J Korean Soc Spine Surg.
2007 Dec;14(4):221-228.
Treatment of Distractive Flexion Injury in Lower Cervical Spine using Anterior Cervical Fusion
- Affiliations
-
- 1Department of Orthopaedic Surgery Yonsei University, Wonju College of Medicine, Wonju, Korea. par73@yonsei.ac.kr
Abstract
-
STUDY DESIGN: A retrospective study.
OBJECTIVES
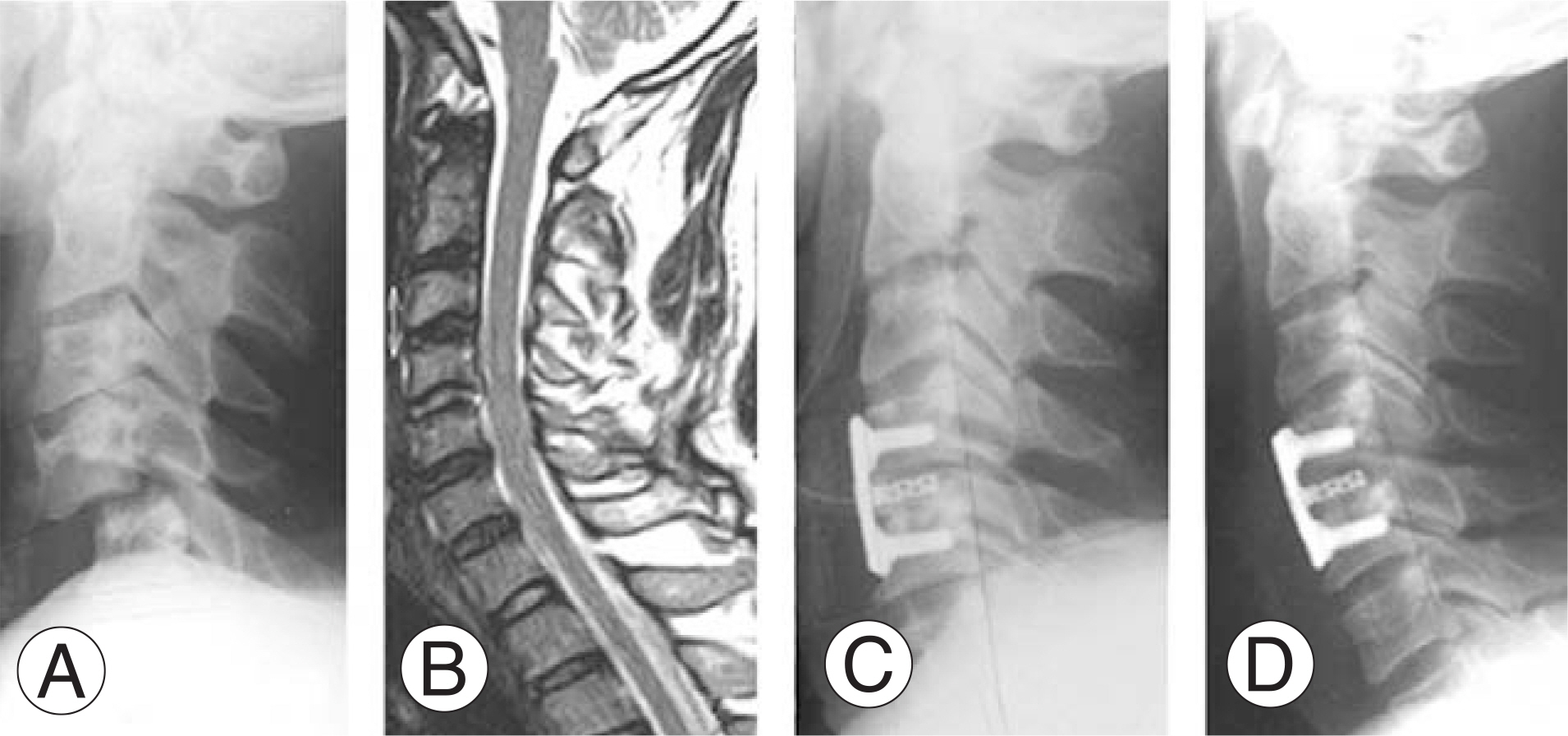
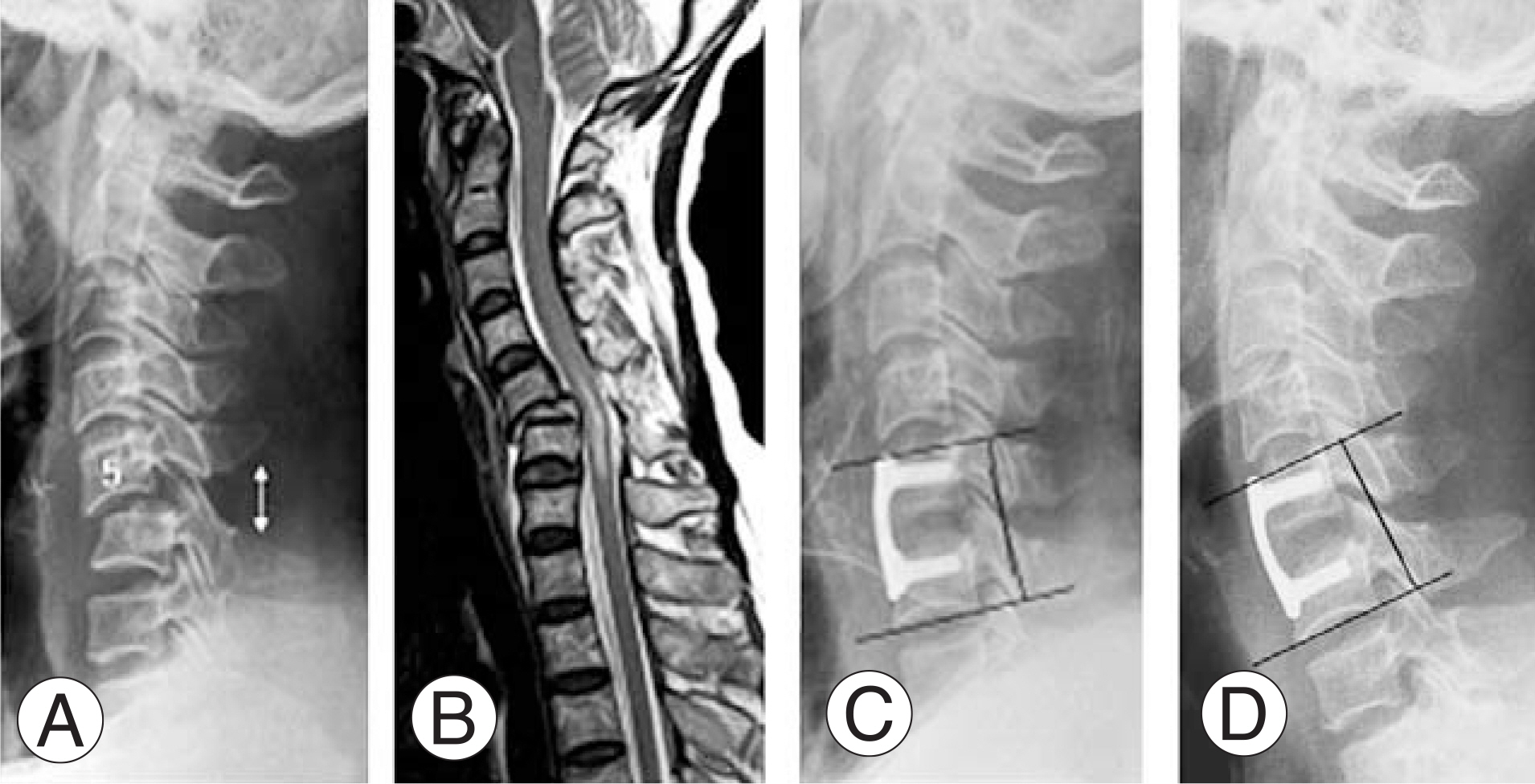
To evaluate the availability of anterior cervical plating in the treatment of distractive flexion injury of the lower cervical spine and the relationship between the neurologic findings, types of dislocation, and disc herniation. SUMMARY OF LITERATURE REVIEW: Anterior stabilization of unstable cervical spine injuries is increasing. However, the stability of anterior stabilization only is controversial for the treatment of bilateral dislocation of the cervical spine. MATERIAL AND METHODS: We retrospectively analyzed 32 patients treated with anterior decompression, auto-iliac bone graft, and anterior cervical plating, who suffered from distractive flexion injury in the lower cervical spine from Feb. 1999 to Feb. 2006. Unilateral dislocation occurred in 21 cases, bilateral dislocation in 11 cases, with evaluation of disc status at the injured level conducted after closed reduction by MRI. We statistically analyzed changes in vertebral body height, disc angle, fusion rate, neurologic recovery, and complications.
RESULTS
All cases were fused by 12.3+/-2.7 weeks after operation, and the loss of anterior and posterior vertebral body height were statistically significant (p=0.00, 0.00), changes in the disc angle were not (p=0.53). Herniation of the disc was more frequent in unilateral dislocation (p=0.02). Clinically 21 (65%) patients had neurologic deficits, but nerve root injuries recovered in all cases, with the original average ASIA motor score of 55.2 improving to 68.3 at last follow up.
CONCLUSIONS
Anterior decompression, bone grafting, and metallic osteosynthesis were effective treatment modalities for distractive-flexion injuries of the lower cervical spine, causing slight vertebral body height decreases but no loss of reduction or neurologic compromise.
MeSH Terms
Figure
Reference
-
1). Yashon D, Tyson G, Vise WM. Rapid closed reduction of cervical fracture-dislocations. Surg Neurol. 1975; 4:513–514.2). Cotler JM, Herbison GJ, Nasuti JF, et al. Closed reduction of traumatic cervical spine dislocation using traction weight up to 140 pounds. Spine. 1993; 18:386–390.3). Cybulsky GR, Douglas RA, Meyer PR Jr, et al. Complication in three column cervical spine injuries requiring anterior-posterior stabilization. Spine. 1992; 17:252–256.4). Henriques T, Olerud C, Bergman A, Jonsson H Jr. Distractive flexion injuries of the subaxial cervical spine treat with anterior plate alone. J Spinal Disord Tech. 2004; 17:1–7.5). Richman JD, Daniel TE, Anderson DD, Miller PL, Douglas RA. Biomechanical evaluation of cervical spine stabilization methods using a porcine model. Spine. 1995; 20:2192–2197.
Article6). Aebi M, Zubber K, Marchesi D. Treatment of cervical spine injuries with anterior plating: Indications, techniques, and results. Spine. 1991; 16:S38–45.7). Adams MS, Crawford NR, Chamberlain RH, Sonntag VK, Dickman CA. Biomechanical comparision of anterior cervical plating and combined anterior/lateral mass plating. Spine. 2001; 1:166–170.8). Goffin J, Van Loon J, Van Calenbergh F, et al. Longterm results after anterior cervical fusion and osteosyn-thetic stabilization for fractures and/or dislocation of the cervical spine. J Spine Disord. 1995; 8:500–508.9). Lifeson RM, Colucci MA. Anterior fusion for rotational-ly unstable cervical spine fractures. Spine. 2000; 25:2028–2034.
Article10). Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958; 40:607–624.
Article11). Fazl M, Pirouzmand F. Intraoperative reduction of locked facets in the cervical spine by use of a modified interlaminar spreader: technical note. Neurosurgery. 2001; 48:444–445.
Article12). Shapiro SA. Management of unilateral locked facet of the cervical spine. Neurosurgery. 1993; 33:832–837.
Article13). Do Koh Y, Lim TH Won You J, et al. A biomechanical comparison of modern anterior and posterior plate fixation of the cervical spine. Spine. 2001; 26:15–21.
Article14). Vaccaro AR, Madigan L, Schweitzer ME, Flanders AE, Hilbrand AS, Albert TJ. Magnetic resonance imaging analysis of soft tissue disruption after flexion-distraction injuries of the subaxial cervical spine. Spine. 2001; 17:1866–1872.
Article15). Ulrich C, Worsdorfer O, Claes L, Magerl F. Comparative study of the stability of anterior and posterior cervical spine fixation procedures. Arch Orthop Trauma Surg. 1987; 106:226–231.
Article16). Coe JD, Warden KE, Sutterlin CE 3rd, McAfee PC. Biomechanical evaluation of cervical spinal stabilization methods in human cadaveric model. Spine. 1989; 14:1122–1131.17). Song KJ, Lee KB, Kim SR. Availability of anterior cervical plating according to the severity of injury in distractive flexion injury in lower cervical spine. J Korean Orthop Assoc. 2005; 40:195–202.
Article18). Rizzolo SJ, Piazza HR, Colter JH, Balderston RA, Schaefer D, Flamders AH. Intervertebral disc injury complicating cervical spine trauma. Spine. 1991; 16:S187–189.
Article19). Argenson C, Lovet J, Sansouiller JL, de Peretti F. Traumatic rotatory displacement of the lower cervical spine. Spine. 1988; 13:767–773.
Article20). Burke CD, Berryman D. The place of closed manipulation in the management of flexion-rotation dislocations of the cervical spine. J Bone Joint Surg Br. 1971; 53:165–182.
Article21). Sim E, Vaccaro AR, Berzlanovich A, Schwarz N, Sim B. In vitro genesis of subaxial cervical unilateral facet dislocations through sequential soft tissue ablation. Spine. 2001; 26:1317–1323.
Article22). Doran SE, Papadopoulos SM, Ducker TB, et al. Magnetic resonance imaging documentation of coexistent traumatic locked facets of the cervical spine and disc herniation. J Neurosurg. 1993; 79:341–345.
Article23). Eismont FJ, Arena MJ, Green BA. Extrusion of an intervertebral disc associated with traumatic subluxation or dislocation of cervical facets: case report. J bone Joint Surg Am. 1991; 73:1555–1560.
Article24). Robertson PA, Ryan MD. Neurological deterioration after reduction of cervical subluxation: mechanical compression by disc tissue. J Bone Joint Surg Br. 1992; 74:224–227.
Article25). Darsaut TE, Ashforth R, Bhargava R, et al. A pilot study of magnetic resonance imaging-guided closed reduction of cervical spine fractures. Spine. 2006; 31:2085–2090.
Article26). Reindl R, Ouellet J, Harvey EJ, Berry G, Arlet V. Anterior reduction for cervical spine dislocation. Spine. 2006; 31:648–652.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Availability of Anterior Cervical Plating According to the Severity of Injury in Distractive Flexion Injury in Lower Cervical Spine
- Delayed Diagnosed Stage 1, 2 Distractive Flexion Injury of the Cervical Spine
- Fracture and Bilateral Facet Dislocation after Anterior Cervical Fusion in a Patient with a Distraction-Flexion Injury at the Lower Cervical Level
- Surgical Treatment of the Unstable Lower Cervical Spine Injuries
- Efficiency of Anterior Interbody Fusion using Cage and Plate in the Distractive Flexion Injury of Cervical Spine : Cage vs Tricortical Autoiliac Bone