J Korean Ophthalmol Soc.
2011 Oct;52(10):1195-1201. 10.3341/jkos.2011.52.10.1195.
Long-Term Visual Outcomes and Prognostic Factors for Successful Idiopathic Macular Hole
- Affiliations
-
- 1Sungmo Eye Hospital, Busan, Korea. heesyoon@dreamwiz.com
- KMID: 2215002
- DOI: http://doi.org/10.3341/jkos.2011.52.10.1195
Abstract
- PURPOSE
To investigate long-term visual outcomes and prognostic factors to predict visual outcomes in patients with anatomic success after macular hole surgery.
METHODS
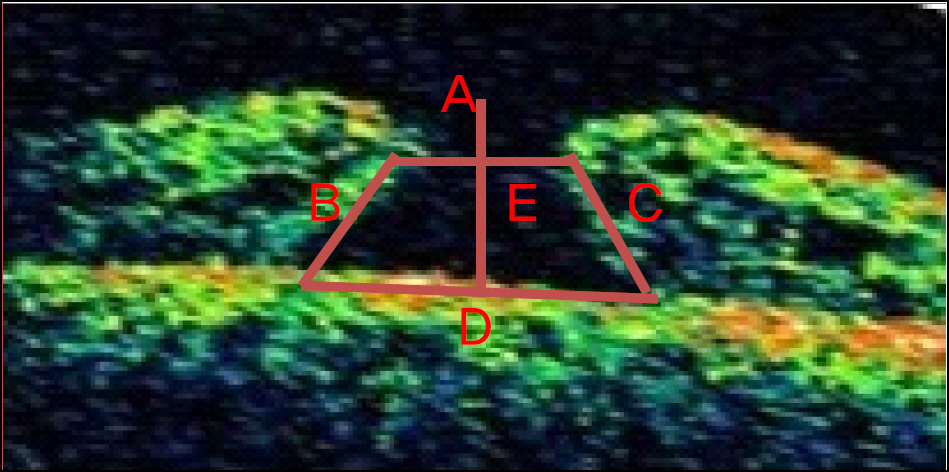
Medical records of 36 eyes with successfully repaired stage 3 or 4 idiopathic macular hole and with at least 24 months of follow-up were reviewed. Hole height, stage of macular hole, base diameter, minimum diameter, hole form factor, macular hole index, and hole closure type were measured or calculated, and the correlations of visual outcomes with variables of preoperative optical coherence tomography (OCT) were analyzed.
RESULTS
The patients were classified into 3 groups according to the time period necessary to achieve the best corrective visual acuity. The visual acuity of 16 eyes (44.4%) recovered in a mean of 6 months, 13 eyes (36.1%) improved slowly and continuously, and 7 eyes had no improvement despite successful anatomical closure. There were no statistical differences in hole height, base diameter, minimum diameter, hole form factor, macular hole index, or closure type among the 3 groups.
CONCLUSIONS
The improvement in visual acuity after successful macular hole surgery persisted at the 24-month follow-up and after. There were no correlations between delayed visual acuity after macular hole surgery and minimum diameter, base diameter, hole height, hole form factor, macular hole index, or closure type.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
A Case of Failed Macular Hole Closure Associated with an Entrapped Microbubble in the Hole
Jinhyun Kim, Gwon Hwi Lee, Seung Woo Lee
J Korean Ophthalmol Soc. 2016;57(5):853-856. doi: 10.3341/jkos.2016.57.5.853.
Reference
-
References
1. Lister W. Holes in the retina and their clinical significance. Br J Ophthalmol. 1924; 8:14–20.
Article2. Gass JD. Idiopathic senile macular hole. Its early stages and pathogenesis. Arch Ophthalmol. 1988; 106:629–39.
Article3. Leonard RE 2nd, Smiddy WE, Flynn HW Jr, Feuer W. Long-term visual outcomes in patients with successful macular hole surgery. Ophthalmology. 1997; 104:1648–52.
Article4. Scott IU, Moraczewski AL, Smiddy WE, et al. Long-term anatomic and visual acuity outcomes after initial anatomic success with macular hole surgery. Am J Ophthalmol. 2003; 135:633–40.
Article5. Kang SJ, Seo MS. Prognostic factors in idiopathic macular hole surgery. J Korean Ophthalmol Soc. 2000; 41:113–22.6. Ullrich S, Haritoglou C, Gass C, et al. Macular hole size as a prognostic factor in macular hole surgery. Br J Ophthalmol. 2002; 86:390–3.
Article7. Kusuhara S, Teraoka Escano MF, Fujii S, et al. Prediction of postoperative visual outcome based on hole configuration by optical coherence tomography in eyes with idiopathic macular holes. Am J Ophthalmol. 2004; 138:709–16.
Article8. Yu SI, Kim HW, Yun IH. The evaluation of prognostic factors after vitrectomy for idiopathic macular hole with OCT. J Korean Ophthalmol Soc. 2007; 48:513–20.9. Kim JH, Lee JE, Oum BS. Evaluation of correlation between OCT findings and visual acuity improvement after macular hole surgery. J Korean Ophthalmol Soc. 2008; 49:763–70.10. Imai M, Iijima H, Gotoh T, Tsukahara S. Optical coherence tomography of successfully repaired idiopathic macular holes. Am J Ophthalmol. 1999; 128:621–7.
Article11. Kim KS, Kim YC. Surgical results of vitrectomy for macular holes, according to the hole size. J Korean Ophthalmol Soc. 2006; 47:927–32.12. Kim SJ, Lee JE, Oum BS. Correlation of preoperativie optical coherence tomography with pre and postoperative visual acuity of macular hole. J Korean Ophthalmol Soc. 2008; 49:583–8.13. Smiddy WE, Feuer W, Cordahi G. Internal limiting membrane peeling in macular hole surgery. Ophthalmology. 2001; 108:1471–6.
Article14. Larsson J, Holm K, Lovestam-Adrian M. The presence of an op-erculum verified by optical coherence tomography and other prognostic factors in macular hole surgery. Acta Ophthalmol Scand. 2006; 84:301–4.
Article15. Kobayashi H, Kobayashi K. Correlation of quantitative three-dimensionalabsorbed measurements of macular hole size with visual acuity after vitrectomy. Graefes Arch Clin Exp Ophthalmol. 1999; 237:283–8.16. Ruiz-Moreno JM, Staicu C, Pinero DP, et al. Optical coherence tomography predictive factors for macular hole surgery outcome. Br J Ophthalmol. 2008; 92:640–4.
Article17. Tadayoni R, Gaudric A, Haouchine B, Massin P. Relationship between macular hole size and the potential benefit of internal limiting membrane peeling. Br J Ophthalmol. 2006; 90:1239–41.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Evaluation of Prognostic Factors after Vitrectomy for Idiopathic Macular Hole with OCT
- Evaluation of Macular Hole Surgery using Confocal Laser Tomography
- The Assessment of Fixation Area and Prognostic Factors in Idiopathic Macular Holes after Vitrectomy with Microperimetry Using Scanning Laser Ophthalmoscope
- Two years results of surgery for idiopathic macular hole
- Prognostic Factors in Idiopathic Macular Hole Surgery