J Korean Ophthalmol Soc.
2009 Jan;50(1):61-68. 10.3341/jkos.2009.50.1.61.
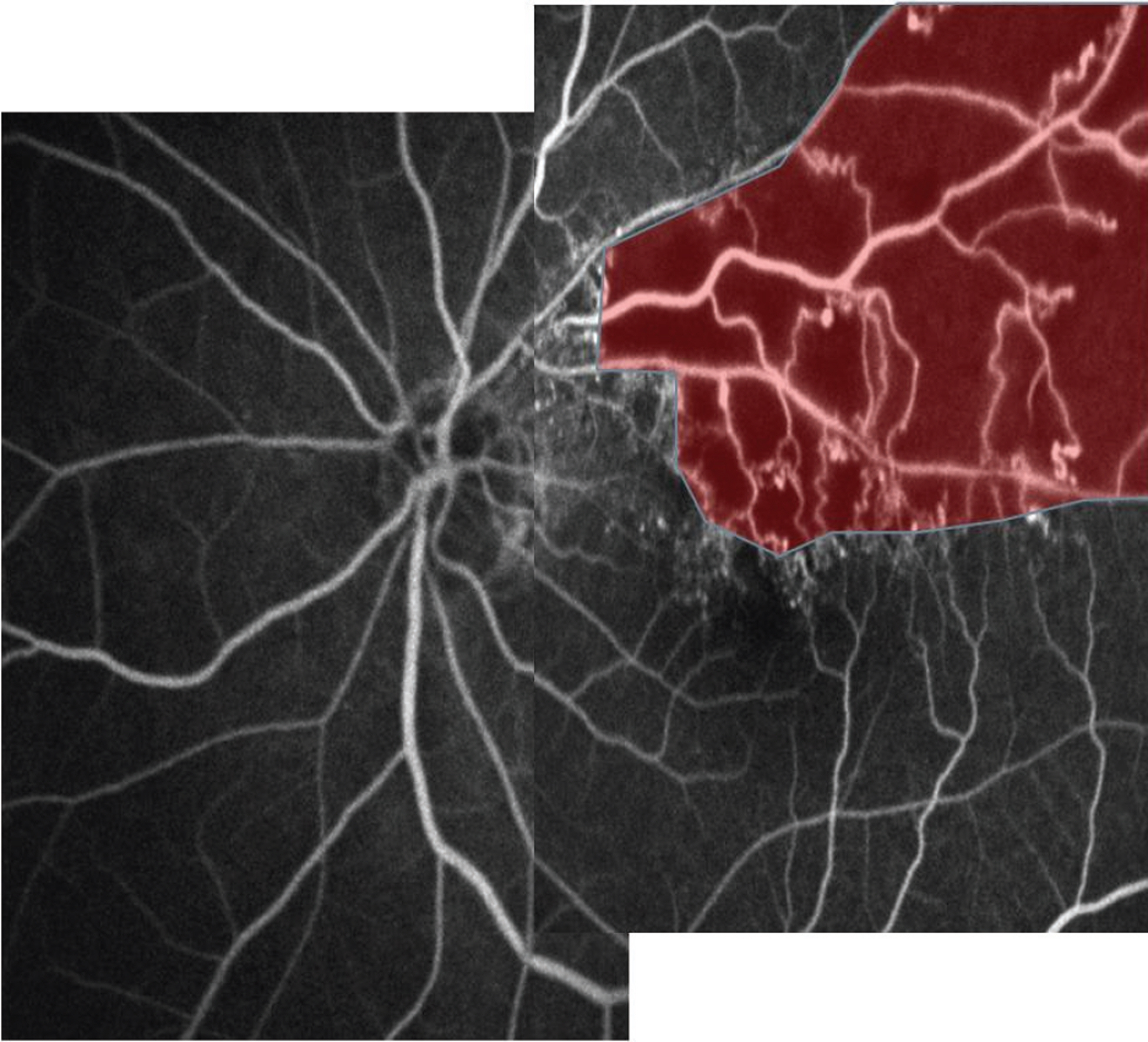
Formation of Collateral Vessels and New Vessels in Branch Retinal Vein Occlusion
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Wonkwang University, Iksan, Korea. ysyang@wonkwang.ac.kr
- KMID: 2211898
- DOI: http://doi.org/10.3341/jkos.2009.50.1.61
Abstract
- PURPOSE
To study the development of collateral vessels and new vessels according to the types of branch retinal vein occlusion (BRVO).
METHODS
One hundred and nine eyes of 103 patients with branch retinal vein occlusion were divided into 4 groups by anatomical position of blockage site and pattern of neovascularization. fluorescein angiography was used to examine perfusion/nonperfusion, size of obstruction site, distance between obstruction site and optic disc (or macula). We compared initial visual acuity and final visual acuity.
RESULTS
there was no statistically significant difference between group in size, between the obstruction site and the optic disc, between the obstruction site and macula. Collateral vessels occurred in major vessel obstruction (MVO) and major vessel and macula obstruction (MVMO) more than in macula obstruction (MO) and peripheral vessel obstruction (PV). Collateral vessels occurred 50 eyes in patients with macula edema and new vessels occurred 36 eyes in patients with macula edema. In collateral group, there was higher incidence of collateral vessels in ischemic type compared to nonischemic type and higher incidence of collateral vessels after laser photocoagulation. ischemic group with collateral vessels had better visual acuity prognosis than perfusion group with collateral vessels.
CONCLUSIONS
collateral vessels in BRVO have a favorable effect on visual prognosis. If patients with collateral vessels shows ischemic type, macula edema and involvement of first order, early laser photocoagulation is recommended for visual prognosis.
MeSH Terms
Figure
Cited by 1 articles
-
Influence of Intravitreal Bevacizumab Injection on Formation of Collateral Vessels in Branch Retinal Vein Occlusion
Yeng Woo Son, Seung Woo Lee
J Korean Ophthalmol Soc. 2016;57(4):582-587. doi: 10.3341/jkos.2016.57.4.582.
Reference
-
References
1. Weinberg D, Dodwell DG, Fern SA. Anatomy of arteriovenous crossings in branch retinal vein occlusion. Am J Ophthalmol. 1990; 109:298–302.
Article2. Christoffersen NL, Larsen M. Pathophysiology and hemodynamic of branch retinal vein occlusion. Ophtha-mology. 1999; 106:2054–62.3. Ryan SJ. Retina. 4th. Vol. 2. St Louis: The C.V Mosby Company;2006. p. 1349–54.4. Orth DH, Patz A. Retinal branch vein occlusion. Surv Opthalmol. 1978; 22:357–76.
Article5. Raitta C. Central venous and retinal venous occlusion. Acta Ophthalmol. 1965; 83:1–123.6. Na KS, Yoon HM, Ji NC. A study on arteriovenous crossing sites in branch retinal vein occlusion. J Korean Ophthalmol Soc. 1992; 33:148–53.7. Park NG, Park YH, Hahn DK. Risk factors and clinical course of bilateral branch retinal vein occlusion. J Korean Ophthalmol Soc. 1995; 36:1493–7.8. Lee DY, Lee SH. Clinical research on the branch retinal vein occlusion. 1989; 30:933–42.9. Appiah AP, Trempe CL. Risk factors associated with branch vs central retinal vein occlusion. Ann Ophthalmol. 1989; 21:153–5. 7.10. Gutman FA. Evaluation of a patient with central retinal vein occlusion. Ophthalmology. 1983; 90:481–3.
Article11. Klein BA, Olwin JH. A survey on the pathogenesis of retinal vein occlusion. Arch Ophthalmol. 1956; 56:207–47.12. Lee DY, Lee SH. Clinical research on the branch retinal vein occlusion. J Korean Ophthalmol Soc. 1989; 30:933–42.13. Yoon YH, Lee JH. Clinical observation on retinal vein occlusion. J Korean Ophthalmol Soc. 1984; 25:477–84.14. Kang KT, Kim YJ. Collateral circulation in the branch retinal vein occlusion. J Korean Ophthalmol Soc. 1991; 32:652–8.15. David Orth. Color and fluorescein angiographic atlas of retinal vascular disorder. Baltimore: Williams & Wilkins;1984. p. 126–60.16. Kanski JJ. Clinical ophthalmology. 6th. London: Butterworth International Edition;2007. p. 585–8.17. Yang HN, Kim YJ, Kim JC, Shyn KH. Clinical evaluation for Branch retinal vein occlusion. J Korean Ophthalmol Soc. 1992; 33:599–604.18. Duker JS, Brown GC. Anterior location of the crossing artery in branch retinal vein occlusion. Arch Ophthalmol. 1989; 107:998–1000.19. Michaelsin IC. Textbook of the fundus of the eye. 3rd. Edinburgh: Churchil Livingston;1980. p. 216–43.20. Oshikiri M. Clinical study on retinal vein occlusion. Jpn J Ophthalmol. 1986; 90:41–51.21. Ball CJ, Henkind P. Retinal arteriolar collaterals in man. Br J Ophthalmol. 1967; 51:688–91.
Article22. Branch Retinal Vein Occlusion Group Argon laser photocoagulation for macular edema in branch retinal vein occlusion. Am J Ophthalmol. 1986; 98:271–82.23. Guttman FA. Macular edema in branch retinal vein occlusion. Trans Am Acad Ophthalmol Otolaryngol. 1977; 83:488–95.24. Kwon OW, Kim JS, Hong YJ, Kim HB. Size of capillary nonperfusion and their prognosis on branch retinal vein occlusion patients. J Korean Ophthalmol Soc. 1993; 34:1162–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Collateral vessels in branch retinal vein occlusion
- Influence of Intravitreal Bevacizumab Injection on Formation of Collateral Vessels in Branch Retinal Vein Occlusion
- Collateral Circulation in the Branch Retinal Vein Occlusion
- Arteriovenous Crossing Patterns in the Normal Retina
- Retinal Arteriolar Changes in a Patient with Branch Retinal Vein Occlusion