in Diabetic Retinopathy Patients
Sung Yu, Yong Il Kim, Kyoo Won Lee, Hyun Gu Kang
J Korean Ophthalmol Soc. 2016;57(2):256-263. doi: 10.3341/jkos.2016.57.2.256.
Reference
-
1. Spitznas M. Pathogenesis of central serous retinopathy: a new working hypothesis. Graefes Arch Clin Exp Ophthalmol. 1986. 224:321–324.2. Gass JD. Pathogenesis of disciform detachment of the neuroepithelium. Am J Ophthalmol. 1967. 63:1–139.3. Tittl M, Polska E, Kircher K, et al. Topical fundus pulsation measurement in patients with active central serous chorioretinopathy. Arch Ophthalmol. 2003. 121:975–978.4. Tittl M, Maar N, Polska E, et al. Choroidal hemodynamic changes during isometric exercise in patients with inactive central serous chorioretinopathy. Invest Ophthalmol Vis Sci. 2005. 46:4717–4721.5. Iida T, Kishi S, Hagimura N, Shimizu K. Persistent and bilateral choroidal vascular abnormalities in central serous chorioretinopathy. Retina. 1999. 19:508–512.6. Prünte C, Flammer J. Choroidal capillary and venous congestion in central serous chorioretinopathy. Am J Ophthalmol. 1996. 121:26–34.7. Giovannini A, Scassellati-Sforzolini B, D'Altobrando E, et al. Choroidal findings in the course of idiopathic serous pigment epithelium detachment detected by indocyanine green videoangiography. Retina. 1997. 17:286–293.8. Imamura Y, Fujiwara T, Margolis R, Spaide RF. Enhanced depth imaging optical coherence tomography of the choroid in central serous chorioretinopathy. Retina. 2009. 29:1469–1473.9. Alam S, Zawadzki RJ, Choi S, et al. Clinical application of rapid serial fourier-domain optical coherence tomography for macular imaging. Ophthalmology. 2006. 113:1425–1431.10. Ojima Y, Hangai M, Sasahara M, et al. Three-dimensional imaging of the foveal photoreceptor layer in central serous chorioretinopathy using high-speed optical coherence tomography. Ophthalmology. 2007. 114:2197–2207.11. Spaide RF, Koizumi H, Pozzoni MC. Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol. 2008. 146:496–500.12. Margolis R, Spaide RF. A pilot study of enhanced depth imaging optical coherence tomography of the choroid in normal eyes. Am J Ophthalmol. 2009. 147:811–815.13. Maruko I, Iida T, Sugano Y, et al. Subfoveal choroidal thickness after treatment of central serous chorioretinopathy. Ophthalmology. 2010. 117:1792–1799.14. Manjunath V, Taha M, Fujimoto JG, Duker JS. Choroidal thickness in normal eyes measured using Cirrus HD optical coherence tomography. Am J Ophthalmol. 2010. 150:325–329.15. Chen TC, Cense B, Miller JW, et al. Histologic correlation of in vivo optical coherence tomography images of the human retina. Am J Ophthalmol. 2006. 141:1165–1168.16. Spaide RF. Age-related choroidal atrophy. Am J Ophthalmol. 2009. 147:801–810.17. Spaide RF. Enhanced depth imaging optical coherence tomography of retinal pigment epithelial detachment in age-related macular degeneration. Am J Ophthalmol. 2009. 147:644–652.18. Fujiwara T, Imamura Y, Margolis R, et al. Enhanced depth imaging optical coherence tomography of the choroid in highly myopic eyes. Am J Ophthalmol. 2009. 148:445–450.19. Spaide RF, Hall L, Haas A, et al. Indocyanine green video-angiography of older patients with central serous chorioretinopathy. Retina. 1996. 16:203–213.20. Spaide RF, Campeas L, Haas A, et al. Central serous chorioretinopathy in younger and older adults. Ophthalmology. 1996. 103:2070–2079.21. Gilbert CM, Owens SL, Smith PD, Fine SL. Long-term follow-up of central serous chorioretinopathy. Br J Ophthalmol. 1984. 68:815–820.22. Lu JG, Friberg TR. Idiopathic central serous retinopathy in China: a report of 600 cases (624 eyes) treated by acupuncture. Ophthalmic Surg. 1987. 18:608–611.23. Bujarborua D, Chatterjee S, Choudhury A, et al. Fluorescein angiographic features of asymptomatic eyes in central serous chorioretinopathy. Retina. 2005. 25:422–429.24. Kitzmann AS, Pulido JS, Diehl NN, et al. The incidence of central serous chorioretinopathy in Olmsted County, Minnesota, 1980-2002. Ophthalmology. 2008. 115:169–173.25. Castro-Correia J, Coutinho MF, Rosas V, Maia J. Long-term follow-up of central serous retinopathy in 150 patients. Doc Ophthalmol. 1992. 81:379–386.26. Payne GW, Bearden SE. The microcirculation of skeletal muscle in aging. Microcirculation. 2006. 13:275–277.27. Muller-Delp JM. Aging-induced adaptations of microvascular reactivity. Microcirculation. 2006. 13:301–314.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Subfoveal Choroidal Thickness in Fellow Eyes of Patients with Central Serous Chorioretinopathy
- Spectral Domain OCT Findings of Asymptomatic Fellow Eyes in Central Serous Chorioretinopathy
- The Color Vision Test in Acute Central Serous Chorioretinopathy
- Multifocal Electroretinogram Abnormalities of Central Serous Chorioretinopathy
- Chroidal Circulation in Central Serous Chorioretinopathy using Indocyanine Green Angiography