J Korean Ophthalmol Soc.
2007 Aug;48(8):1067-1072.
The Effect of Internal Limiting Membrane Peeling in Treatment of Idiopathic Epiretinal Membrane
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Dongsan Medical Center, Keimyung University, Daegu, Korea. kimks@dsmc.or.kr
Abstract
-
PURPOSE: This study was designed to evaluate the effect of internal limiting membrane (ILM) peeling in the surgical management of idiopathic macular epiretinal membrane (ERM).
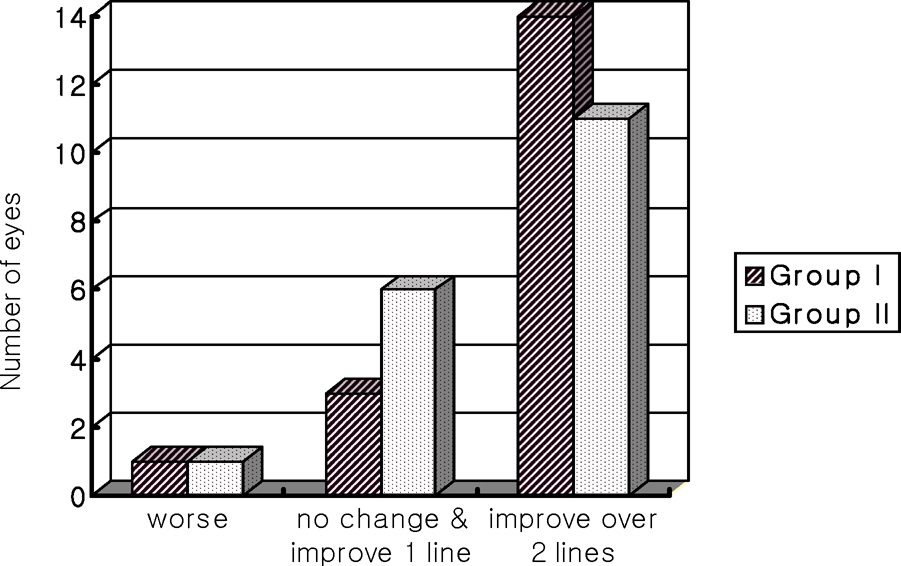
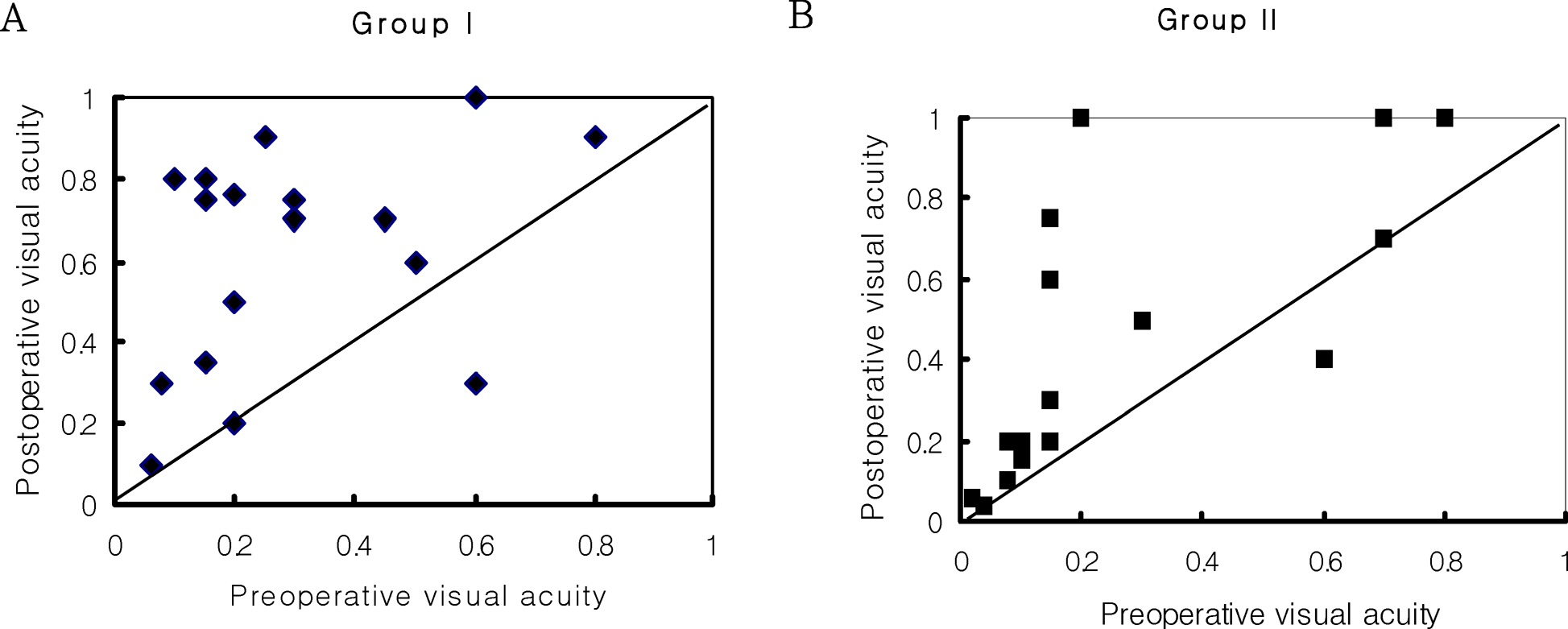
METHOD: The records of 36 patients (36 eyes) with idiopathic macular ERM who had undergone pars plana vitrectomy with removal of the ERM were retrospectively reviewed. The patients were divided into two groups: eyes with (18 eyes) or without (18 eyes) ILM peeling. The best corrected visual acuity (BCVA), recurrence of ERM, persistence of retinal wrinkling, as well as the complications and improvement of visual acuity of the two groups were compared.
RESULTS
The mean pre-operative BCVA for the two groups was 0.29 in the group with ILM peeling and 0.26 in the group without ILM peeling, while the mean post-operative BCVA was 0.59 and 0.50, respectively. Although the post-operative BCVA significantly improved in both groups (P=0.001), there was no statistically significant difference between the two groups (P>0.05). However, the persistence of retinal wrinkling greatly decreased in the group with ILM peeling, and ERM recurred in two cases in the group without ILM peeling.
Conclusion
ILM peeling in the surgical management of idiopathic macular ERM does not affect the postoperative results of visual acuity and complications, except for the persistence of retinal wrinkling and recurrence.
MeSH Terms
Figure
Reference
-
References
1. Mitchell P, Smith W, Chey T, et al. Prevalence and associations of epiretinal membranes. The Blue Mountains Eye Study, Australia. Opthalmology. 1997; 104:1033–40.2. Poliner LS, Olk RJ, Grand MG, et al. Surgical management of pre-macular fibroplasia. Arch Ophthalmol. 1988; 106:761–5.
Article3. de Bustros S, Thompson JT, Michels RG, et al. Vitrectomy for idiopathic epiretinal membranes causing macular pucker. Br J Ophthalmol. 1988; 72:692–5.
Article4. de Bustros S, Rice TA, Michels RG, et al. Vitrectomy for macular pucker: use after treatment of retinal tears or retinal detachment. Arch Ophthalmol. 1998; 106:758–60.5. Pesin SR, Olk RJ, Grand MG, et al. Vitrectomy for premacular fibroplasia: prognostic factors, long-term follow-up, and time course of visual improvement. Ophthalmology. 1991; 98:1109–14.6. Grewing R, Mester U. Results of surgery for epiretinal membranes and their recurrences. Br J Ophthlmol. 1996; 80:323–6.
Article7. Donati G, Kapetanios AD, Pournaras CJ. Complications of surgery for epiretinal membranes. Graefes Arch Clin Exp Ophthalmol. 1998; 236:739–46.
Article8. Kim TW, Song SJ, Chung H, et al. Internal limiting membrane peeling in surgical treatment of macular epiretinal membrane. J Korean Ophthalmol Soc. 2005; 46:989–94.9. Wilkinson CP. Recurrent macular pucker. Am J Ophthalmol. 1979; 88:1029–31.
Article10. Kwok AK, Lai TY, Li WW, et al. Indocyanine green-assisted internal limiting membraned removal in epiretinal membrane surgery: a clinical and histologic study. Am J Ophthalmol. 2004; 138:194–9.11. Sorcinelli R. Surgical management of epiretinal membrane with indocyanine-green-assisted peeling. Ophthalmologica. 2003; 217:107–10.
Article12. Park DW, Dugel PU, Garda J, et al. Macular pucker removal with and without internal limiting membrane peeling: pilot study. Ophthalmology. 2003; 110:62–4.
Article13. Shea M. The surgical management of macular pucker in rhegmatogenous retinal detachment. Ophthalmology. 1980; 87:70–4.
Article14. Maia M, Haller JA, Pieramici DJ, et al. Retinal pigment epithelial abnormalities after internal limiting membrane peeling guided by indocyanine green staining. Retina. 2004; 24:157–60.
Article15. Sivalingam A, Eagle RC Jr, Duker JS, et al. Visual prognosis correlated with the presence of internal - limiting membrane in histopathologic specimens obtained from epiretinal membrane surgery. Ophthalmology. 1990; 97:1549–52.16. Haritoglou C, Gandorfer A, Gass CA, et al. The effect of indocyanine-green on functional out come of macular pucker surgery. Am J Ophthalmol. 2003; 135:328–37.17. Wilkins JR, Puliafito CA, Hee MR, et al. Characteristics of epiretinal membranes using optical coherence tomography. Ophthalmology. 1996; 103:2142–51.18. Mori K, Gehlbach PL, Sano A, et al. Comparison of epiretinal membranes of differing pathogenesis using optical coherence tomography. Retina. 2004; 24:57–62.
Article19. Gass JDM. Stereoscopic Atlas of Macular disease, Diagnosis and Treatment. 3rd ed.2. St. Louis: Mosby;1987. p. 676–93.20. Kim NJ, Chung H, Heo JW. Factors associated with recurrence after surgery for epiretinal membrane. J Korean Ophthalmol Soc. 2003; 44:825–9.21. Vinores SA, Campochiaro PA, Conway BP. Ultrastructural and electron immunocyto-chemical characterization of cells in epiretinal membranes. Invest Ophthalmo Vis Sci. 1990; 31:14–28.22. Foos RY. Vitreoretinal juncture-Simple epiretinal membranes. Graefes Arch Clin Exp Ophthalmol. 1974; 189:231–50.23. Bellhorn MB, Freidman AH, Wise GN, Henkind P. Ultrastructral and clinicopathologic correlation of idiopathic preretinal macular fibrosis. Am J Ophthalmol. 1974; 79:366–73.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Internal Limiting Membrane Peeling In Surgical Treatment of Macular Epiretinal Membrane
- Tomographic Structural Changes of the Inner Retina after Internal Limiting Membrane Peeling for Idiopathic Epiretinal Membrane
- Effects of Internal Limiting Membrane Peeling in Combined Hamartoma of Retina and Retinal Pigment Epithelium
- Clinical Outcomes of Indocyanine Green-Assisted Peeling of the Internal Limiting Membrane in Epiretinal Membrane Surgery
- Analysis of the Maular Change in Optical Coherent Tomography after Internal Limiting Membrane Peeling