J Pathol Transl Med.
2016 Mar;50(2):83-95. 10.4132/jptm.2015.11.23.
Sentinel Lymph Node in Breast Cancer: Review Article from a Pathologist's Point of View
- Affiliations
-
- 1Department of Pathology and Laboratory Medicine, University of California at Los Angeles (UCLA), Los Angeles, CA, USA. sapple@mednet.ucla.edu
- KMID: 2211375
- DOI: http://doi.org/10.4132/jptm.2015.11.23
Abstract
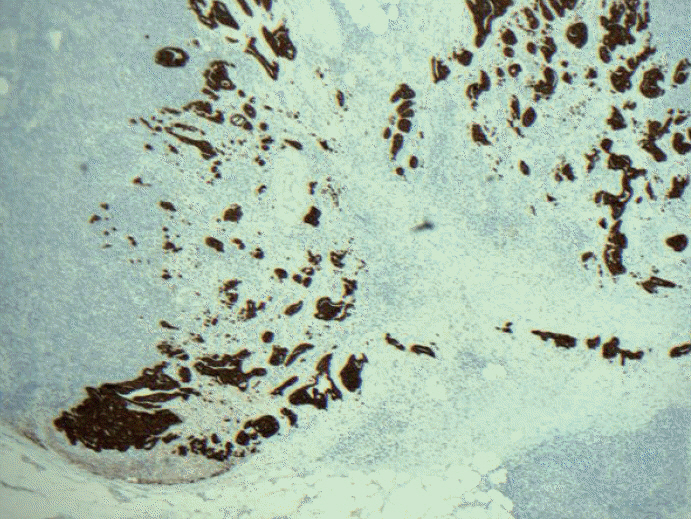
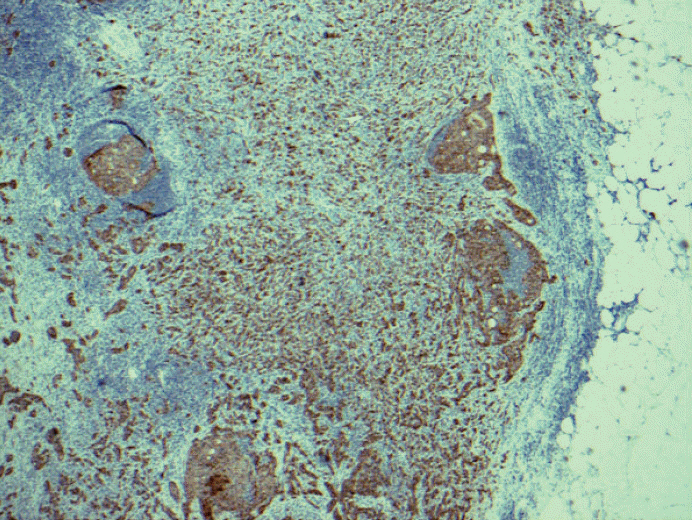
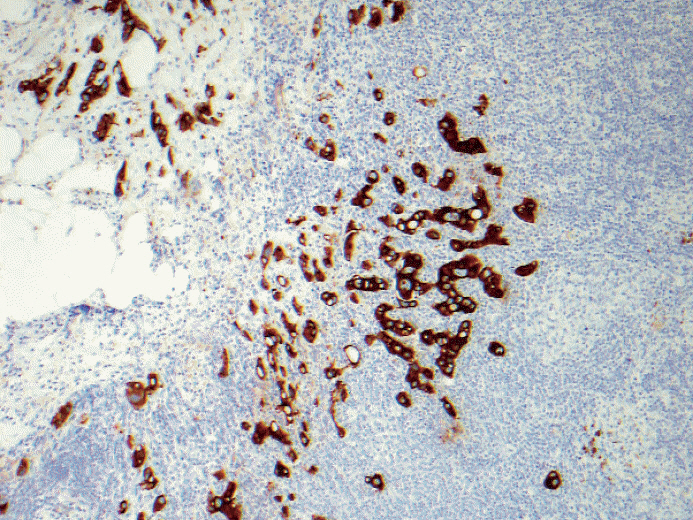
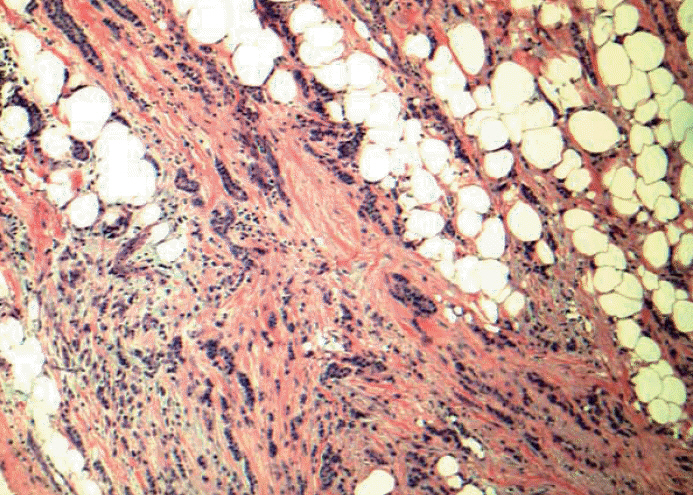
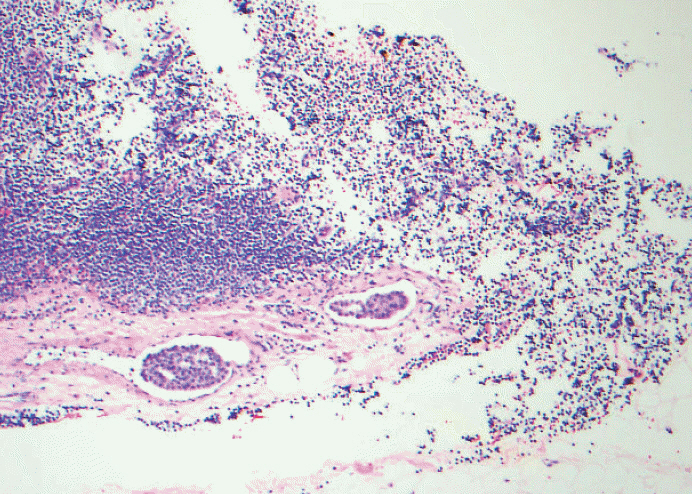
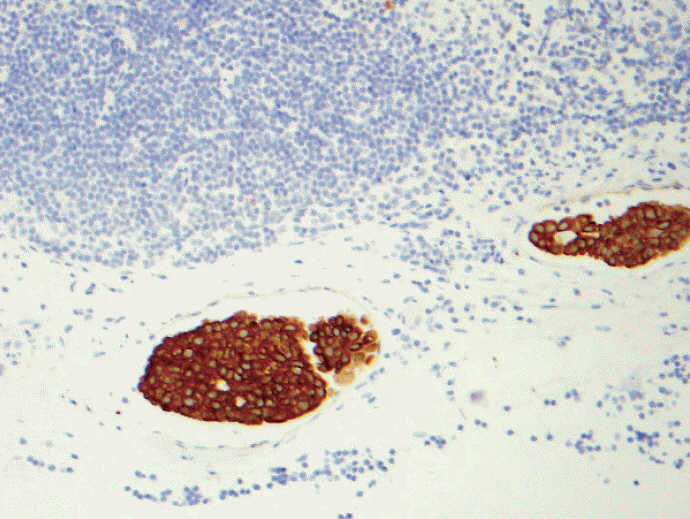
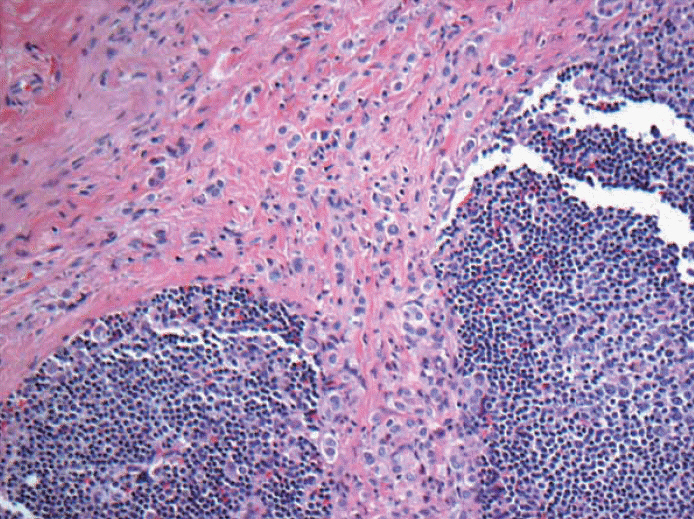
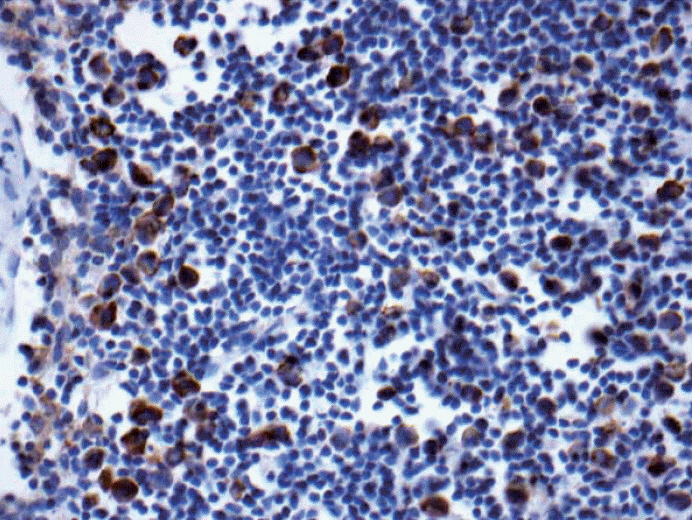
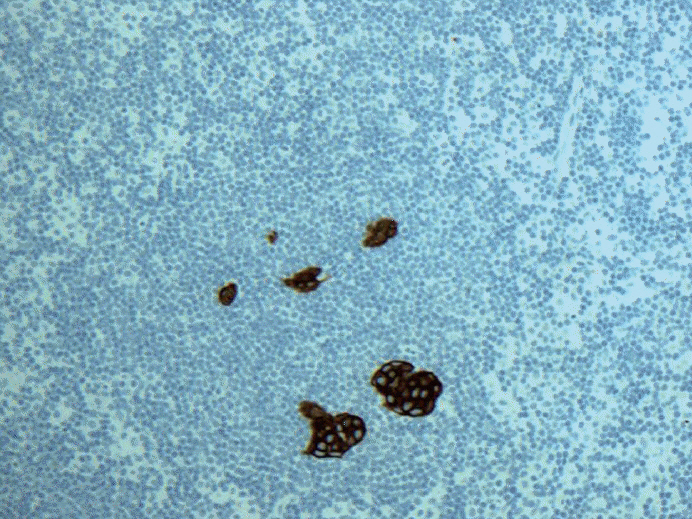
- Breast cancer staging, in particular N-stage changed most significantly due to the advanced technique of sentinel lymph node biopsy two decades ago. Pathologists have more thoroughly examined and scrutinized sentinel lymph node and found increased number of small volume metastases. While pathologists use the strict criteria from the Tumor Lymph Node Metastasis (TNM) Classification, studies have shown poor reproducibility in the application of American Joint Committee on Cancer and International Union Against Cancer/TNM guidelines for sentinel lymph node classification in breast cancer. In this review article, a brief history of TNM with a focus on N-stage is described, followed by innate problems with the guidelines, and why pathologists may have difficulties in assessing lymph node metastases uniformly. Finally, clinical significance of isolated tumor cells, micrometastasis, and macrometastasis is described by reviewing historical retrospective data and significant prospective clinical trials.
MeSH Terms
Figure
Reference
-
1. Trojani M, de Mascarel I, Bonichon F, Coindre JM, Delsol G. Micrometastases to axillary lymph nodes from carcinoma of breast: detection by immunohistochemistry and prognostic significance. Br J Cancer. 1987; 55:303–6.
Article2. Hainsworth PJ, Tjandra JJ, Stillwell RG, et al. Detection and significance of occult metastases in node-negative breast cancer. Br J Surg. 1993; 80:459–63.
Article3. Clare SE, Sener SF, Wilkens W, Goldschmidt R, Merkel D, Winchester DJ. Prognostic significance of occult lymph node metastases in node-negative breast cancer. Ann Surg Oncol. 1997; 4:447–51.
Article4. Sedmak DD, Meineke TA, Knechtges DS, Anderson J. Prognostic significance of cytokeratin-positive breast cancer metastases. Mod Pathol. 1989; 2:516–20.5. Chen ZL, Wen DR, Coulson WF, Giuliano AE, Cochran AJ. Occult metastases in the axillary lymph nodes of patients with breast cancer node negative by clinical and histologic examination and conventional histology. Dis Markers. 1991; 9:239–48.6. de Mascarel I, Bonichon F, Coindre JM, Trojani M. Prognostic significance of breast cancer axillary lymph node micrometastases assessed by two special techniques: reevaluation with longer follow-up. Br J Cancer. 1992; 66:523–7.
Article7. Denoix PF. Tumor, node and metastasis (TNM). Bull Inst Nat Hyg (Paris). 1944; 1:1–69.8. Sobin LH, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours. 7th ed. New York: John Wiley and Sons Inc.;2009.9. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC cancer staging manual. 7th ed. New York: Springer;2009.10. Giuliano AE, Kirgan DM, Guenther JM, Morton DL. Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann Surg. 1994; 220:391–8.
Article11. Fleming ID, Cooper JS, Hensen DE, et al. AJCC cancer staging manual. 5th ed. Philadelphia: Lippincott-Raven;1997.12. Singletary SE, Allred C, Ashley P, et al. Staging system for breast cancer: revisions for the 6th edition of the AJCC Cancer Staging Manual. Surg Clin North Am. 2003; 83:803–19.
Article13. Huvos AG, Hutter RV, Berg JW. Significance of axillary macrometastases and micrometastases in mammary cancer. Ann Surg. 1971; 173:44–6.
Article14. Fisher ER, Palekar A, Rockette H, Redmond C, Fisher B. Pathologic findings from the National Surgical Adjuvant Breast Project (Protocol No. 4). V. Significance of axillary nodal micro- and macrometastases. Cancer. 1978; 42:2032–8.15. Nasser IA, Lee AK, Bosari S, Saganich R, Heatley G, Silverman ML. Occult axillary lymph node metastases in “node-negative” breast carcinoma. Hum Pathol. 1993; 24:950–7.
Article16. Greene FL, Page DL, Fleming ID, et al. AJCC cancer staging manual. 6th ed. New York: Springer-Verlag;2002.17. Bleiweiss IJ, Nagi CS, Jaffer S. Axillary sentinel lymph nodes can be falsely positive due to iatrogenic displacement and transport of benign epithelial cells in patients with breast carcinoma. J Clin Oncol. 2006; 24:2013–8.
Article18. Fitzgibbons PL, Page DL, Weaver D, et al. Prognostic factors in breast cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med. 2000; 124:966–78.19. Hansen NM, Grube BJ, Giuliano AE. The time has come to change the algorithm for the surgical management of early breast cancer. Arch Surg. 2002; 137:1131–5.
Article20. Singletary SE, Connolly JL. Breast cancer staging: working with the sixth edition of the AJCC Cancer Staging Manual. CA Cancer J Clin. 2006; 56:37–47.
Article21. Kim T, Giuliano AE, Lyman GH. Lymphatic mapping and sentinel lymph node biopsy in early-stage breast carcinoma: a metaanalysis. Cancer. 2006; 106:4–16.22. McCready DR, Yong WS, Ng AK, Miller N, Done S, Youngson B. Influence of the new AJCC breast cancer staging system on sentinel lymph node positivity and false-negative rates. J Natl Cancer Inst. 2004; 96:873–5.
Article23. Cserni G, Gregori D, Merletti F, et al. Meta-analysis of non-sentinel node metastases associated with micrometastatic sentinel nodes in breast cancer. Br J Surg. 2004; 91:1245–52.
Article24. Viale G, Maiorano E, Mazzarol G, et al. Histologic detection and clinical implications of micrometastases in axillary sentinel lymph nodes for patients with breast carcinoma. Cancer. 2001; 92:1378–84.
Article25. van Deurzen CH, de Boer M, Monninkhof EM, et al. Non-sentinel lymph node metastases associated with isolated breast cancer cells in the sentinel node. J Natl Cancer Inst. 2008; 100:1574–80.
Article26. Connolly JL. Changes and problematic areas in interpretation of the AJCC Cancer Staging Manual, 6th Edition, for breast cancer. Arch Pathol Lab Med. 2006; 130:287–91.
Article27. Cserni G, Bianchi S, Vezzosi V, et al. Variations in sentinel node isolated tumour cells/micrometastasis and non-sentinel node involvement rates according to different interpretations of the TNM definitions. Eur J Cancer. 2008; 44:2185–91.
Article28. Cserni G, Bianchi S, Boecker W, et al. Improving the reproducibility of diagnosing micrometastases and isolated tumor cells. Cancer. 2005; 103:358–67.
Article29. Cserni G, Sapino A, Decker T. Discriminating between micrometastases and isolated tumor cells in a regional and institutional setting. Breast. 2006; 15:347–54.
Article30. Turner RR, Weaver DL, Cserni G, et al. Nodal stage classification for breast carcinoma: improving interobserver reproducibility through standardized histologic criteria and image-based training. J Clin Oncol. 2008; 26:258–63.
Article31. de Mascarel I, MacGrogan G, Debled M, Brouste V, Mauriac L. Distinction between isolated tumor cells and micrometastases in breast cancer: is it reliable and useful? Cancer. 2008; 112:1672–8.32. Cserni G, Amendoeira I, Bianchi S, et al. Distinction of isolated tumour cells and micrometastasis in lymph nodes of breast cancer patients according to the new Tumour Node Metastasis (TNM) definitions. Eur J Cancer. 2011; 47:887–94.
Article33. Vestjens JH, Pepels MJ, de Boer M, et al. Relevant impact of central pathology review on nodal classification in individual breast cancer patients. Ann Oncol. 2012; 23:2561–6.
Article34. Apple SK, Moatamed NA, Finck RH, Sullivan PS. Accurate classification of sentinel lymph node metastases in patients with lobular breast carcinoma. Breast. 2010; 19:360–4.
Article35. Lyman GH, Giuliano AE, Somerfield MR, et al. American Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J Clin Oncol. 2005; 23:7703–20.36. Chen SL, Hoehne FM, Giuliano AE. The prognostic significance of micrometastases in breast cancer: a SEER population-based analysis. Ann Surg Oncol. 2007; 14:3378–84.
Article37. de Boer M, van Deurzen CH, van Dijck JA, et al. Micrometastases or isolated tumor cells and the outcome of breast cancer. N Engl J Med. 2009; 361:653–63.
Article38. Pugliese MS, Beatty JD, Tickman RJ, et al. Impact and outcomes of routine microstaging of sentinel lymph nodes in breast cancer: significance of the pN0(i+) and pN1mi categories. Ann Surg Oncol. 2009; 16:113–20.
Article39. Hansen NM, Grube B, Ye X, et al. Impact of micrometastases in the sentinel node of patients with invasive breast cancer. J Clin Oncol. 2009; 27:4679–84.
Article40. Bilimoria KY, Bentrem DJ, Hansen NM, et al. Comparison of sentinel lymph node biopsy alone and completion axillary lymph node dissection for node-positive breast cancer. J Clin Oncol. 2009; 27:2946–53.
Article41. Yi M, Giordano SH, Meric-Bernstam F, et al. Trends in and outcomes from sentinel lymph node biopsy (SLNB) alone vs. SLNB with axillary lymph node dissection for node-positive breast cancer patients: experience from the SEER database. Ann Surg Oncol. 2010; 17 Suppl 3:343–51.
Article42. Cyr A, Gao F, Gillanders WE, Aft RL, Eberlein TJ, Margenthaler JA. Disease recurrence in sentinel node-positive breast cancer patients forgoing axillary lymph node dissection. Ann Surg Oncol. 2012; 19:3185–91.
Article43. Vergara-Lluri ME, Prati R, Petersen J, Omidvar Y, Apple SK. Recurrence rates in breast cancer patients who had sentinel lymph node biopsy alone versus completion axillary lymph node dissection: a 7-year clinical follow-up study. Breast J. 2014; 20:666–8.
Article44. Fu Y, Chung D, Cao MA, Apple S, Chang H. Is axillary lymph node dissection necessary after sentinel lymph node biopsy in patients with mastectomy and pathological N1 breast cancer? Ann Surg Oncol. 2014; 21:4109–23.
Article45. Krag DN, Anderson SJ, Julian TB, et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010; 11:927–33.
Article46. Giuliano AE, Hunt KK, Ballman KV, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011; 305:569–75.47. Galimberti V, Cole BF, Zurrida S, et al. Axillary dissection versus no axillary dissection in patients with sentinel-node micrometastases (IBCSG 23-01): a phase 3 randomised controlled trial. Lancet Oncol. 2013; 14:297–305.48. Weaver DL, Ashikaga T, Krag DN, et al. Effect of occult metastases on survival in node-negative breast cancer. N Engl J Med. 2011; 364:412–21.
Article49. Weaver DL, Le UP, Dupuis SL, et al. Metastasis detection in sentinel lymph nodes: comparison of a limited widely spaced (NSABP protocol B-32) and a comprehensive narrowly spaced paraffin block sectioning strategy. Am J Surg Pathol. 2009; 33:1583–9.
Article50. Hieken TJ, Boughey JC. Axillary dissection versus no axillary dissection in patients with sentinel-node micrometastases: commentary on the IBCSG 23-01 Trial. Gland Surg. 2013; 2:128–32.51. Straver ME, Meijnen P, van Tienhoven G, et al. Role of axillary clearance after a tumor-positive sentinel node in the administration of adjuvant therapy in early breast cancer. J Clin Oncol. 2010; 28:731–7.
Article52. AMAROS. The EORTC 10981-22023 AMAROS trial [Internet]. AMAROS, 2010 [cited 2015 Oct 1]. Available from: http://research.nki.nl/amaros/.53. Mansel RE, Fallowfield L, Kissin M, et al. Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: the ALMANAC Trial. J Natl Cancer Inst. 2006; 98:599–609.
Article54. Gill G; SNAC Trial Group of the Royal Australasian College of Surgeons (RACS) and NHMRC Clinical Trials Centre. Sentinel-lymphnode-based management or routine axillary clearance? One-year outcomes of sentinel node biopsy versus axillary clearance (SNAC): a randomized controlled surgical trial. Ann Surg Oncol. 2009; 16:266–75.
Article55. Lucci A, McCall LM, Beitsch PD, et al. Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection compared with SLND alone in the American College of Surgeons Oncology Group Trial Z0011. J Clin Oncol. 2007; 25:3657–63.
Article56. Cote RJ, Peterson HF, Chaiwun B, et al. Role of immunohistochemical detection of lymph-node metastases in management of breast cancer. International Breast Cancer Study Group. Lancet. 1999; 354:896–900.57. Guenther JM, Hansen NM, DiFronzo LA, et al. Axillary dissection is not required for all patients with breast cancer and positive sentinel nodes. Arch Surg. 2003; 138:52–6.
Article58. Tvedskov TF, Jensen MB, Ejlertsen B, Christiansen P, Balslev E, Kroman N. Prognostic significance of axillary dissection in breast cancer patients with micrometastases or isolated tumor cells in sentinel nodes: a nationwide study. Breast Cancer Res Treat. 2015; 153:599–606.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Validation and Controversy of Sentinel Node Biopsy for Breast Cancer
- Sentinel Lymph Node Biopsy in Breast Cancer: A Clinical Review and Update
- The Number of Removed Lymph Nodes for an Acceptable False Negative Rate in Sentinel Lymph Node Biopsy for Breast Cancer
- Sentinel Lymph Node Imaging in Breast Cancer
- Optimized Criteria for Sentinel Lymph Node Biopsy in Patients with Clinically Node Negative Breast Cancer