J Korean Surg Soc.
2010 Jun;78(6):369-375. 10.4174/jkss.2010.78.6.369.
Spontaneous Hemoperitoneum in Patients Taking Anticoagulants
- Affiliations
-
- 1Department of Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea. iykim@yonsei.ac.kr
- KMID: 2211967
- DOI: http://doi.org/10.4174/jkss.2010.78.6.369
Abstract
- PURPOSE
Spontaneous hemoperitoneum is not a common disease but may cause a fatal outcome. Warfarin is a coumarin anticoagulant, used widely for therapeutic and prophylactic anticoagulation. Although, it is considered a life saving medicine, it is associated with significant adverse effects including intraabdominal bleeding. Literatures about spontaneous hemoperitoneum in patients taking anticoagulants have been reported, but until now there have not been a definite establishment in diagnostic criteria and treatment strategy.
METHODS
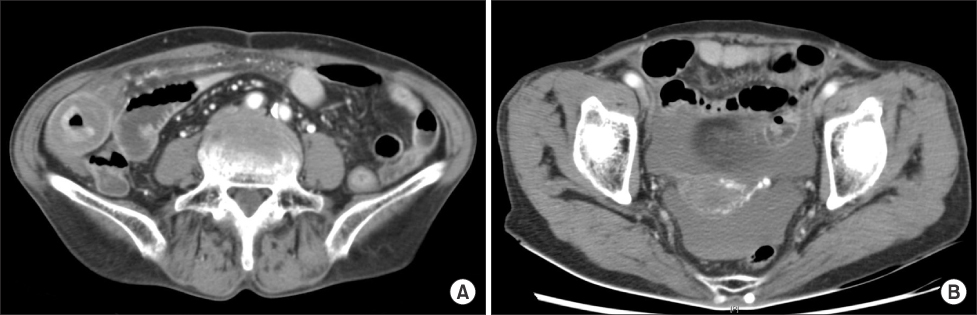
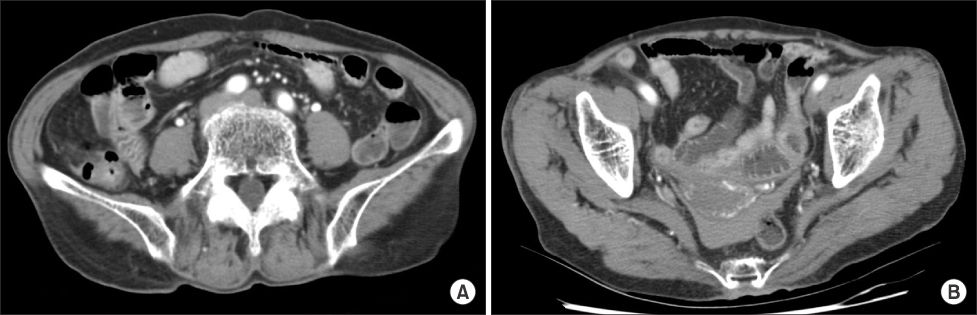
Among 209 patients who were diagnosed hemoperitoneum from Jan 2005 through May 2009, we identified 9 patients with spontaneous hemoperitoneum without any trauma history or solid organ abnormalities. All 9 patients were taking warfarin for various durations. Initially, we evaluated vital signs, laboratory, CT findings, and clinical course, retrospectively. In addition, we analyzed risk factors potentiating the pharmacologic effect of anticoagulants.
RESULTS
One of the most prominent features in this study is that all patients showed prolonged international normalized ratio (6.36~15.11). One patient received an exploratory laparotomy for hemoperitoneum secondary to warfarin, presenting as a localized peritonitis in the right lower quadrant of the abdomen. Mean hospital stay was 15.2 days. Five patients were transfused with packed red blood cells (500~1,000 ml) and fresh frozen plasma (300~900 ml). All patients were discharged without any mortality.
CONCLUSION
It is important to identify and confirm the factors that can potentiate the pharmacologic effect of anticoagulants, when acute abdomen is suspected in patients taking anticoagulants. If the patients are hemodynamically stable, they can be treated without surgical intervention.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Hemoperitoneum with Splenic Artery Rupture Following Diagnostic Colonoscopy
Yeo Wool Kang, Jong Yoon Lee, Jong Hoon Lee
Korean J Gastroenterol. 2020;76(5):246-250. doi: 10.4166/kjg.2020.124.
Reference
-
1. Lucey BC, Varghese JC, Soto JA. Spontaneous hemoperitoneum: causes and significance. Curr Probl Diagn Radiol. 2005. 34:182–195.2. Sanderson PL, Davies MF, Howat JM. Idiopathic spontaneous haemoperitoneum. Postgrad Med J. 1988. 64:322–324.3. Levine MN, Raskob G, Landefeld S, Kearon C. Hemorrhagic complications of anticoagulant treatment. Chest. 2001. 119:108S–121S.4. Landefeld CS, Beyth RJ. Anticoagulant-related bleeding: clinical epidemiology, prediction, and prevention. Am J Med. 1993. 95:315–328.5. Gonzalez C, Penado S, Llata L, Valero C, Riancho JA. The clinical spectrum of retroperitoneal hematoma in anticoagulated patients. Medicine (Baltimore). 2003. 82:257–262.6. Ivascu FA, Janczyk RJ, Bair HA, Bendick PJ, Howells GA. Spontaneous retroperitoneal hemorrhage. Am J Surg. 2005. 189:345–347.7. Yang KH, Kim S, Cho YH. Spontaneous hemoperitoneum. J Korean Surg Soc. 2007. 72:66–70.8. Rathod K, Sheth R, Chavhan G, Asrani A, Raut A. Hemoperitoneum complicating snake bite: rare CT features. Abdom Imaging. 2003. 28:820–821.9. Faraj R, Martindale E, Hill S. Massive ovarian cyst haemorrhage with haemoperitoneum as a complication of long-term anticoagulation. J Obstet Gynaecol. 2008. 28:250–251.10. Whitlon DS, Sadowski JA, Suttie JW. Mechanism of coumarin action: significance of vitamin K epoxide reductase inhibition. Biochemistry. 1978. 17:1371–1377.11. Schulman S. Clinical practice. Care of patients receiving long-term anticoagulant therapy. N Engl J Med. 2003. 349:675–683.12. Schulman S. Beutler E, Lichtman MA, Coller BS, Kipps TJ, Seligsohn U, editors. Oral anticoagulation. Williams Hematology. 2001. 6th ed. New York: McGraw-Hill;1777–1792.13. Hylek EM, Singer DE. Risk factors for intracranial hemorrhage in outpatients taking warfarin. Ann Intern Med. 1994. 120:897–902.14. Wells PS, Holbrook AM, Crowther NR, Hirsh J. Interactions of warfarin with drugs and food. Ann Intern Med. 1994. 121:676–683.15. Harder S, Thurmann P. Clinically important drug interactions with anticoagulants. An update. Clin Pharmacokinet. 1996. 30:416–444.16. Lee YS, Kim JJ, Lee KH, Oh SJ, Park SM, Kim YH. Cecal Intramural hematoma after acupuncture in a patient taking anticoagulant drug. J Korean Soc Coloproctol. 2005. 21:109–111.17. Mortele KJ, Cantisani V, Brown DL, Ros PR. Spontaneous intraperitoneal hemorrhage: imaging features. Radiol Clin North Am. 2003. 41:1183–1201.18. Nazarian LN, Lev-Toaff AS, Spettell CM, Wechsler RJ. CT assessment of abdominal hemorrhage in coagulopathic patients: impact on clinical management. Abdom Imaging. 1999. 24:246–249.19. Sagar J, Kumar V, Shah DK, Bhatnagar A. Spontaneous intra-peritoneal bleeding secondary to warfarin, presenting as an acute appendicitis: a case report and review of literature. BMC Blood Disord. 2006. 6:7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Renal Rupture with Hemoperitoneum in a Patient on Continuous Ambulatory Peritoneal Dialysis
- Spontaneous Hemoperitoneum
- A Case of a Spontaneous Hemoperitoneum as the Presentation of a Gastric Arteriovenous Malformation
- A Study of Lupus Anticoagulants and Anticardiolipin Antibodies in Patients with Infertility and Recurrent Spontaneous Abortion
- A case of hemoperitoneum to spontaneous perforation of uterine leiomyoma with huge cystic degeneration