J Korean Ophthalmol Soc.
2016 May;57(5):853-856. 10.3341/jkos.2016.57.5.853.
A Case of Failed Macular Hole Closure Associated with an Entrapped Microbubble in the Hole
- Affiliations
-
- 1Department of Ophthalmology, Dongguk University College of Medicine, Gyeongju, Korea. jazzhanul@hanmail.net
- KMID: 2212732
- DOI: http://doi.org/10.3341/jkos.2016.57.5.853
Abstract
- PURPOSE
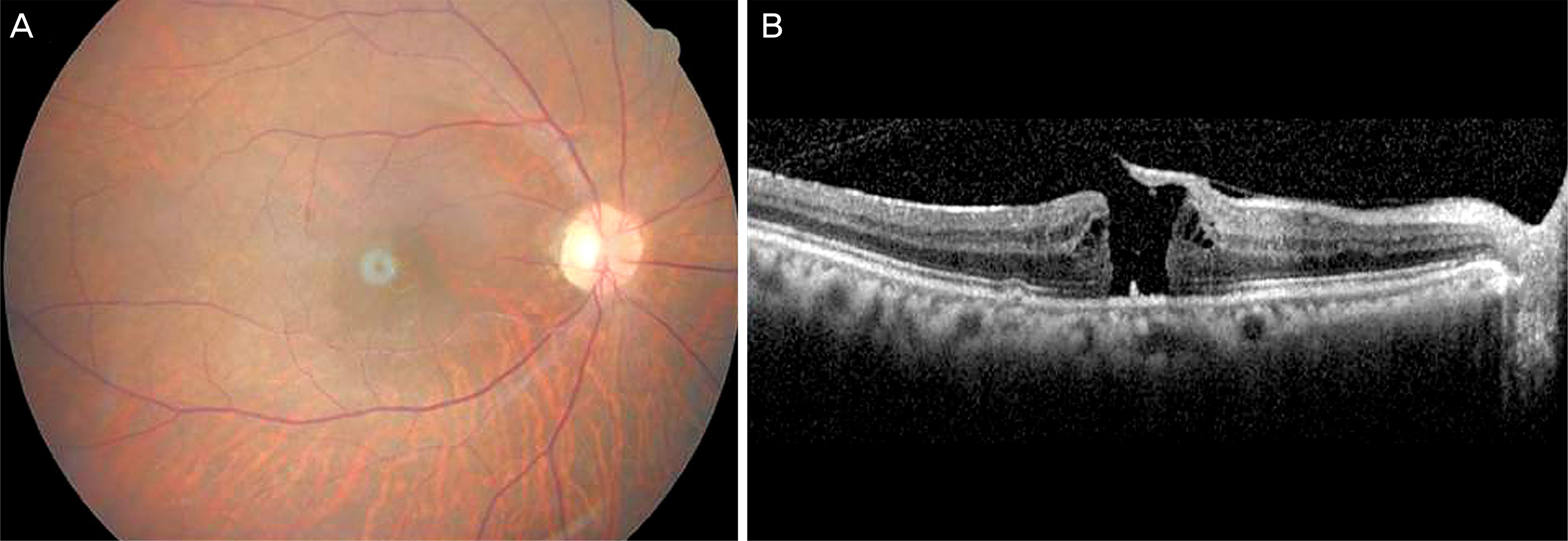
To report a case of failed sealing of full-thickness macular hole associated with an entrapped microbubble in the hole after vitrectomy, peeling of the internal limiting membrane and C3F8 (14%) gas injection.
CASE SUMMARY
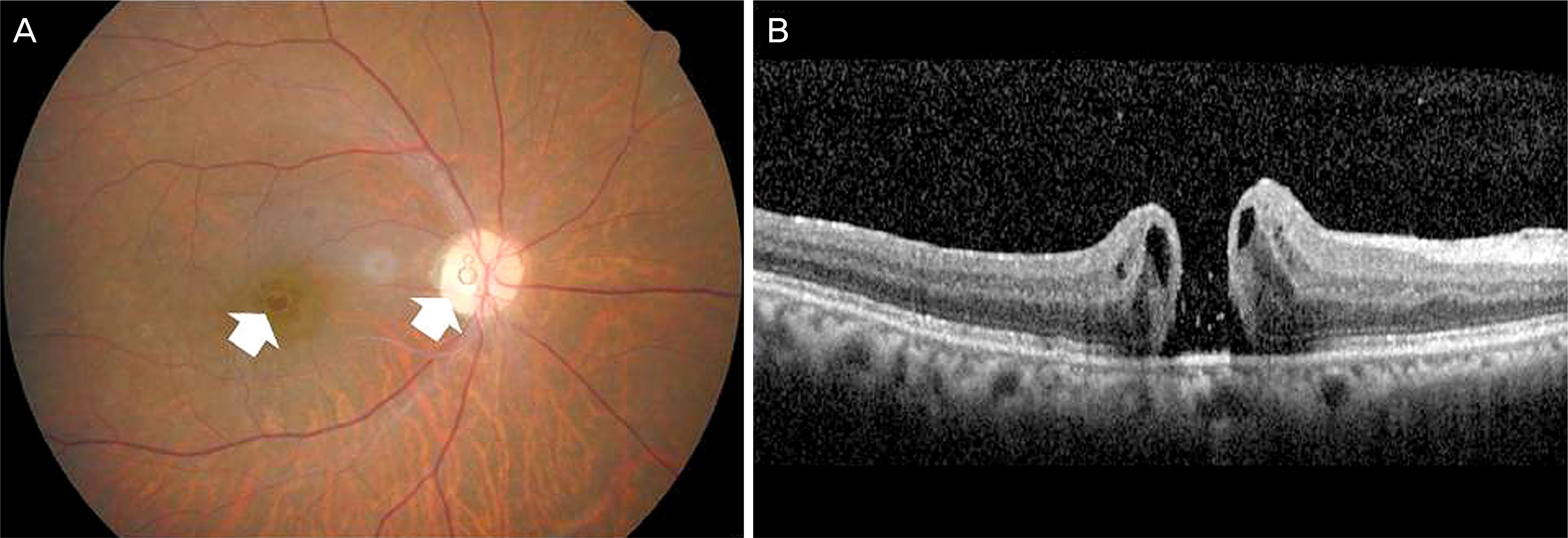
A 69-year-old female visited our clinic for decreased visual acuity in her right eye. The best corrected visual acuity (BCVA) was 20/200 in the right eye. The fundoscopy and spectral domain optical coherence tomography (SD-OCT) showed a full-thickness macular hole. She had a history of spine surgery and, thus was unable to maintain a prone position after surgery. The patient underwent pars plana vitrectomy, peeling of the internal limiting membrane and C3F8 (14%) gas injection in a sitting position postoperatively. Three weeks postoperatively, fundoscopy showed an entrapped microbubble within the macular hole, which was not sealed as observed on SD-OCT. We thought the entrapped microbubble within the macular hole prevented closure of the hole and removed it during the repeated surgery. At 2 weeks after the microbubble removal, fundoscopy and SD-OCT in the right eye showed the closure of the macular hole and the BCVA was improved to 20/40.
CONCLUSIONS
We experienced a failed sealing of full-thickness macular hole due to an entrapped microbubble within the hole after macular hole surgery and observed the closure of the macular hole after removal of the microbubble. Based on our results, early microbubble removal operation should be considered in the treatment of an entrapped microbubble within the hole.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Morgan CM. Schatz H. Idiopathic macular holes. Am J Ophthalmol. 1985; 99:437–44.
Article2. Atmaca LS. Yilmaz M. Changes in the fundus caused by blunt ocular trauma. Ann Ophthalmol. 1993; 25:447–52.3. Evans JR. Schwartz SD. McHugh JD, et al. Systemic risk factors for idiopathic macular holes: a case-control study. Eye (Lond). 1998; 12:2. 256–9.
Article4. Jackson TL. Ni cod E. Simpson A, et al. Symptomatic vitreomacular adhesion. Retina. 2013; 33:1503–11.
Article5. Yagi F. Takagi S. Tomita G. Incidence and causes of iatrogenic retinal breaks in idiopathic macular hole and epiretinal membrane. Semin Ophthalmol. 2014; 29:66–9.
Article6. Scott IU. Moraczewski AL. Smiddy WE, et al. Long-term anatomic and visual acuity outcomes after initial anatomic success with macular hole surgery. Am J Ophthalmol. 2003; 135:633–40.
Article7. Thompson JT. Smiddy WE. Glaser BM, et al. Intraocular tamponade duration and success of macular hole surgery. Retina. 1996; 16:373–82.
Article8. Lee SB. Nam KY. Kim KN. Jo YJ. The surgical results of stages 2 and 3 macular hole with internal limiting membrane peeling and intravitreal air. J Korean Ophthalmol Soc. 2009; 50:1076–81.
Article9. Moon SJ. Kang JH. Yoon HS. Long-term visual outcomes and prognostic factors for successful idiopathic macular hole. J Korean Ophthalmol Soc. 2011; 52:1195–201.
Article10. Spaide RF. Macular hole hypotheses. Am J Ophthalmol. 2005; 139:149–51.
Article11. Kwon YK. Eum SJ. Shin JP, et al. Surgical outcomes of taking a reading position after air tamponade in idiopathic macular hole. J Korean Ophthalmol Soc. 2015; 56:1752–8.
Article12. Park JH. Chang WH. Sagong M. Comparison of prone and seated position after vitrectomy for idiopathic macular hole surgery. J Korean Ophthalmol Soc. 2013; 54:1723–30.
Article13. Kapoor KG. Bakri SJ. Air bubbles emanating from the vitrector probe port during vitrectomy. Ophthalmic Surg Lasers Imaging. 2012; 43:439–40.
Article14. Chow DR. Hassan T. Microbubble retention and failed macular hole surgery. Ophthalmic Surg Lasers. 2001; 32:243–4.
Article15. Tatlipinar S. Yenerel NM. Microbubble in the hole: a rare cause of failed macular hole surgery? Retin Cases Brief Rep. 2013; 7:150–1.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case Report of Closed Traumatic Macular Hole after Intravit real Gas Injection
- Long-Term Visual Outcomes and Prognostic Factors for Successful Idiopathic Macular Hole
- Eccentric Macular Hole Formation After Macular Hole Surgery
- Autologous Retinal Flap Transplantation of a Refractory Giant Macular Hole with Retinal Detachment
- A Case of Spontaneous Closure of Macular Hole in a Previously Vitrectomized Eye