J Korean Ophthalmol Soc.
2010 Feb;51(2):297-302. 10.3341/jkos.2010.51.2.297.
A Case of Primary Intraocular Lymphoma Confirmed by Endoretinal Biopsy
- Affiliations
-
- 1Department of Ophthalmology, Catholic University of Daegu College of Medicine, Daegu, Korea. yykim@cu.ac.kr
- KMID: 2213156
- DOI: http://doi.org/10.3341/jkos.2010.51.2.297
Abstract
- PURPOSE
To report one case of primary intraocular lymphoma confirmed by endoretinal biopsy and clinical experience.
CASE SUMMARY
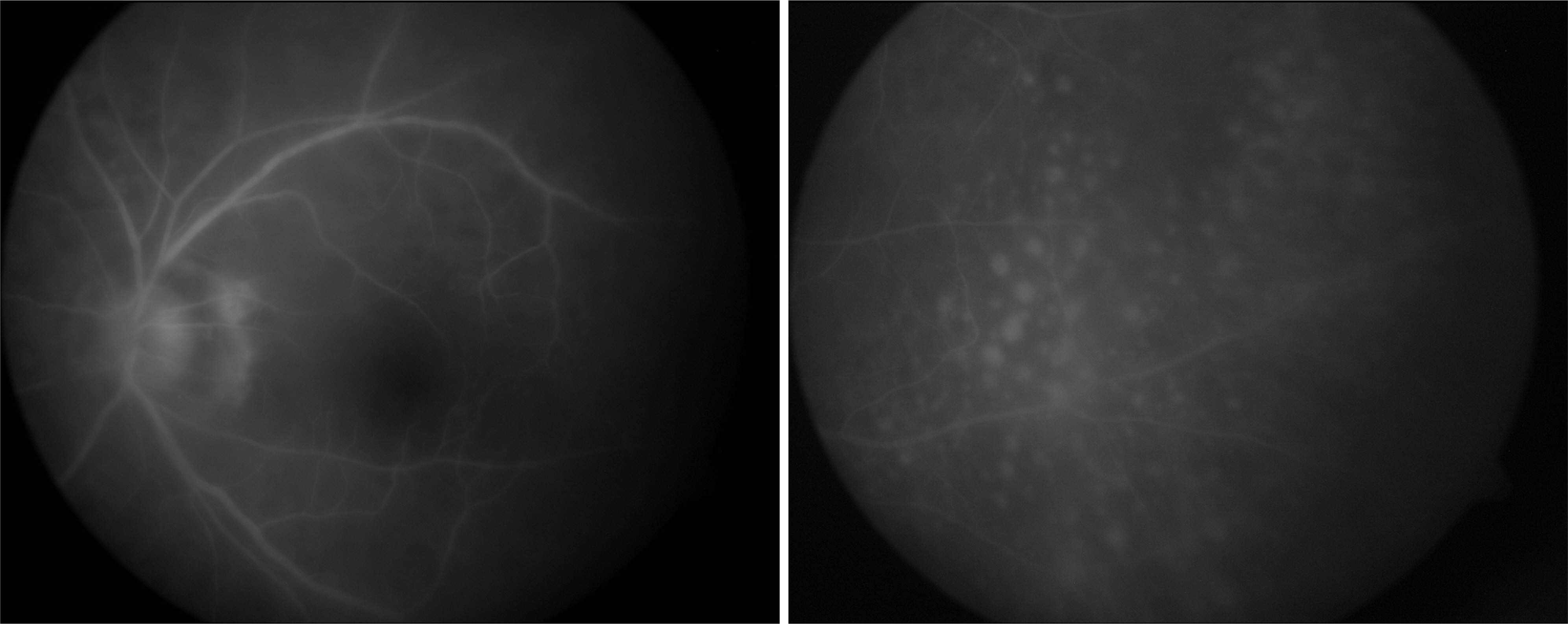
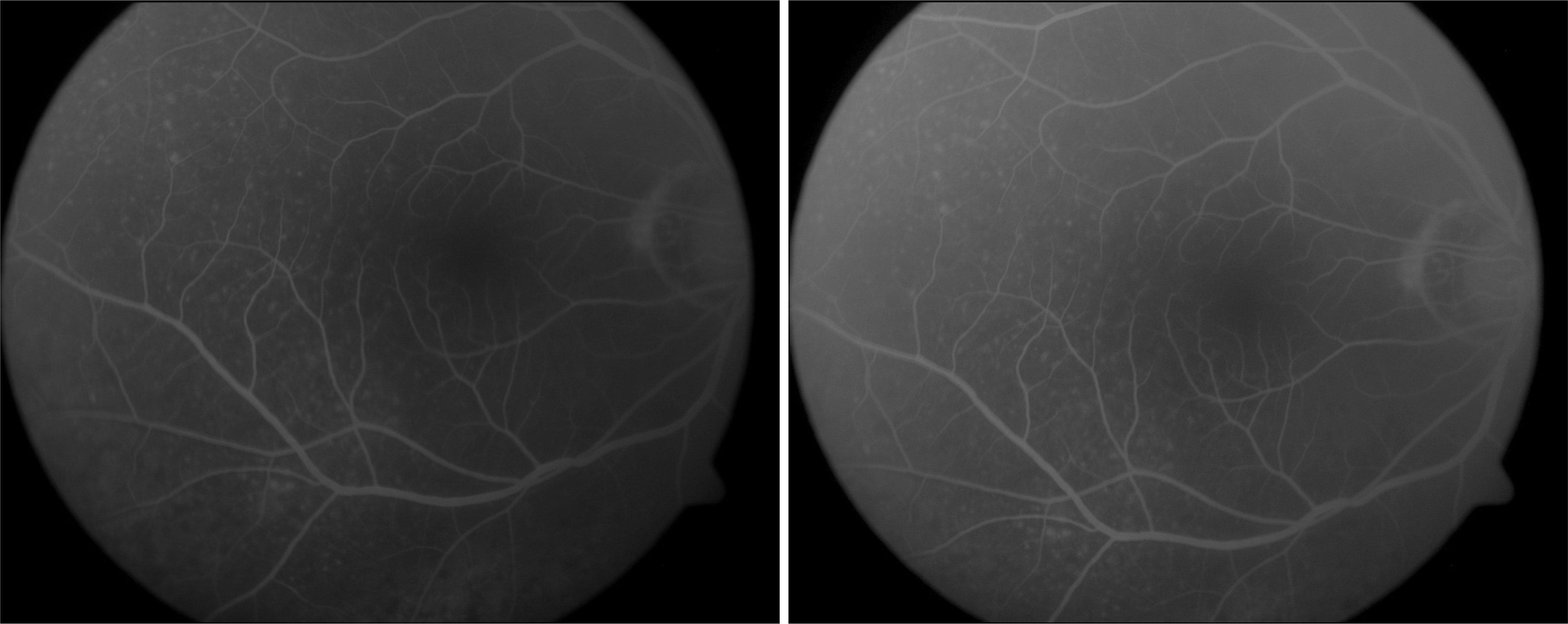
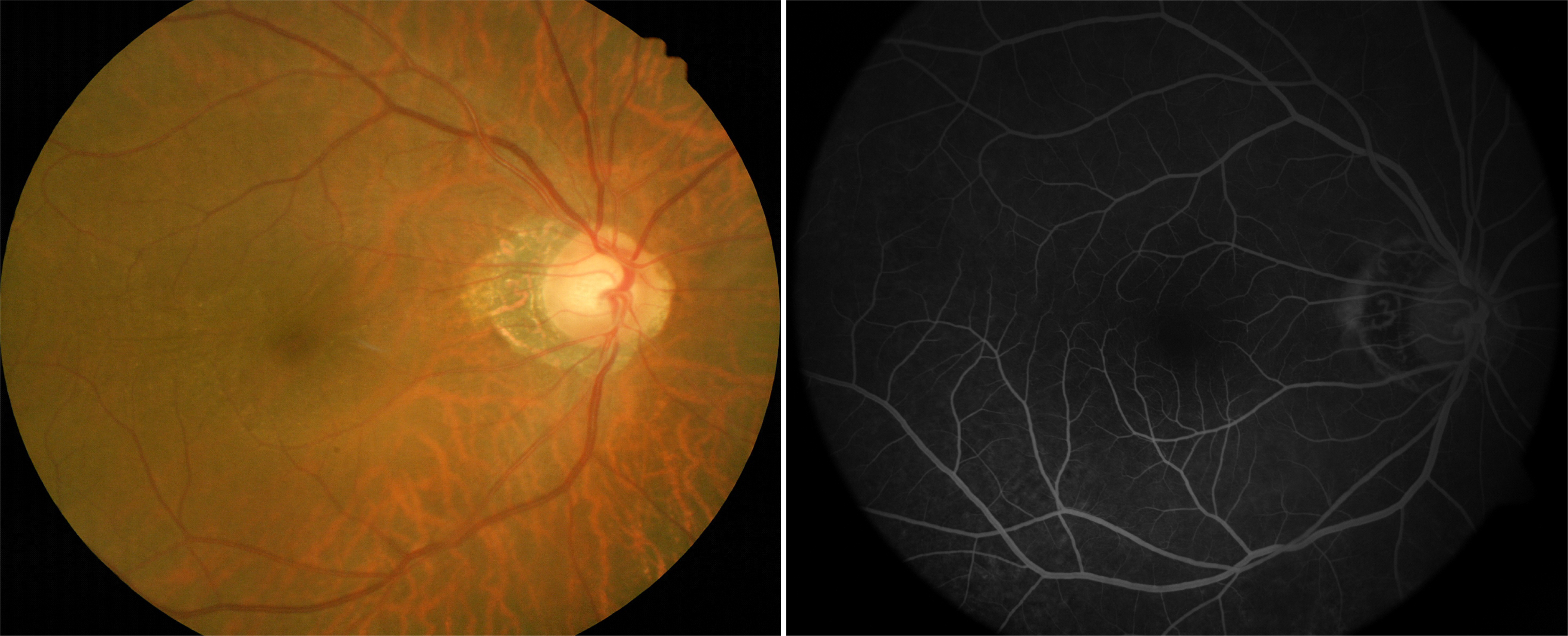
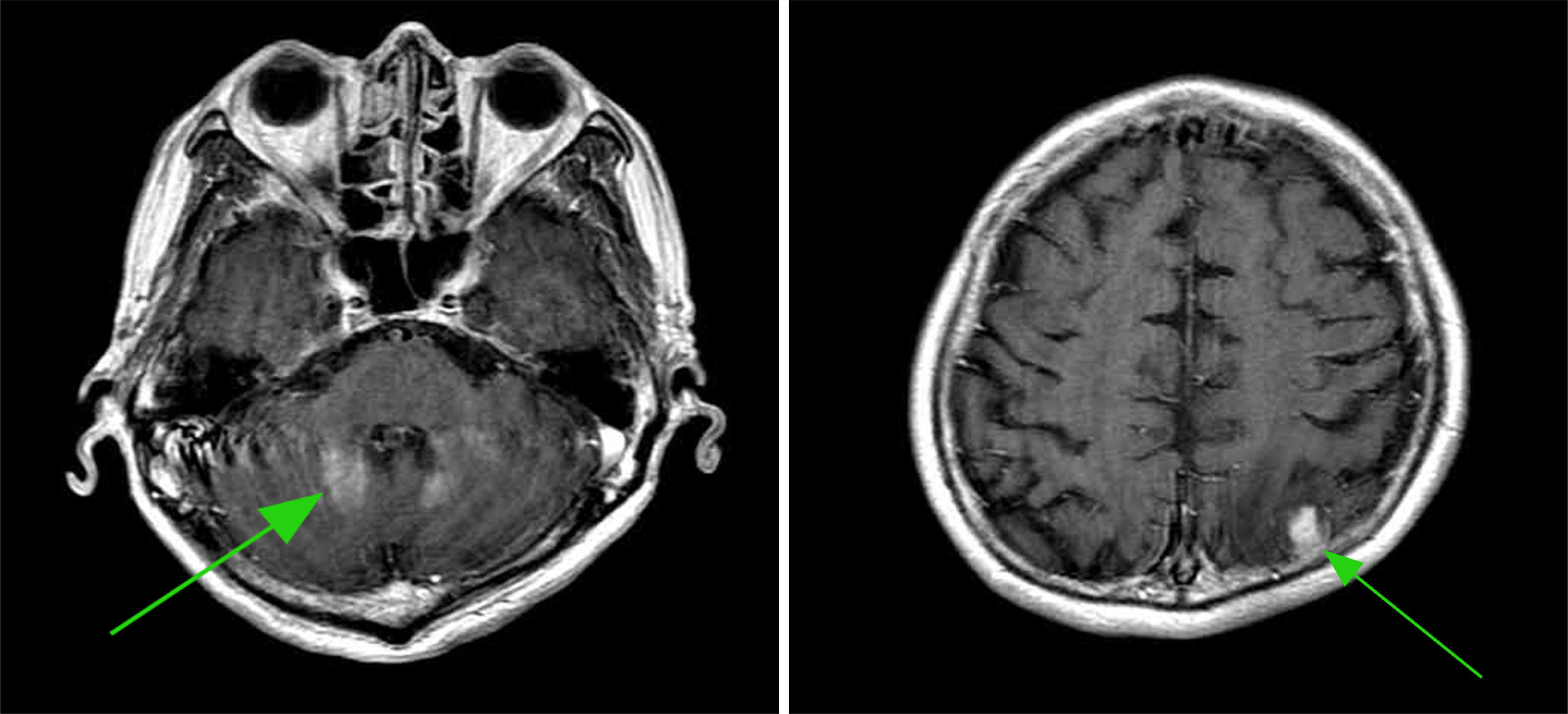
A 65 year-old man complaining of persistent decreased visual acuity was referred to our hospital. Biomicroscopic examination showed bilateral vitreous cells and small round yellowish inflammatory lesions at the level of the retinal pigment epithelial cells. The disc of the left eye was pale in color. Fluorescein angiographic examination of the left eye showed intermingling round hyperfluorescent and hypofluorescent lesions. We performed diagnostic vitrectomy due to unresponsiveness to oral steroid therapy, but the result was negative. We finally performed an endoretinal biopsy, which showed tumor cells with H&E staining and strong immunoreactivities against CD 20 and CD 79a indicating the presence of B cells. We diagnosed this case as primary intraocular lymphoma and performed multiple-cycle chemotherapy with high-dose methotrexate. The ocular signs and symptoms were improved after chemotherapy.
CONCLUSIONS
Endoretinal biopsy could be another diagnostic tool for confirming suspected primary intraocular lymphoma in cases showing negative results with diagnostic pars plana vitrectomy and cytology.
MeSH Terms
Figure
Cited by 1 articles
-
Presumed Intraocular Natural Killer/T-cell Lymphoma Combined with Nasal Lymphoma
Hoon Seok Jeong, Sang Hui Park, Jae Hoon Lee, Dae Yeong Lee, Dong Heun Nam
J Korean Ophthalmol Soc. 2011;52(7):871-875. doi: 10.3341/jkos.2011.52.7.871.
Reference
-
References
1. Coupland SE, Heimann H, Bechrakis NE. Primary intraocular lymphoma: a review of the clinical, histopathological and molecular biological features. Graefes Arch Clni Exp Ophthalomol. 2004; 242:901–13.
Article2. Lobo A, Lightman S. Vitreous aspiration needle tap in the diagnosis of intraocular inflammation. Ophthalmolology. 2003; 110:595–9.
Article3. Kirmani MH, Thomas EL, Rao NA, Laborde RP. Intraocular re-ticulum cell sarcoma: diagnosis by choroidal biopsy. Br J aberrations. 1987; 71:748–52.
Article4. Gil MK, Jampol LM. Variations in the presentation of primary intraocular lymphoma: Case reports and a review. Surv Ophthalmol. 2001; 45:463–71.5. Buggage RR, Chan CC, Nussenblatt RB. Ocular manifestations of central nervous system lymphoma. Curr Opin Oncol. 2001; 13:137–42.
Article6. Suh HS, Yu HG. Clinical manifestations of intraocular lymphoma. J Korean Ophthalmol Soc. 2009; 50:78–84.
Article7. Coupland SE, Bechrakis NE, Anastassiou G, et al. Evaluation of vitrectomy specimens and chorioretinal biopsies in the diagnosis of primary intraocualr lymphoma in patients with masquerade syndrome. Graefes Arch Clin Exp Ophthalmol. 2003; 241:860–70.8. Peterson K, Gordon KB, Heinemann MH, DeAngelis LM. The clinical spectrum of ocular lymphoma. Cancer. 1993; 72:843–9.
Article9. Chan CC, Gonzales JA. Diagnostic approaches. Chan CC, Gonzales JA, editors. Primary ocular lymphoma. 1st ed.Singapore: World scientific publishing co;2007. 1:chap.p. 19.10. Peyman GA, Juarez CP, Raichand M. Full thickness eye wall biopsy: long term results in 9 patients. Br J Ophthalmol. 1981; 65:723–6.11. Cassoux N, Charlotte F, Rao NA, et al. Endoretinal biopsy in establishing the diagnosis of uveitis: a clinicopathologic report of three cases. Ocul Immunol Inflamm. 2005; 13:79–83.12. Johnston RL, Tufail A, Lightman S, et al. Retinal and choroidal biopsy are helpful in unclear uveitis of suspected infections or malignant origin. Ophthalmology. 2004; 111:522–8.13. Martin DF, Chan CC, de Smet MD, et al. The role of chorioretinal biopsy in the management of posterior uveitis. aberrationsogy. 1993; 100:705–14.14. Basso U, Brandes AA. Diagnostic advances and new trends for the treatment of primary central nervous system lymphoma. Eur J Cancer. 2002; 38:1298–312.
Article15. Bachelor TT, Kolak G, Ciordia R, et al. High dose methotrexate for intraocular lymphoma. Clin Cancer Res. 2003; 9:711–5.