J Korean Ophthalmol Soc.
2011 Mar;52(3):378-384. 10.3341/jkos.2011.52.3.378.
Visual Field Defect Developed after Internal Limiting Membrane Peeling in a Patient with Epiretinal Membrane
- Affiliations
-
- 1Department of Ophthalmology, Pusan National University School of Medicine, Busan, Korea. alertlee@hanmail.net
- KMID: 2214306
- DOI: http://doi.org/10.3341/jkos.2011.52.3.378
Abstract
- PURPOSE
To report a case of visual field defect developed after internal limiting membrane (ILM) peeling in a patient with macular epiretinal membrane (ERM).
CASE SUMMARY
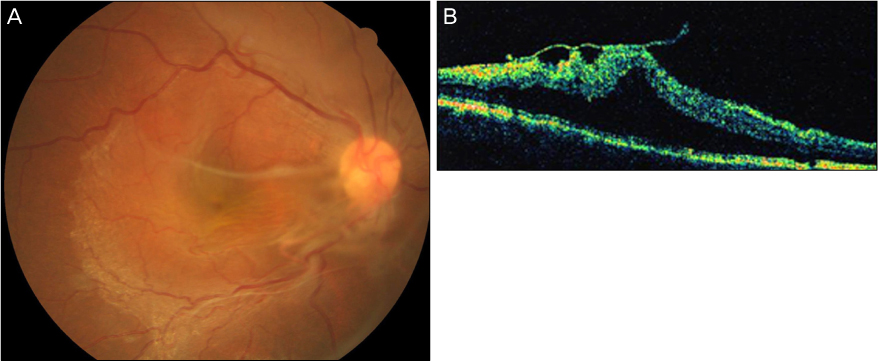
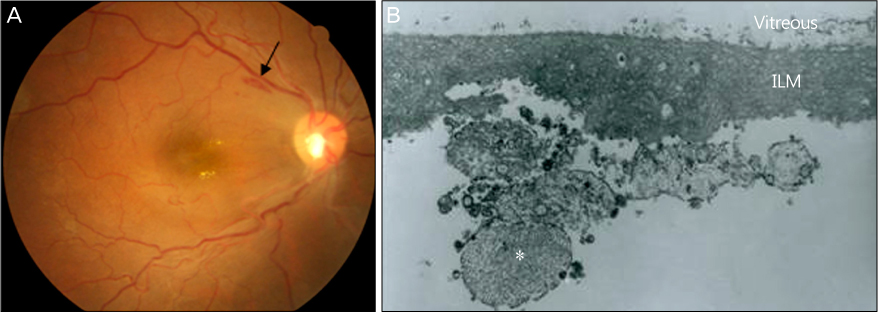
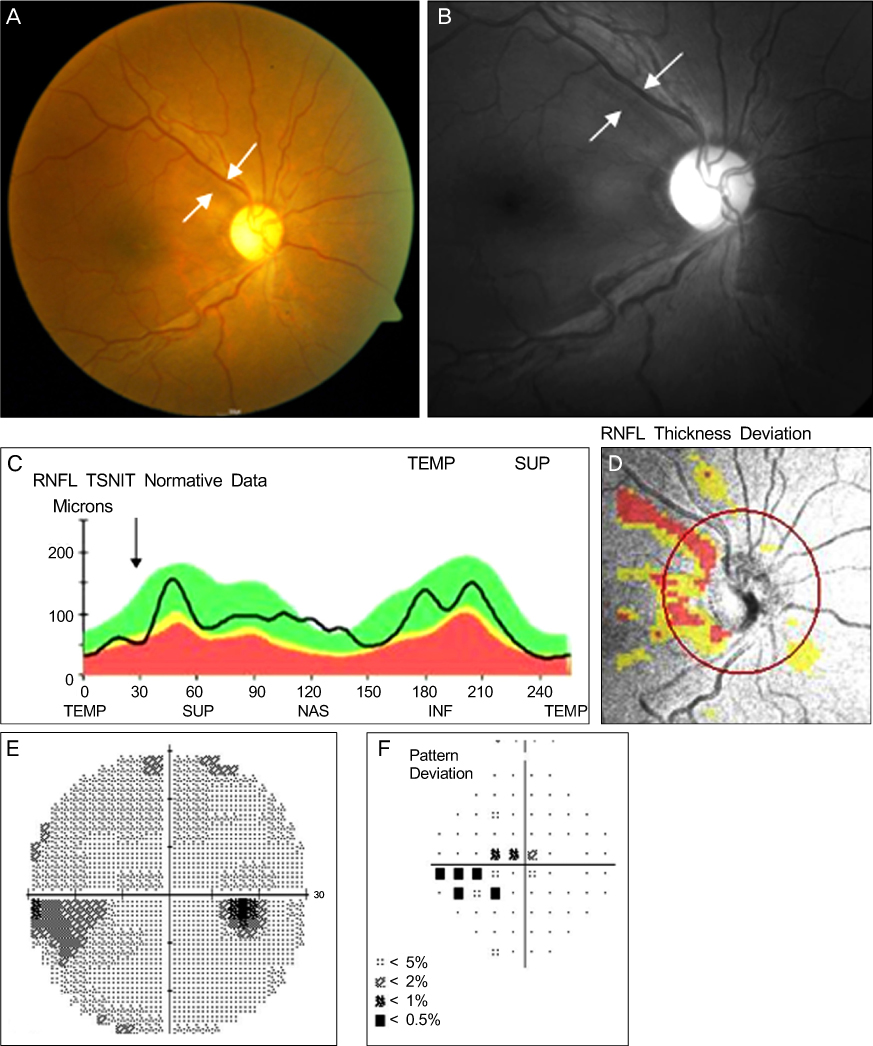
A 33-year-old female without a history of specific diseases presented with a gradually decreased visual acuity in the right eye for 3 years. The patient was diagnosed as having macular ERM and underwent vitrectomy. During ILM peeling, retinal hemorrhage occurred in the superior region of macula, which spontaneously disappeared 2 weeks after surgery. Transmission electron microscopy showed Muller cell end feet with damaged appearance adherent to the ILM. At 3 months after surgery, the patient developed retinal nerve fiber layer (RNFL) defect in the area where the spot retinal hemorrhage had occurred. Optical coherence tomography showed focal RNFL thinning in the superotemporal region. The automated perimetry revealed corresponding inferior nasal step and scotomas in the right eye. Intraocular pressure was normal throughout the follow-up period and there was no evidence of glaucomatous optic disc change.
CONCLUSIONS
The results obtained from the patient in the present study indicated that visual field defect may be the result of a mechanical damage to the RNFL during ILM peeling.
MeSH Terms
Figure
Cited by 1 articles
-
Visual Field Changes after Internal Limiting Membrane Peeling in Glaucoma Patients with Epiretinal Membrane
Han Seok Park, Seong Jung Ha, Jae Hong Ahn
J Korean Ophthalmol Soc. 2019;60(10):966-974. doi: 10.3341/jkos.2019.60.10.966.
Reference
-
1. Ting FS, Kwok AK. Treatment of epiretinal membrane: an update. Hong Kong Med J. 2005. 11:496–502.2. Pesin SR, Olk RJ, Grand MG, et al. Vitrectomy for premacular fibroplasia. Prognostic factors, long-term follow-up, and time course of visual improvement. Ophthalmology. 1991. 98:1109–1114.3. Kwok AKh, Lai TY, Yuen KS. Epiretinal membrane surgery with or without internal limiting membrane peeling. Clin Experiment Ophthalmol. 2005. 33:379–385.4. Park DW, Dugel PU, Garda J, et al. Macular pucker removal with and without internal limiting membrane peeling: pilot study. Ophthalmology. 2003. 110:62–64.5. Kwok AK, Lai TY, Li WW, et al. Indocyanine green-assisted internal limiting membrane removal in epiretinal membrane surgery: a clinical and histologic study. Am J Ophthalmol. 2004. 138:194–199.6. FINE BS. Limiting membranes of the sensory retina and pigment epithelium. An electron microscopic study. Arch Ophthalmol. 1961. 66:847–860.7. Wolf S, Schnurbusch U, Wiedemann P, et al. Peeling of the basal membrane in the human retina: ultrastructural effects. Ophthalmology. 2004. 111:238–243.8. Koo GH, Lee JE, Choi HY, Oum BS. Ultrastructure of the internal limiting membrane removed during macular hole and diabetic macular edema surgery. J Korean Ophthalmol Soc. 2010. 51:42–48.9. Terasaki H, Miyake Y, Nomura R, et al. Focal macular ERGs in eyes after removal of macular ILM during macular hole surgery. Invest Ophthalmol Vis Sci. 2001. 42:229–234.10. Uemoto R, Yamamoto S, Aoki T, et al. Macular configuration determined by optical coherence tomography after idiopathic macular hole surgery with or without internal limiting membrane peeling. Br J Ophthalmol. 2002. 86:1240–1242.11. Holländer H, Makarov F, Dreher Z, et al. Structure of the macroglia of the retina: sharing and division of labour between astrocytes and Müller cells. J Comp Neurol. 1991. 313:587–603.12. Gandorfer A, Haritoglou C, Gass CA, et al. Indocyanine green-assisted peeling of the internal limiting membrane may cause retinal damage. Am J Ophthalmol. 2001. 132:431–433.13. Tadayoni R, Paques M, Massin P, et al. Dissociated optic nerve fiber layer appearance of the fundus after idiopathic epiretinal membrane removal. Ophthalmology. 2001. 108:2279–2283.14. Mitamura Y, Ohtsuka K. Relationship of dissociated optic nerve fiber layer appearance to internal limiting membrane peeling. Ophthalmology. 2005. 112:1766–1770.15. Ito Y, Terasaki H, Takahashi A, et al. Dissociated optic nerve fiber layer appearance after internal limiting membrane peeling for idiopathic macular holes. Ophthalmology. 2005. 112:1415–1420.16. Haritoglou C, Gass CA, Schaumberger M, et al. Macular changes after peeling of the internal limiting membrane in macular hole surgery. Am J Ophthalmol. 2001. 132:363–368.17. Haritoglou C, Ehrt O, Gass CA, et al. Paracentral scotomata: a new finding after vitrectomy for idiopathic macular hole. Br J Ophthalmol. 2001. 85:231–233.18. Uemura A, Kanda S, Sakamoto Y, Kita H. Visual field defects after uneventful vitrectomy for epiretinal membrane with indocyanine green-assisted internal limiting membrane peeling. Am J Ophthalmol. 2003. 136:252–257.19. Pendergast SD, McCuen BW 2nd. Visual field loss after macular hole surgery. Ophthalmology. 1996. 103:1069–1077.20. Paques M, Massin P, Santiago PY, et al. Visual field loss after vitrectomy for full-thickness macular holes. Am J Ophthalmol. 1997. 124:88–94.21. Hutton WL, Fuller DG, Snyder WB, et al. Visual field defects after macular hole surgery. A new finding. Ophthalmology. 1996. 103:2152–2158.22. Boldt HC, Munden PM, Folk JC, Mehaffey MG. Visual field defects after macular hole surgery. Am J Ophthalmol. 1996. 122:371–381.23. Russell SR, Hageman GS. Optic disc, foveal, and extrafoveal damage due to surgical separation of the vitreous. Arch Ophthalmol. 2001. 119:1653–1658.24. Kim CY, Lee JH, Lee SJ, et al. Visual field defect caused by nerve fiber layer damage associated with an internal limiting lamina defect after uneventful epiretinal membrane surgery. Am J Ophthalmol. 2002. 133:569–571.25. Melberg NS, Thomas MA. Visual field loss after pars plana vitrectomy with air/fluid exchange. Am J Ophthalmol. 1995. 120:386–388.26. Welch JC. Dehydration injury as a possible cause of visual field defect after pars plana vitrectomy for macular hole. Am J Ophthalmol. 1997. 124:698–699.27. Yamashita T, Uemura A, Kita H, Sakamoto T. Analysis of the retinal nerve fiber layer after indocyanine green-assisted vitrectomy for idiopathic macular holes. Ophthalmology. 2006. 113:280–284.28. Lee JW, Kim IT. Outcomes of idiopathic macular epiretinal membrane removal with and without internal limiting membrane peeling: a comparative study. Jpn J Ophthalmol. 2010. 54:129–134.29. Miura M, Elsner AE, Osako M, et al. Dissociated optic nerve fiber layer appearance after internal limiting membrane peeling for idiopathic macular hole. Retina. 2003. 23:561–563.30. Harris A, Bingaman D, Ciulla T, Martin B. Ryan SJ, editor. Retinal and choroidal blood flow in health and disease. Reting. 2006. 4th ed. Los Angeles: Elsvier Mosby;v.1. chap. 5.31. Yamada E. Some structural features of the fovea centralis in the human retina. Arch Ophthalmol. 1969. 82:151–159.32. Gass JD. Müller cell cone, an overlooked part of the anatomy of the fovea centralis: hypotheses concerning its role in the pathogenesis of macular hole and foveomacualr retinoschisis. Arch Ophthalmol. 1999. 117:821–823.33. Sivalingam A, Eagle RC Jr, Duker JS, et al. Visual prognosis correlated with the presence of internal-limiting membrane in histopathologic specimens obtained from epiretinal membrane surgery. Ophthalmology. 1990. 97:1549–1552.34. Iriyama A, Uchida S, Yanagi Y, et al. Effects of indocyanine green on retinal ganglion cells. Invest Ophthalmol Vis Sci. 2004. 45:943–947.35. Paques M, Genevois O, Régnier A, et al. Axon-tracing properties of indocyanine green. Arch Ophthalmol. 2003. 121:367–370.36. Yip HK, Lai TY, So KF, Kwok AK. Retinal ganglion cells toxicity caused by photosensitising effects of intravitreal indocyanine green with illumination in rat eyes. Br J Ophthalmol. 2006. 90:99–102.37. Maia M, Haller JA, Pieramici DJ, et al. Retinal pigment epithelial abnormalities after internal limiting membrane peeling guided by indocyanine green staining. Retina. 2004. 24:157–160.38. Poliner LS, Tornambe PE. Retinal pigment epitheliopathy after macular hole surgery. Ophthalmology. 1992. 99:1671–1677.39. Michels M, Lewis H, Abrams GW, et al. Macular phototoxicity caused by fiberoptic endoillumination during pars plana vitrectomy. Am J Ophthalmol. 1992. 114:287–296.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Visual Field Changes after Internal Limiting Membrane Peeling in Glaucoma Patients with Epiretinal Membrane
- The Effect of Internal Limiting Membrane Peeling in Treatment of Idiopathic Epiretinal Membrane
- Internal Limiting Membrane Peeling In Surgical Treatment of Macular Epiretinal Membrane
- The Effect of Internal Limiting Membrane Peeling in Epiretinal Membrane Including Pseudolamellar Macular Hole
- Macular Hole Surgery with or without Indocyanine Green-Assisted Internal Limiting Membrane Peeling