J Korean Ophthalmol Soc.
2008 May;49(5):763-770. 10.3341/jkos.2008.49.5.763.
Evaluation of Correlation Between OCT Findings and Delayed Visual Acuity Improvement After Macular Hole Surgery
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Pusan National University, Pusan, Korea. jlee@pusan.ac.kr
- KMID: 2211706
- DOI: http://doi.org/10.3341/jkos.2008.49.5.763
Abstract
-
PURPOSE: We evaluated the relationship between the delayed visual acuity (VA) improvement and retinal features, including in the photoreceptor layer, after a successful macular hole surgery using optical coherence tomography (OCT) images during long-term post-operative observation. The goal was to find the mechanism in delayed VA improvement.
METHODS
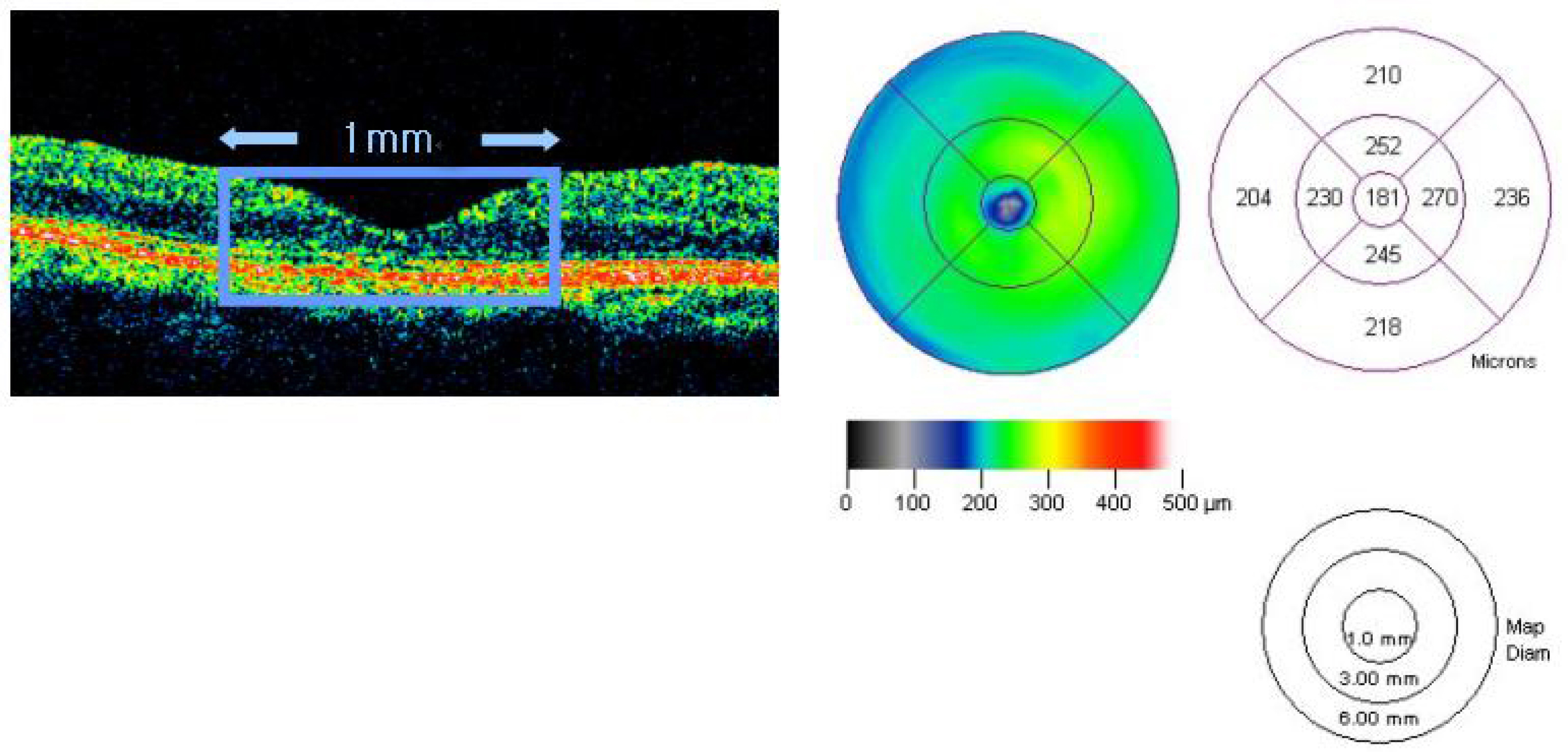
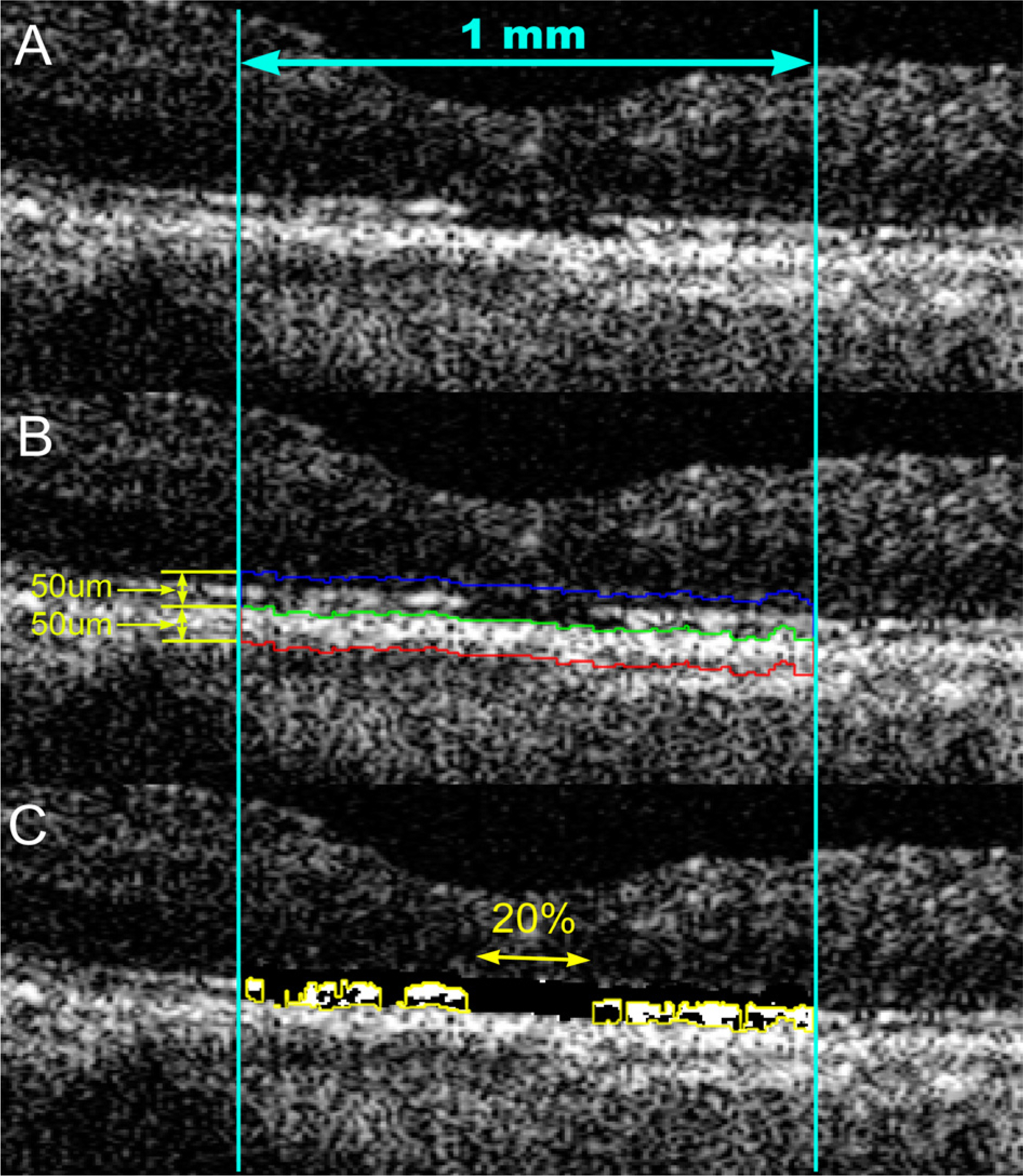
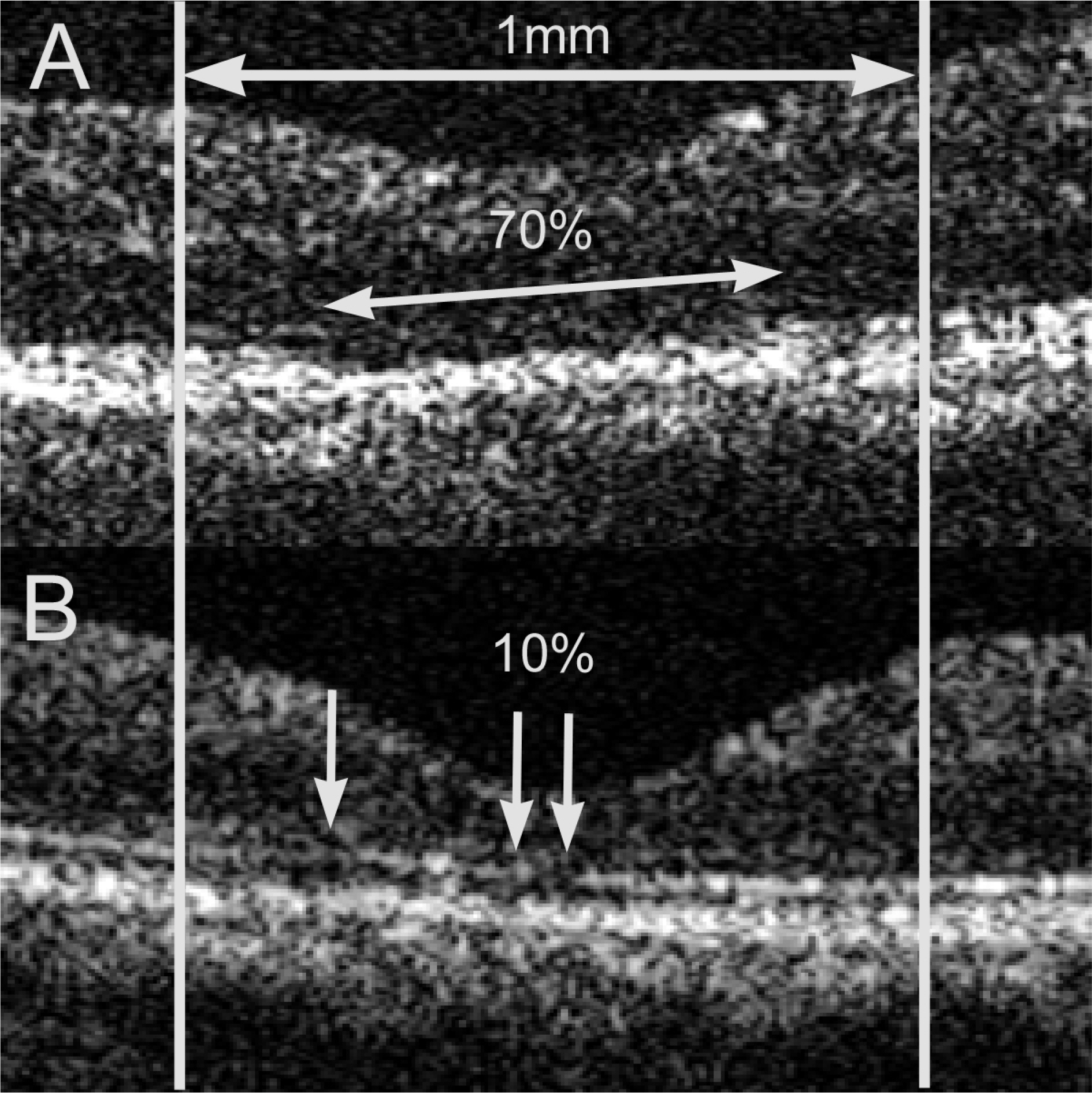
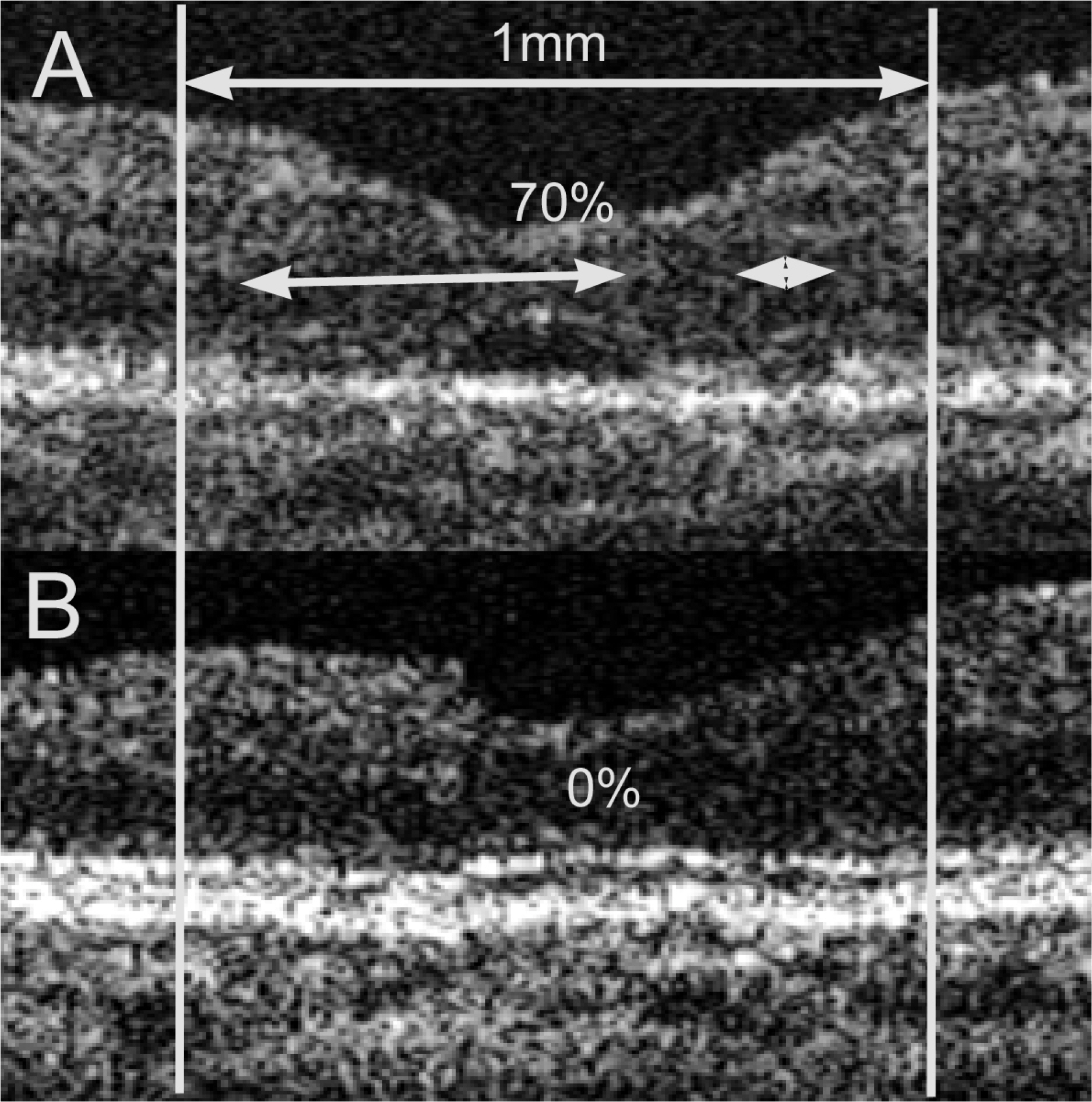
Postoperative OCT scans were analyzed in nine eyes of eight patients who underwent idiopathic macular hole surgery between June 2003 to June 2005. Horizontal and vertical OCT scans taken of the operated eyes immediately after absorption of intraocular gas and after VA improvement were exported to Adobe Photoshop 7.0. We measured changes in parameters of the central foveal thickness (central 1 mm area), photoreceptor layer thickness, relative reflectivity of photoreceptor to retinal pigment epithelium, and the defective area of photoreceptor layer.
RESULTS
The median visual acuity was determined to be 0.2 (range: 0.15~0.3) at the VA unimproved period and 0.5 (range: 0.3~1.0) at VA improved period. The mean central foveal thickness decreased from 221.3 micrometer (range: 155~265 micrometer) to 191.2 micrometer (range: 150~231 micrometer), as VA improved (p=0.007). The mean photoreceptor layer thickness increased from 15.2 micrometer (range: 4.2~27.6 micrometer) to 22.6 micrometer (range: 4.2~35.8 micrometer) as VA improved (p=0.032), and mean relative reflectivity of photoreceptor layer increased from 0.43 (range: 0.08~0.67) to 0.48 (range: 0.10~0.70), as VA improved (p=0.415). The defective area of photoreceptor layer decreased from 70% (range: 90~45%) to 27% (range: 8~5), as VA improved (p=0.001).
CONCLUSIONS
A decrease of the central foveal thickness and of photoreceptor layer defective signal, and an increase of photoreceptor layer thickness were observed on OCT during delayed vision improvement after a successful macular hole surgery. Improvement of macular edema and photoreceptor reorganization are suggested as important parts of the mechanism toward vision recovery.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Noyes HD. Detachment of retina with laceration at macula. Trans Am Ophthalmol Soc. 1871; 1:128–9.2. Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes; results of a pilot study. Arch Ophthalmol. 1991; 109:654–9.
Article3. Kang SJ, Seo MS. Prognostic factors in idiopathic macular hole surgery. J Korean Ophthalmol Soc. 2000; 41:1746–52.4. Lee JE, Oum BS. Macular Hole Surgery with or without Indocyanine Green Assisted Internal Limiting Membrane Peeling. J Korean Ophthalmol Soc. 2003; 44:2553–9.5. Hahm IR, Tae KS, Cho SW, et al. The Outcomes After Indocyanine Green-assisted Peeling of the Internal Limiting Membrane in Macular Hole Surgery. J Korean Ophthalmol Soc. 2005; 46:1361–7.6. Uemoto R, Yamamoto S, Aoki T, et al. Macular configuration determined by optical coherence tomography after idiopathic macular hole surgery with or without internal limiting membrane peeling. Br J Ophthalmol. 2002; 85:1240–2.
Article7. Ryan EH Jr, Gilbert HD. Results of surgical treatment of recent onset full thickness idiopathic macular holes. Arch Ophthalmol. 1994; 112:1545–53.8. Ullrich S, Haritoglou C, Gass C, et al. Macular hole size as a prognostic factor in macular hole surgery. Br J Ophthalmol. 2002; 86:390–3.
Article9. Choung HK, Chung H. Prognosis of Retinal Detachment Caused by Macular Hole according to the Refractive Power. J Korean Ophthalmol Soc. 2002; 43:274–80.10. Hee MR, Puliafito CA, Wong C, et al. Optical coherence tomography of macular holes. Ophthalmology. 1995; 102:748–56.
Article11. Tornambe PE, Poliner LS, Cohen RG. Definition of macular hole surgery end points: elevated/open, flat/open, flat/closed. Retina. 1998; 18:286–7.
Article12. Kang SW, Ahn K, Ham DI. Types of macular hole closure and their clinical implications. Br J Ophthalmol. 2003; 87:1015–9.
Article13. Kitaya N, Hikichi T, Kagokawa H, et al. Irregularity of photoreceptor layer after successful macular hole surgery prevents visual acuity improvement. Am J Ophthalmol. 2004; 138:308–10.
Article14. Villate N, Lee JE, Venkatraman A, Smiddy WE. Photoreceptor layer features in eyes with closed macular holes: optical coherence tomography findings and correlation with visual outcomes. Am J Ophthalmol. 2005; 139:280–9.
Article15. Ko TH, Witkin AJ, Fujimoto JG, et al. Ultrahigh-resolution optical coherence tomography of surgically closed macular holes. Arch Ophthalmol. 2006; 6:827–36.
Article16. Sato H, Kawasaki R, Yamashita H. Observation of idiopathic full-thickness macular hole closure in early postoperative period as evaluated by optical coherence tomography. Am J Ophthalmol. 2003; 136:185–7.
Article17. Leonard RE, Smiddy WE, Flynn HW Jr, Feuer W. Long-term visual outcomes in patients with successful macular hole surgery. Ophthalmology. 1997; 104:1648–52.
Article18. Lee JE, Kim EH, Oum BS. Relationship between Visual Acuity and Photoreceptor Layer or Foveal Thickness on Optical Coherence Tomography after Macular Hole Surgery. J Korean Ophthalmol Soc. 2006; 47:1966–71.19. Brooks HL Jr. Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology. 2000; 107:1939–48.
Article20. Mikajiri K, Okada AA, Ohji M, et al. Analysis of vitrectomy for idiopathic macular hole by optical coherence tomography. Am J Ophthalmol. 1999; 128:655–7.
Article21. Apostolopoulos MN, Koutsandrea CN, Moschos MN, et al. Evaluation of successful macular hole surgery by optical coherence tomography and multifocal electroretinography. Am J Ophthalmol. 2002; 134:667–74.
Article22. Desai VN, Hee MR, Puliafito CA. OCT of macular holes. Madreperla SA, McCuen BW II, editors. Macular hole: pathogenesis, diagnosis and treatment, diagnosis and treatment. 1st ed.Boston: Butterworth-Heinemann;1999. 1.23. Anderson DH, Fisher SK. Disc Shedding in Rodlike and Cone like Photoreceptors of Tree Squirrels. Science. 1975; 187:953–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correlation of Preoperative Optical Coherence Tomography with Preand Postoperative Visual Acuity of Macular Hole
- Evaluation of Macular Hole Surgery using Confocal Laser Tomography
- Long-Term Visual Outcomes and Prognostic Factors for Successful Idiopathic Macular Hole
- The Spontaneous Resolution of Idiopathic Macular Hole Diagnosed with OCT
- Relationship between Visual Acuity and Photoreceptor Layer or Foveal Thickness on Optical Coherence Tomography after Macular Hole Surgery