J Korean Soc Spine Surg.
2013 Mar;20(1):28-33. 10.4184/jkss.2013.20.1.28.
Usefulness of the ProSet MRI for Diagnosis of the Extraforaminal Disc Herniation
- Affiliations
-
- 1Department of Orthopaedic Surgery, Yeungnam University Hospital, Daegu, South Korea. mwahn@med.yu.ac.kr
- KMID: 2209498
- DOI: http://doi.org/10.4184/jkss.2013.20.1.28
Abstract
- STUDY DESIGN: This is a retrospective study.
OBJECTIVES
The purpose of this study is to confirm the clinical usefulness of utilizing ProSet imaging for checking the nerve root compression and swelling in extraforaminal disc herniation. SUMMARY OF LITERATURE REVIEW: Diagnosing extraforaminal disc herniations can be neglected with using a conventional MRI.
MATERIALS AND METHODS
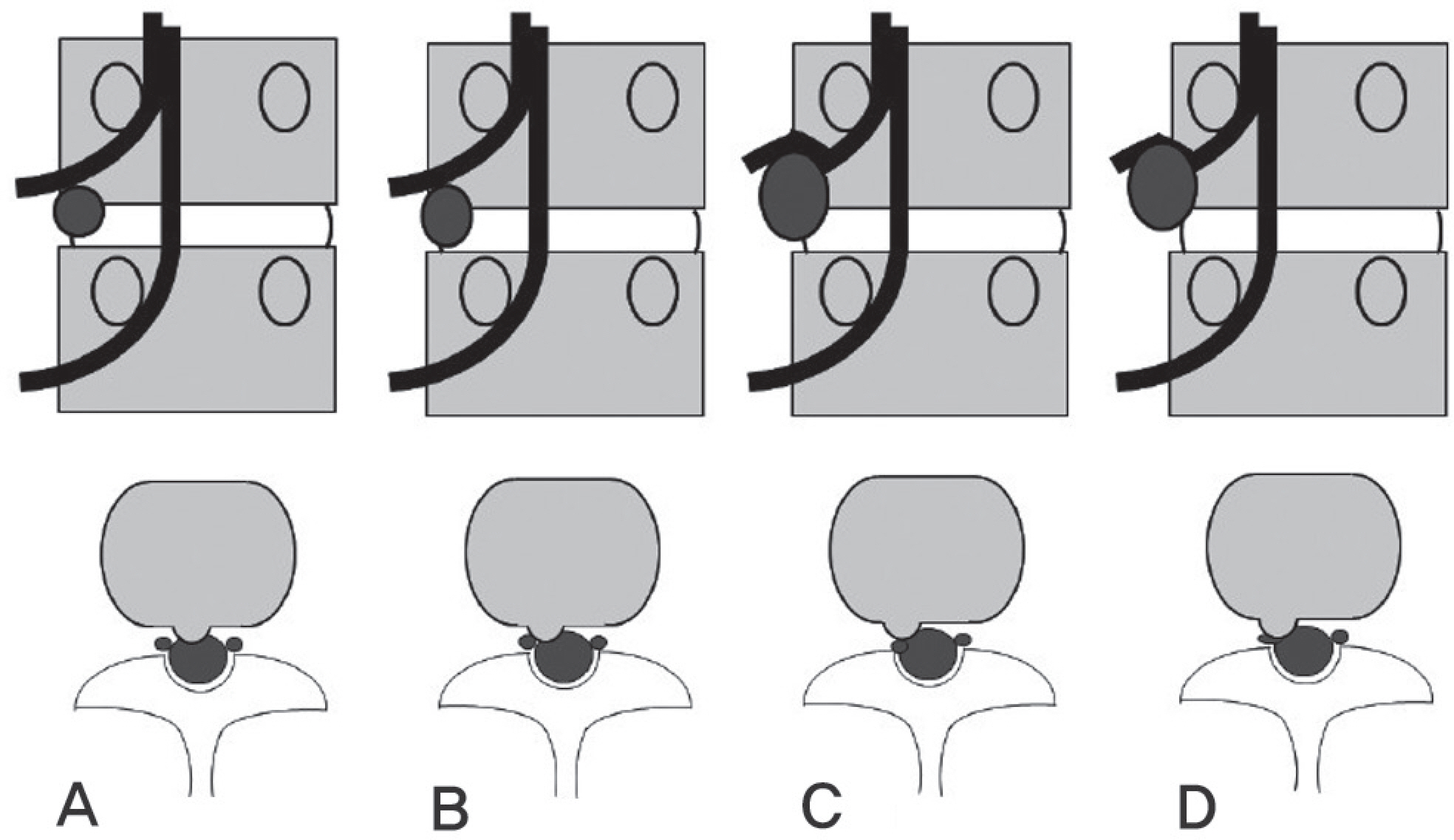
A retrospective analysis was performed on 25 patients, who underwent both conventional & Principles of the selective excitation technique (ProSet) MR imaging for the evaluation of extraforaminal disc herniation, from April 2008 to October 2010. Radiographic analysis was based on the notion that the degree of nerve root compression and swelling was decided by Pfirrmann's classification.
RESULTS
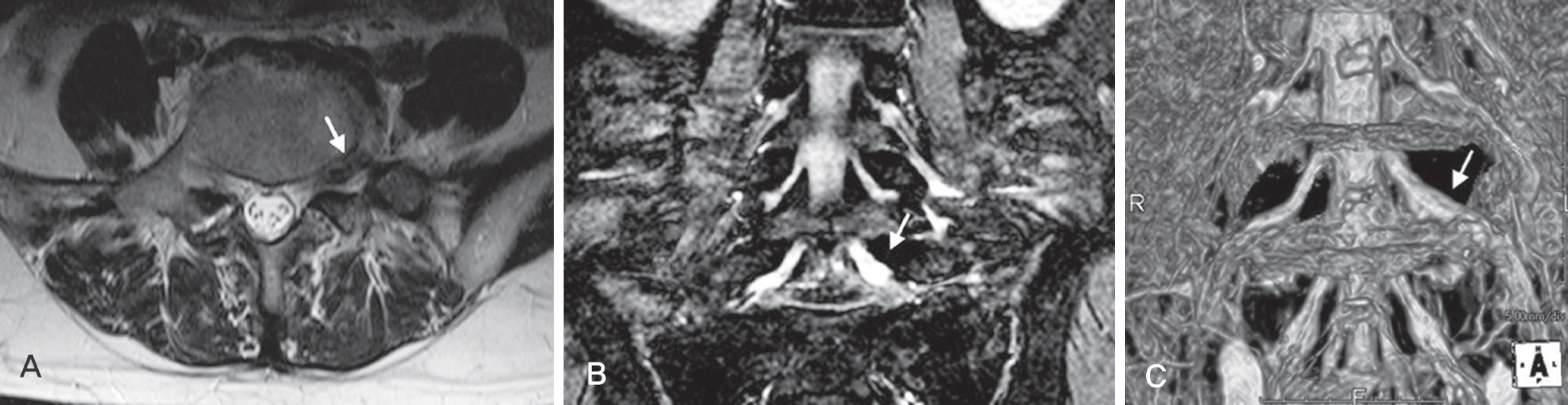
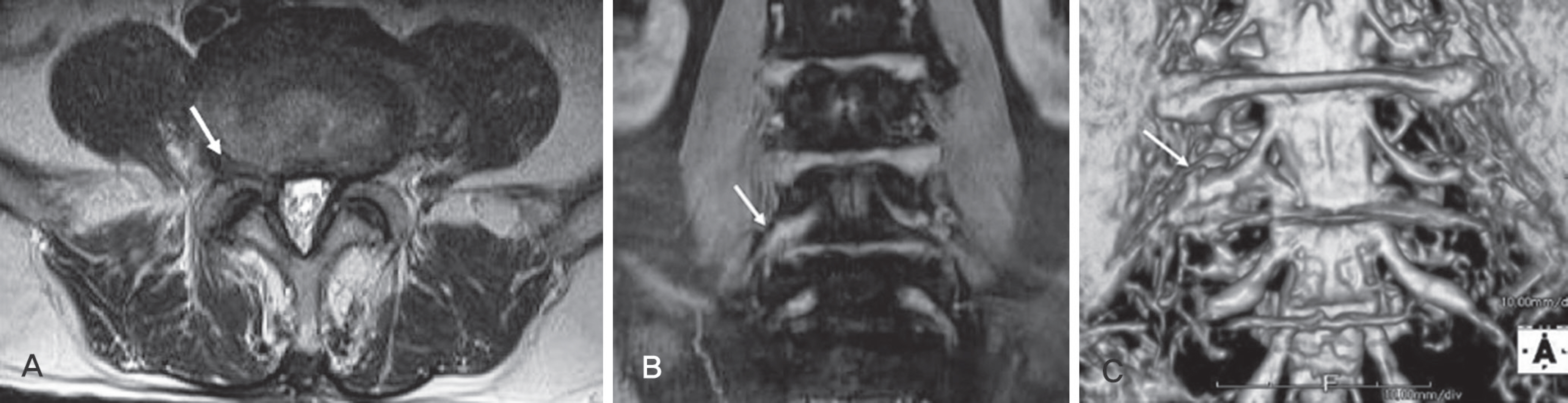
Severe compression in the ProSet 3D rendering image was observed in 21 subjects, as compared with 8 subjects in the conventional axial image. Especially, nothing was ever detected in the conventional sagittal image. Severe compression in the ProSet 3D rendering image was observed in 4 subjects, while their nerve root compression was not clear in the conventional axial image. Severe compression and severe swelling in the ProSet 3D & coronal image was observed in 15 subjects, while their nerve root compression was none or not clear in the conventional sagittal image. The swelling degree of the ProSet coronal image turned out bigger than the swelling degree of conventional axial image, and the signal intensity change was also obvious.
CONCLUSIONS
ProSet imaging is regarded useful to investigate the symptom triggering nerves, because ProSet image not only observes better nerve root compression, but also identifies the swelling degree more easily than that of the conventional magnetic resonance imaging (MRI).
Keyword
Figure
Cited by 1 articles
-
Relative Risk of Operation between Lumbar Far Lateral Disc Herniation and Posterolateral Disc Herniation: A Retrospective Cohort Study
Dae Ho Ha, Dae Moo Shim, Tae Kyun Kim, Sung Kyun Oh, Jin Kim
J Korean Orthop Assoc. 2017;52(5):442-447. doi: 10.4055/jkoa.2017.52.5.442.
Reference
-
1.Benini A. Der Zugang zu den lateralen lumbalen diskush-ernien ambeispiel einer hernie L4/L5. Operat Orthop Trau-matol. 1988. 10:103–16.2.Ohmori K., Kanamori M., Kawaguchi Y., Ishihara H., Kimura T. Clinical features of extraforaminal lumbar disc herniation based on the radiographic location of the dorsal root ganglion. Spine (Phila Pa 1976). 2001. 26:662–6.
Article3.Jackson RP., Clah JJ. Foraminal and extraforaminal lumbar disc herniation: Diagnosis and treatment. Spine (Phila Pa 1976). 1987. 12:577–85.
Article4.Junichi K., Mitsuo H. Diagnosis and operative treatment of intraforaminal & extraforaminal nerve root compression. Spine (Phila Pa 1976). 1991. 16:1312–20.5.Macnab I. Negative disc exploration: An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg. 1971. 53:891–903.6.Abdullah AF., Ditton EW III., Byrd EB. Extreme-lateral lumbar disc herniations: Clinical syndrome and special problems of diagnosis. J Neusurg. 1974. 41:229–34.7.Kim MH., Suh KJ., Lee JY., Min SH., Yoo HY. Usefulness of Coronal MR Image in Diagnosis of Foraminal and Extraforaminal Disc Herniation. J Korean Soc Spine Surg. 2008. 15:165–73.
Article8.Pfirrmann CW., Dora C., Schmid MR., Zanetti M., Holdler J., Boos N. MR image-based grading of lumbar nerve root compromise due to disk herniation: Reliability study with surgical correlation. Radiology. 2004. 230:583–8.
Article9.Lindblom K. Protrusions of disks and nerve compression in the lumbar region. Acta Radiol. 1944. 25:195–212.
Article10.Bronx NY. Foraminal and far lateral lumbar disc herniations: Surgical alternatives outcome measures. Spinal Cord. 2002. 40:491–500.11.Faust SE., Ducker TB., VanHassent JA. Lateral lumbar disc herniations. J Spinal Disord. 1992. 5:97–103.
Article12.Lee CK., Rauschning W., Glenn W. Lateral lumbar canal stenosis: Classification, pathologic anatomy and surgical decompression. Spine (Phila Pa 1976). 1988. 13:313–20.13.Forristal RM., Marsh HO., Pay NT. MRI & CT of the lumbar spine: Comparison of diagnotic methods and correlation with surgical findings. Spine (Phila Pa 1976). 1988. 13:1049–54.14.Byun WM., Kin JW., Lee JK. Differentiation between symptomatic and asymptomatic extraforaminal stenosis in lum-bosacral transitional vertebra: role of three-dimensional magnetic resonance lumbosacral radiculography. Korean J Radiol. 2012. 13:403–11.
Article15.Byun WM., Ahn SH., Ahn MW. Value of 3D MR lum-bosacral radiculopathy in the diagnosis of symptomatic chemical radiculitis. Am J Neuroradiol. 2012. 33:529–34.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of Coronal MR Image in Diagnosis of Foraminal and Extraforaminal Disc Herniation
- Reliability of MRI findings for Symptomatic Extraforaminal Disc Herniation in Lumbar Spine
- Paramedian Tangential Approach for the Lumbosacral Extraforaminal Disc Herniations
- Usefulness of Three Dimensional Proset MR Images for Diagnosis of Symptomatic L5-S1 Foraminal and Extraforaminal Stenosis
- Diagnosis of Lumbar Lateral Disc Herniation: Value of Magnetic Resonance Imaging Revisited