J Korean Soc Spine Surg.
2006 Sep;13(3):163-169. 10.4184/jkss.2006.13.3.163.
Availability of Anterior Cervical Plating in Distractive Flexion Injury in Lower Cervical Spine: Radiologic Aspects
- Affiliations
-
- 1Department of Orthopaedic Surgery, Eulji University School of Medicine, Daejeon, Korea. jwkang@eulji.ac.kr
- 2Department of Orthopaedic Surgery. Daejeon Veterans Hospital, Daejeon, Korea.
- KMID: 2209637
- DOI: http://doi.org/10.4184/jkss.2006.13.3.163
Abstract
-
STUDY DESIGN: A retrospective clinical and radiological analysis.
OBJECTIVES
To evaluate the availability of anterior cervical plating in the treatment of distractive-flexion injuries of the lower cervical spine. SUMMARY OF LITERATURE REVIEW: Surgical approaches for distractive-flexion injuries of the lower cervical spine have included the anterior approach, the posterior approach, and the combined anterior and posterior approach. However, which approach is the most useful remains a controversial issue.
MATERIALS AND METHODS
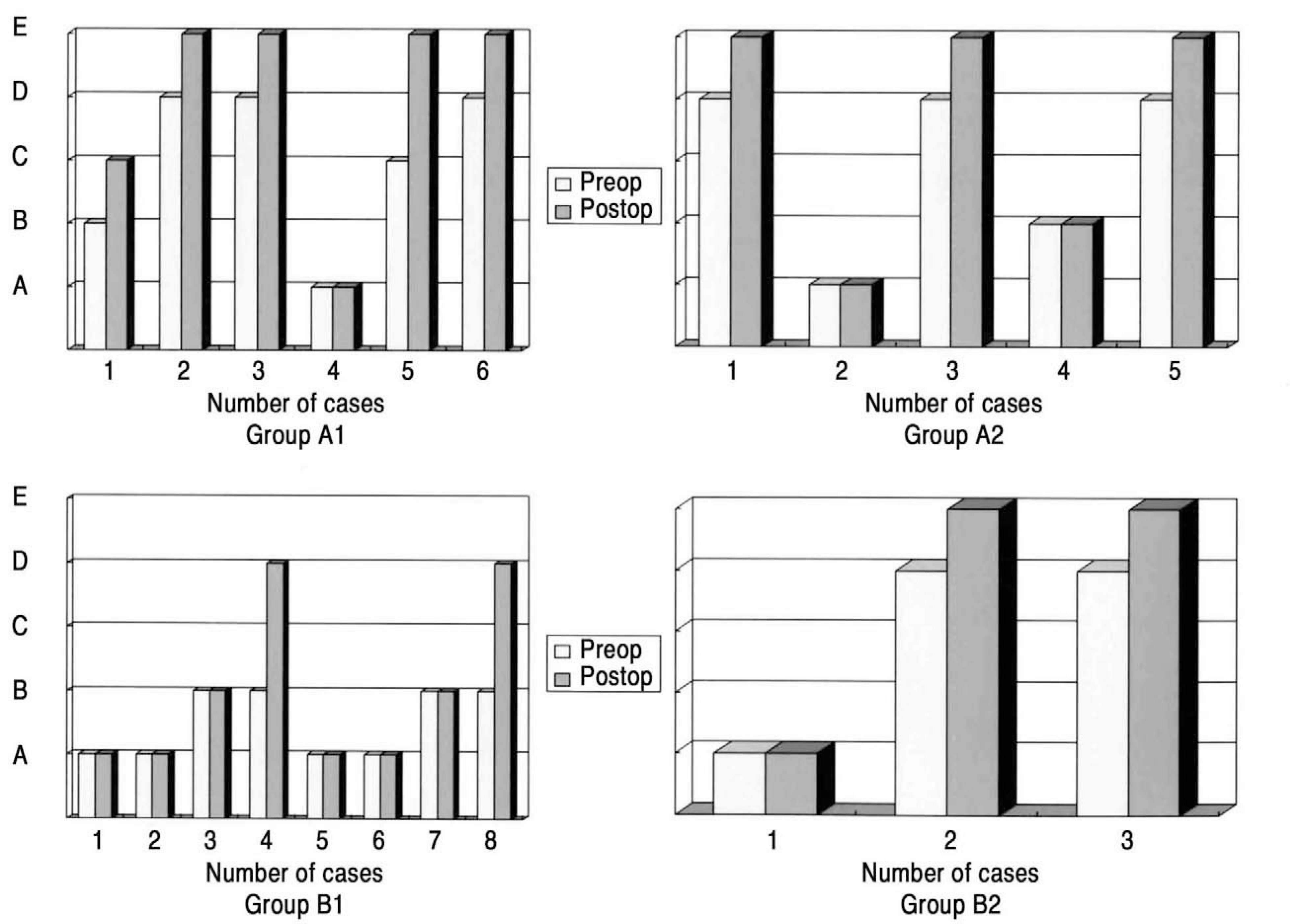
We reviewed the outcomes of 30 patients, who were followed-up for an average of 16 months (range, 12-43 months) after undergoing fusions with anterior cervical plating for distractive-flexion injuries of the lower cervical spine from July 1995 to July 2004. The average age of these patients was 52.9 years (range 24-77 years) and male-to-female ratio was 26:4. Group A consisted of 19 cases that were composed of unilateral dislocations and Group B consisted of 11 cases that were composed of bilateral dislocations based on Allen s classification. Group A1 (9 cases) and B1 (8 cases) were composed of cases that had fractures on the superior end plates or facet joints of the lower cervical spine in each group. Group A2 (10 cases) and B2 (3 cases) were composed of cases without fractures in each group. Neurologic symptoms were evaluated by the Frankel classification; and the angle of lordosis, disc height, and duration of bony union were analyzed postoperatively and with the last follow-up roentgenograms.
RESULTS
Clinically, 22 (73%) patients had neurologic deficits, which were composed of 9 (41%) cases of complete injury, 7 (32%) cases of incomplete injury, and 6 (27%) cases of nerve root injury. The nerve root injuries recovered in all cases and the incomplete injuries had an average 1.7 grade recovery by the Frankel classification. Radiologically, the loss of lordosis was 2.2+/-1.7degrees in group A, 3.1+/-2.8degrees in group B (p=0.359), 3.0+/-1.6degrees in group A1, 1.5+/-1.5degrees in group A2 p=0.048), 3.5+/-3.1degrees in group B1, and 2.1+/-1.7degrees in group B2. Loss of disc height was 1.7+/-1.1 mm in group A, 2.2+/-0.9 mm in group B( p=0.201), 2.2+/-0.9 mm in group A1, 1.2+/-1.0 mm in group A2 (p=0.046), 2.5+/-0.6 mm in group B1, and 1.2+/-1.1 mm in group B2. The duration for bony union was 12.9+/-2.8 weeks in group A, 14.1+/-2.7 weeks in group B (p=0.044), 13.9+/-2.1 weeks in group A1, 11.9+/-3.0 weeks in group A2 (p=0.046), 14.4+/-2.9 weeks in group B1, and 13.3+/-2.3 weeks in group B2. There was no graft displacement, nonunion or metal failure.
CONCLUSION
Anterior cervical plating was an effective treatment modality for distractive-flexion injuries of the lower cervical spine. and more firm method was necessary to surgical treatment in case of fractures on superior end plate or facet joint.
Keyword
MeSH Terms
Figure
Reference
-
01). Vaccaro AR., Cook CM., McCullen G., Garfin SR. Cervical trauma: rationale for selecting the appropriate fusion technique. Orthop Clin North Am. 1998. 29:745–754.02). An HS. Cervical spine trauma. Spine. 1998. 23:2713–2729.
Article03). Olveira JC. Anterior reduction of interlocking facets in the lower cervical spine. Spine. 1979. 4:195–202.
Article04). Coe JD., Warden KE., Sutterlin CE Ⅲ., McAfee PC. Biomechanical evaluation of cervical spinal stabilization methods in a human cadaveric model. Spine. 1989. 14:1122–1131.
Article05). Sutterlin CE Ⅲ., McAfee PC., Warden KE., Rey RM Jr., Farey ID. A biomechanical evaluation of cervical spinal stabilization methods in a bovine model. static and cyclic loading. Spine. 1988. 13:795–802.06). Weis JC., Cunningham BW., Kanayama M., Parker L., McAfee PC. In vitro biomechanical comparison of multi-strand cables with conventional cervical stabilization. Spine. 1996. 21:2108–2114.
Article07). Cybulsky GR., Douglas RA., Meyer PR Jr., Rovin RA. Complications in three-column cervical spine injuries requiring anterior-posterior stabilization. Spine. 1992. 17:253–256.
Article08). Spivak JM., Bharam S., Chen D., Kummer FJ. Internal fixation of cervical trauma following corpectomy and reconstruction. The effects of posterior element injury. Bull Hosp Jt Dis. 2000. 59:47–51.09). Aebi M., Zuber K., Marchesi D. Treatment of cervical spine injuries with anterior plating. Indications, techniques, and results. Spine. 1991. 16:S38–45.10). Ripa DR., Kowall MG., Meyer PR Jr., Rusin JJ. Series of ninety-two traumatic cervical spine injuries stabilized with anterior ASIF plate fusion technique. Spine. 1991. 16:S46–55.
Article11). Goffin J., van Loon J., Van Calenbergh F., Plets C. Long-term results after anterior cervical fusion and osteosynthetic stabilization for fractures and/or dislocations of the cervical spine. J Spinal Disord. 1995. 8:500–508.
Article12). Lifeso RM., Colucci MA. Anterior fusion for rotationally unstable cervical spine fractures. Spine. 2000. 25:2028–2034.
Article13). Song KJ., Lee KB., Kim SR. Availability of anterior cervical plating according to the severity of injury in distractive flexion injury in lower cervical spine. J Korean Orthop Assoc. 2005. 40:195–202.
Article14). Ahn JS., Lee JK., Yang JY., Lee HH. Change of the lordosis on cervical spine after anterior interbody fusion with autogenous iliac strut bone graft. J Korean Soc Spine Surg. 2001. 8:468–474.
Article15). Park HJ., Kim IG., Kim WK. Changes of adjacent segment in anterior cervical fusion. J Korean Soc Spine Surg. 2003. 10:269–276.
Article16). Johnson MG., Fisher CG., Boyd M., Pitzen T., Oxland TR., Dvorak MF. The radiologic failure of single segment anterior cervical plate fixation in traumatic cervical flexion distraction injuries. Spine. 2004. 29:2815–2820.17). Richman JD., Daniel TE., Anderson DD., Miller PL., Douglas RA. Biomechanical evaluation of cervical spine stabilization methods using a porcine model. Spine. 1995. 20:2192–2197.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Distractive Flexion Injury in Lower Cervical Spine using Anterior Cervical Fusion
- Availability of Anterior Cervical Plating According to the Severity of Injury in Distractive Flexion Injury in Lower Cervical Spine
- Delayed Diagnosed Stage 1, 2 Distractive Flexion Injury of the Cervical Spine
- The Treatment of Anterior Plating and Posterior Wiring on Lower Cervical Spine Fracture and Dislocation
- Efficiency of Anterior Interbody Fusion using Cage Packed with DBM in the Distractive Flexion Injury of Cervical Spine: Demineralized Bone Matrix vs Autoiliac Cancellous Bone