J Korean Surg Soc.
2011 Sep;81(3):187-194. 10.4174/jkss.2011.81.3.187.
Survival benefits of surgical resection in recurrent cholangiocarcinoma
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. Jinseok.heo@samsung.com
- KMID: 2212196
- DOI: http://doi.org/10.4174/jkss.2011.81.3.187
Abstract
- PURPOSE
Attempt to identify the beneficial effects associated with surgical procedures on survival outcome of patients with recurrent cholangiocarcinoma.
METHODS
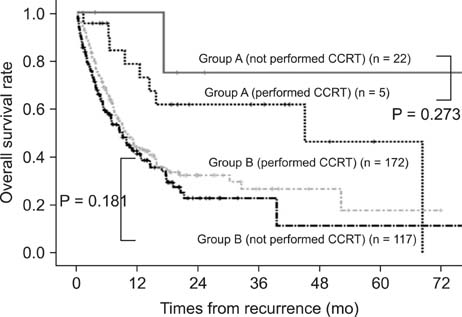
921 patients diagnosed with cholangiocarcinoma underwent surgical resection with curative intent in a single institute during the last 15 years. Patients with recurrent disease were divided into two groups according to whether surgical procedures were performed for the treatment of recurrence. Clinicopathologic variables, ranges of survival based on sites of recurrence, and types of treatment were analyzed retrospectively.
RESULTS
The median follow-up period was 21.8 months and 316 (34.3%) patients had recurrence. 27 (group A) patients with recurrent disease were treated surgically and 289 patients (group B) were not treated. Liver resection, metastasectomy, pancreaticoduodenectomy, partial pancreatectomy, and regional lymph node dissection were performed on the patients in group A. The overall survival rate was statistically higher in group A (P = 0.001). Among the surgical procedures, resection of locoregional recurrences (except liver) in abdominal cavity (4.0 to 101.8 months vs. 0.6 to 71.6 months) and metastasectomy of abdominal or chest wall (3.5 to 18.9 months vs. 1.9 to 2.2 months) showed remarkable differences with respect to the range of survival.
CONCLUSION
Better survival outcomes can be expected by performing surgical resection of locoregional recurrences (except liver) in abdominal cavity and abdominal or chest wall metastatic lesions in recurrent cholangiocarcinoma.
MeSH Terms
Figure
Cited by 1 articles
-
A long-term survival case of advanced biliary cancer with repeated resection due to recurrence in the pancreaticogastrostomy site after pancreaticoduodenectomy
Shohei Eto, Masashi Ishikawa, Michihito Asanoma, Yoshihiko Tashiro, Kazuo Matsuyama, Takehito Oshio
Ann Hepatobiliary Pancreat Surg. 2018;22(2):173-177. doi: 10.14701/ahbps.2018.22.2.173.
Reference
-
1. Kwon OS, Jun DW, Kim SH, Chung MY, Kim NI, Song MH, et al. Distant skeletal muscle metastasis from intrahepatic cholangiocarcinoma presenting as Budd-Chiari syndrome. World J Gastroenterol. 2007. 13:3141–3143.2. Tao LY, He XD, Qu Q, Cai L, Liu W, Zhou L, et al. Risk factors for intrahepatic and extrahepatic cholangiocarcinoma: a case-control study in China. Liver Int. 2010. 30:215–221.3. Park SK, Kim YS, Kim SG, Jang JY, Moon JH, Lee MS, et al. Detection of distant metastasis to skeletal muscle by 18F-FDG-PET in a case of intrahepatic cholangiocarcinoma. Korean J Hepatol. 2010. 16:325–328.4. Zhang KJ, Wang DS, Zhang SY, Jiao XL, Li CW, Wang XS, et al. The E-cadherin repressor slug and progression of human extrahepatic hilar cholangiocarcinoma. J Exp Clin Cancer Res. 2010. 29:88.5. Ito Y, Tajima Y, Fujita F, Tsutsumi R, Kuroki T, Kanematsu T. Solitary recurrence of hilar cholangiocarcinoma in a mediastinal lymph node two years after curative resection. World J Gastroenterol. 2007. 13:2243–2246.6. Singal AG, Rakoski MO, Salgia R, Pelletier S, Welling TH, Fontana RJ, et al. The clinical presentation and prognostic factors for intrahepatic and extrahepatic cholangiocarcinoma in a tertiary care centre. Aliment Pharmacol Ther. 2010. 31:625–633.7. Endo I, Gonen M, Yopp AC, Dalal KM, Zhou Q, Klimstra D, et al. Intrahepatic cholangiocarcinoma: rising frequency, improved survival, and determinants of outcome after resection. Ann Surg. 2008. 248:84–96.8. Ito K, Ito H, Allen PJ, Gonen M, Klimstra D, D'Angelica MI, et al. Adequate lymph node assessment for extrahepatic bile duct adenocarcinoma. Ann Surg. 2010. 251:675–681.9. Francis H, Alpini G, DeMorrow S. Recent advances in the regulation of cholangiocarcinoma growth. Am J Physiol Gastrointest Liver Physiol. 2010. 299:G1–G9.10. Tamandl D, Herberger B, Gruenberger B, Puhalla H, Klinger M, Gruenberger T. Influence of hepatic resection margin on recurrence and survival in intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2008. 15:2787–2794.11. Yamamoto Y, Shimada K, Sakamoto Y, Esaki M, Nara S, Ban D, et al. Clinicopathological characteristics of intrahepatic cholangiocellular carcinoma presenting intrahepatic bile duct growth. J Surg Oncol. 2009. 99:161–165.12. Saxena A, Chua TC, Sarkar A, Chu F, Morris DL. Clinicopathologic and treatment-related factors influencing recurrence and survival after hepatic resection of intrahepatic cholangiocarcinoma: a 19-year experience from an established Australian hepatobiliary unit. J Gastrointest Surg. 2010. 14:1128–1138.13. Shen FZ, Zhang BY, Feng YJ, Jia ZX, An B, Liu CC, et al. Current research in perineural invasion of cholangiocarcinoma. J Exp Clin Cancer Res. 2010. 29:24.14. Park J, Kim MH, Kim KP, Park DH, Moon SH, Song TJ, et al. Natural history and prognostic factors of advanced cholangiocarcinoma without surgery, chemotherapy, or radiotherapy: a large-scale observational study. Gut Liver. 2009. 3:298–305.15. Carrafiello G, Laganà D, Cotta E, Mangini M, Fontana F, Bandiera F, et al. Radiofrequency ablation of intrahepatic cholangiocarcinoma: preliminary experience. Cardiovasc Intervent Radiol. 2010. 33:835–839.16. Nagahashi M, Shirai Y, Wakai T, Sakata J, Ajioka Y, Nomura T, et al. Depth of invasion determines the postresectional prognosis for patients with T1 extrahepatic cholangiocarcinoma. Cancer. 2010. 116:400–405.17. Kurosaki I, Hatakeyama K. Repeated hepatectomy for recurrent intrahepatic cholangiocarcinoma: report of two cases. Eur J Gastroenterol Hepatol. 2005. 17:125–130.18. Kamphues C, Seehofer D, Eisele RM, Denecke T, Pratschke J, Neumann UP, et al. Recurrent intrahepatic cholangiocarcinoma: single-center experience using repeated hepatectomy and radiofrequency ablation. J Hepatobiliary Pancreat Sci. 2010. 17:509–515.19. Kobayashi A, Miwa S, Nakata T, Miyagawa S. Disease recurrence patterns after R0 resection of hilar cholangiocarcinoma. Br J Surg. 2010. 97:56–64.20. Sakamoto Y, Shimada K, Nara S, Esaki M, Ojima H, Sano T, et al. Surgical management of infrahilar/suprapancreatic cholangiocarcinoma: an analysis of the surgical procedures, surgical margins, and survivals of 77 patients. J Gastrointest Surg. 2010. 14:335–343.21. Kim SJ, Lee CY, Kim DG. Analysis of the clinical outcome and prognostic factors of patients with hilar cholangiocarcinoma. J Korean Surg Soc. 2007. 73:156–164.22. Takahashi Y, Nagino M, Nishio H, Ebata T, Igami T, Nimura Y. Percutaneous transhepatic biliary drainage catheter tract recurrence in cholangiocarcinoma. Br J Surg. 2010. 97:1860–1866.23. Stergiopoulos C, Kountouras J, Kapetanakis N, Katsinelos P, Kokkali S, Tsapournas G, et al. Distant cutaneous metastasis preceding the diagnosis of ductal cholangiocarcinoma. J Eur Acad Dermatol Venereol. 2009. 23:242–243.24. Ohtsuka M, Kimura F, Shimizu H, Yoshidome H, Kato A, Yoshitomi H, et al. Significance of repeated resection for recurrent intrahepatic cholangiocarcinoma. Hepatogastroenterology. 2009. 56:1–5.25. Choi D, Lim HK, Rhim H, Kim YS, Yoo BC, Paik SW, et al. Percutaneous radiofrequency ablation for recurrent hepatocellular carcinoma after hepatectomy: long-term results and prognostic factors. Ann Surg Oncol. 2007. 14:2319–2329.26. Valle J, Wasan H, Palmer DH, Cunningham D, Anthoney A, Maraveyas A, et al. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 2010. 362:1273–1281.27. Buell JF, Rosen S, Yoshida A, Labow D, Limsrichamrern S, Cronin DC, et al. Hepatic resection: effective treatment for primary and secondary tumors. Surgery. 2000. 128:686–693.28. Konishi M, Iwasaki M, Ochiai A, Hasebe T, Ojima H, Yanagisawa A. Clinical impact of intraoperative histological examination of the ductal resection margin in extrahepatic cholangiocarcinoma. Br J Surg. 2010. 97:1363–1368.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinicopathologic Features and Prognosis in Peripheral Cholangiocarcinoma
- Surgery for Perihilar Cholangiocarcinoma
- Clinical Analysis of Intrahepatic Cholangiocarcinoma
- Resection or transplantation for perihilar cholangiocarcinoma
- Analysis of Survival and Factors Affecting the Survival after Surgical Resection of Peripheral Cholangiocarcinoma: 318 Cases in Single Institute