J Korean Soc Spine Surg.
2005 Mar;12(1):28-38. 10.4184/jkss.2005.12.1.28.
Diagnosis of Lumbar Lateral Disc Herniation: Value of Magnetic Resonance Imaging Revisited
- Affiliations
-
- 1Department of Orthopaedic Surgery, Seoul National University College of Medicine, Seoul, Korea. ortho@hananet.net
- 2Department of Radiology, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 1897018
- DOI: http://doi.org/10.4184/jkss.2005.12.1.28
Abstract
- STUDY DESIGN: We retrospectively evaluated the value of magnetic resonance imaging (MRI) in the diagnosis of lumbar lateral disc herniations.
SUMMARY OF LITERATURE REVIEW: MRI is known to be a reliable study for the diagnosis of a lumbar disc herniation. However, recent studies of its diagnostic value for lateral disc herniation have been rare.
OBJECTIVES
We aimed to assess the diagnostic value of simple MRI, to determine the need for additional imaging studies and to investigate mimicking lesions.
MATERIALS AND METHODS
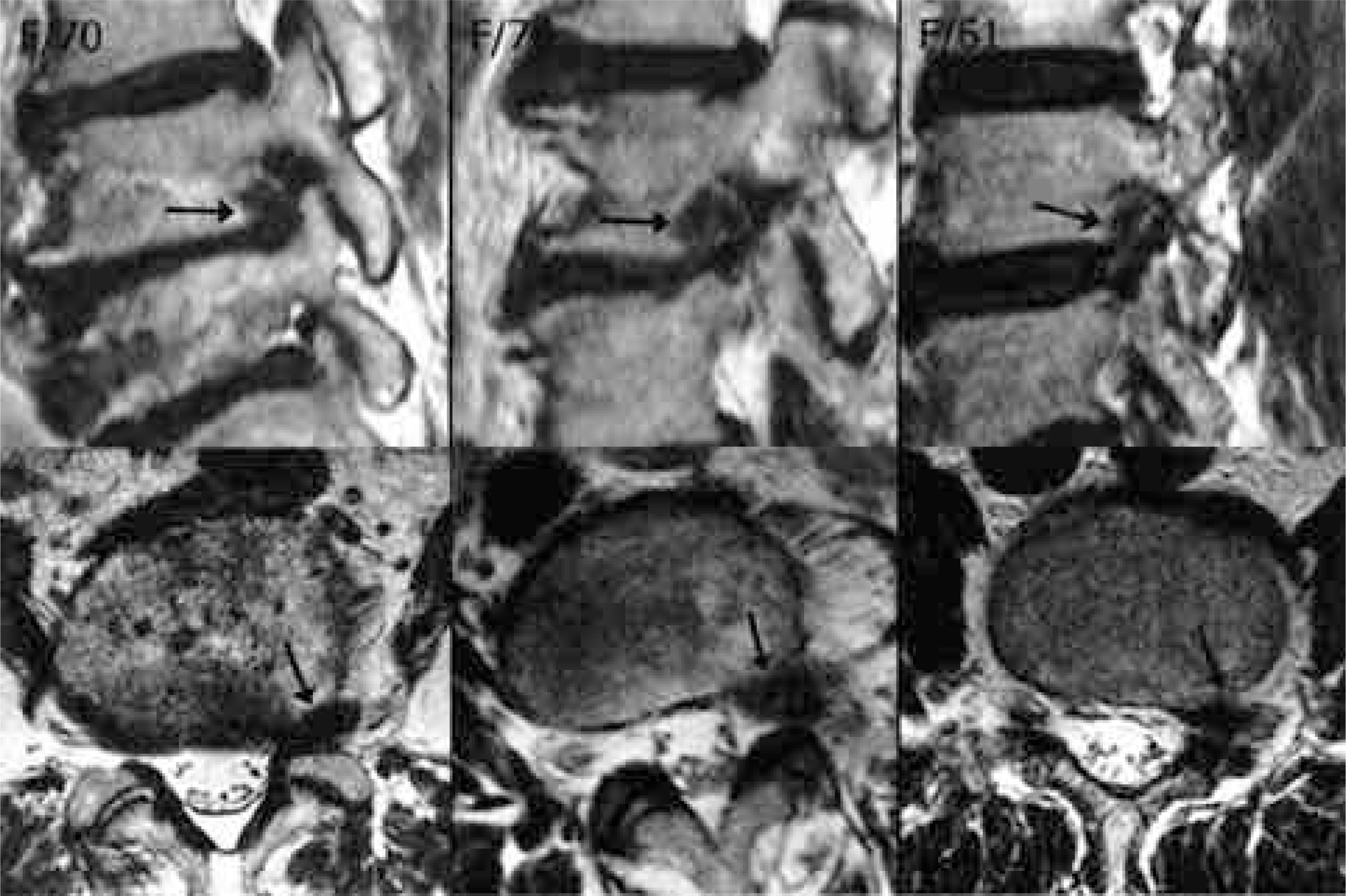
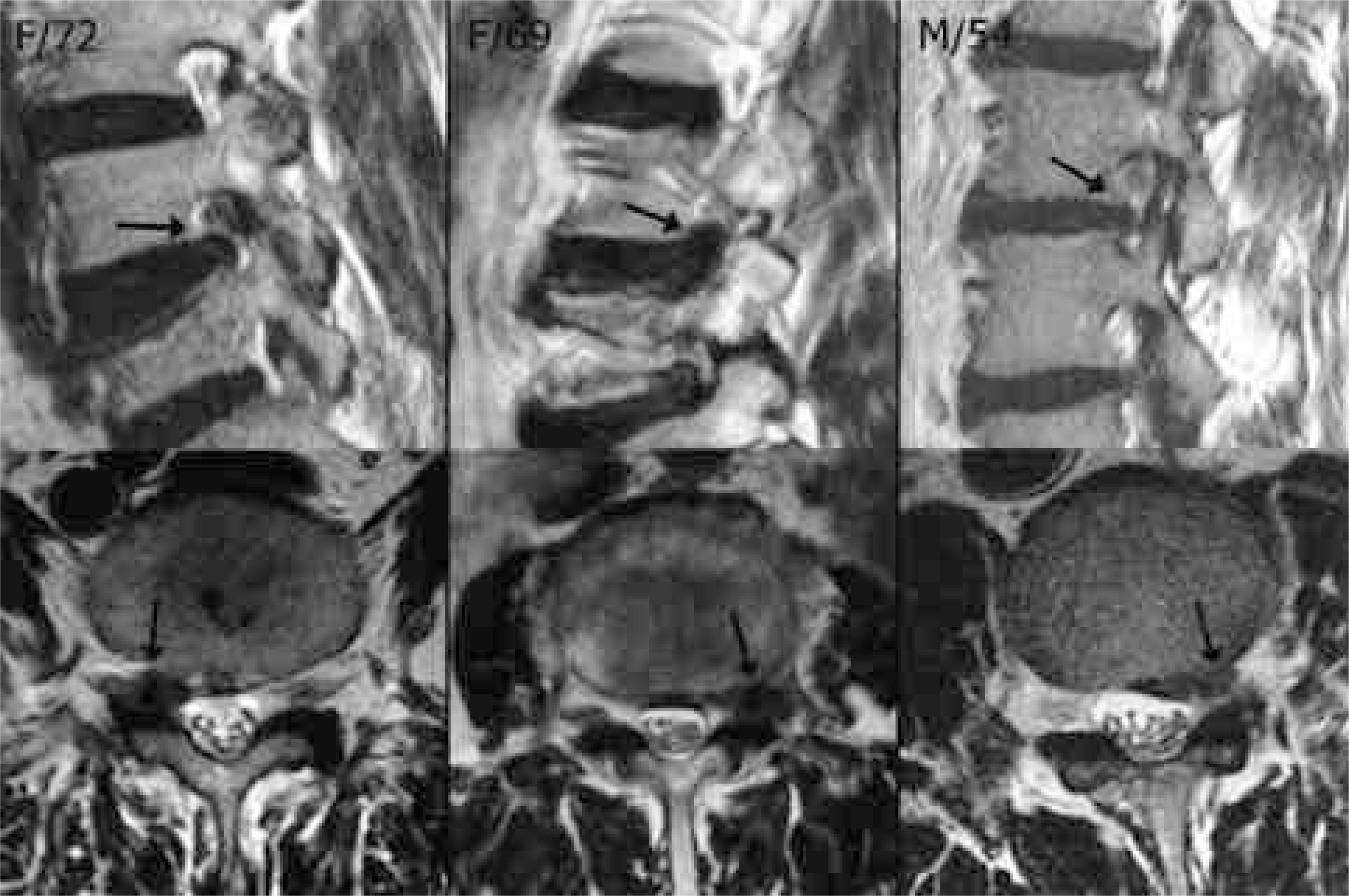
In a lateral herniation group composed of 21 cases, including 10 foraminal and 11 extraforaminal herniations, the diagnostic value of simple MRI was evaluated, and the potential requirement for additional studies investigated. In a mimicking lesion group(5 cases), the entity of each lesion was identified.
RESULTS
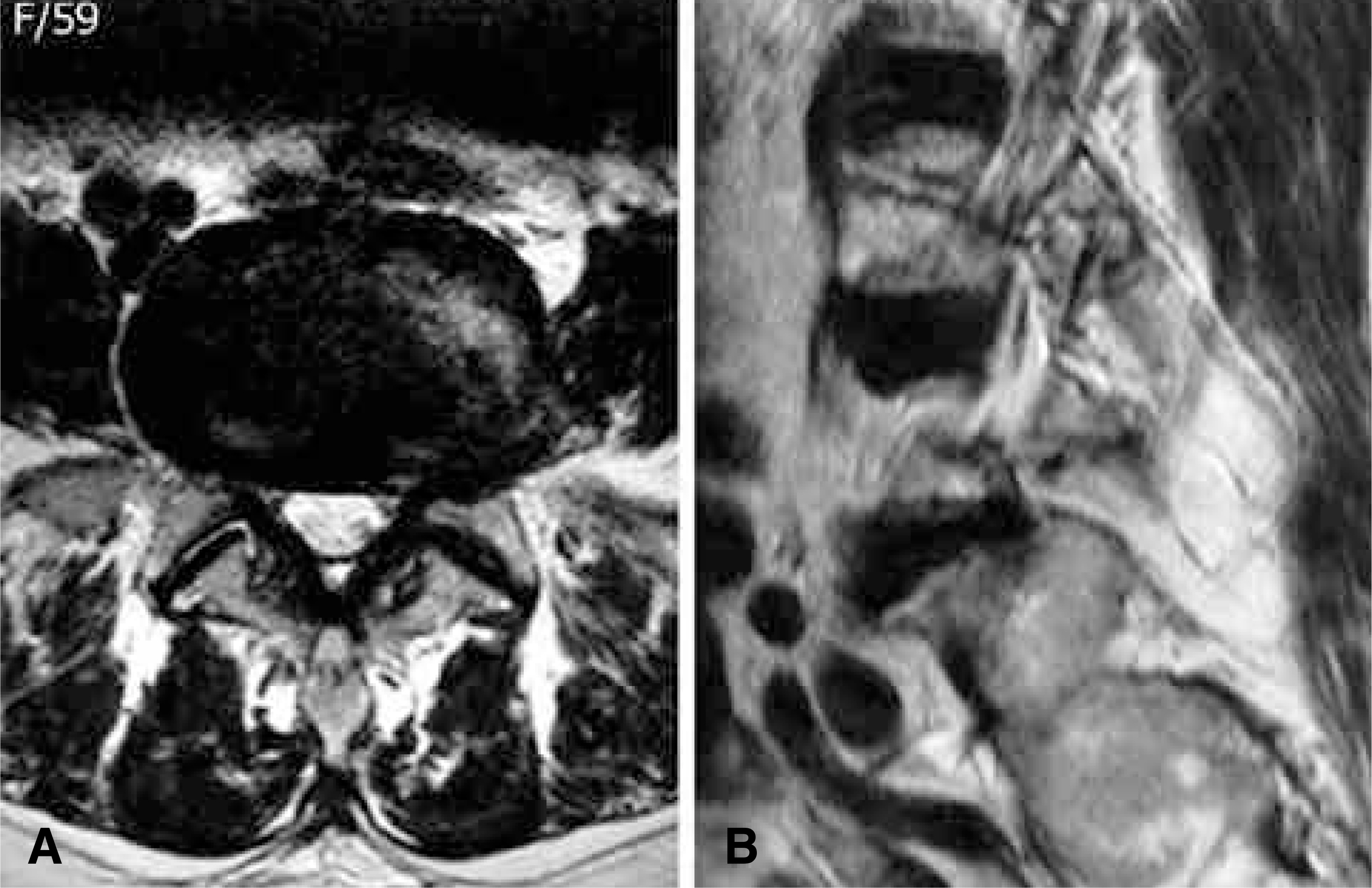
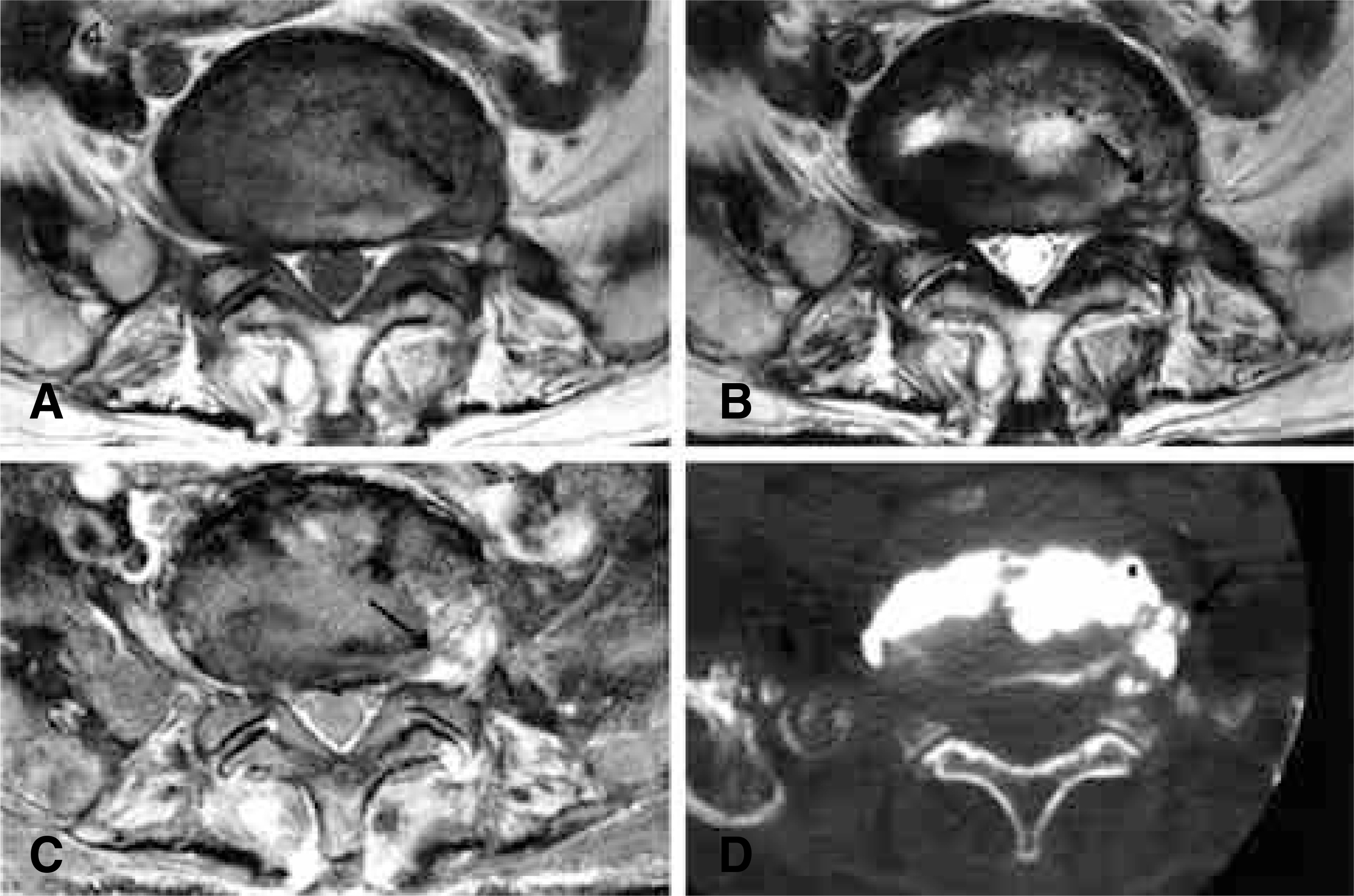
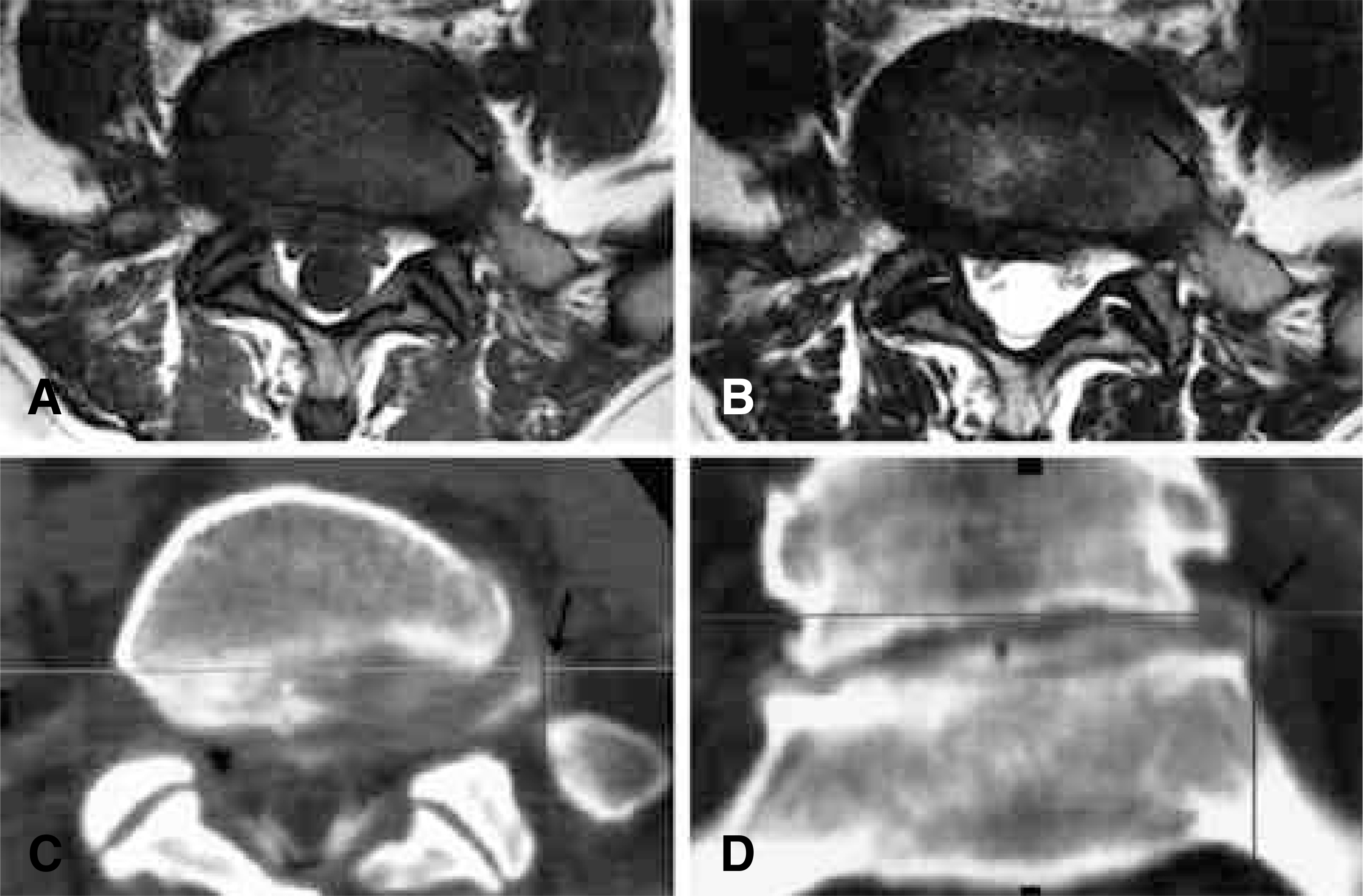
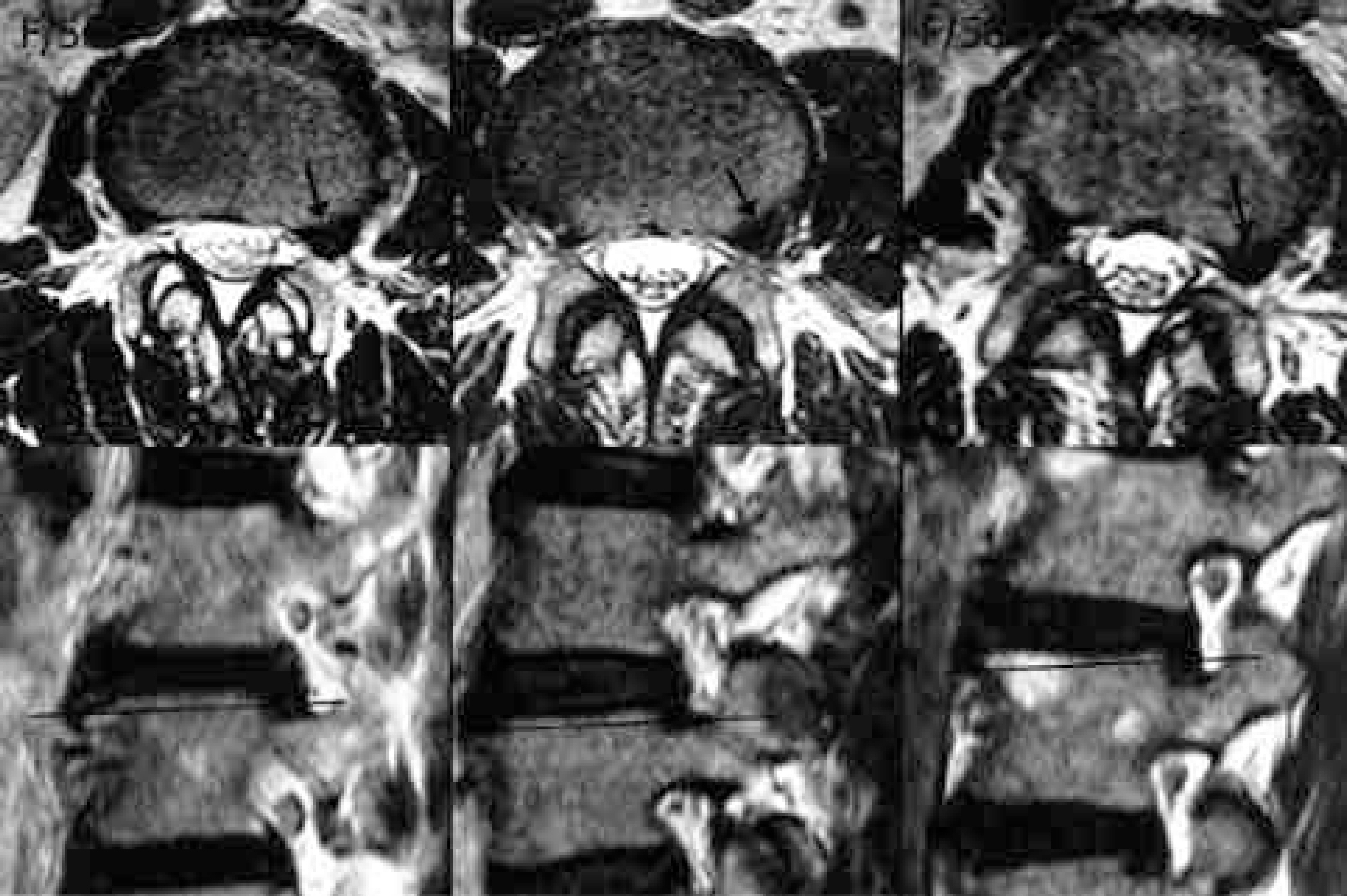
All 10 foraminal disc herniation cases were able to be confirmed with simple MRI, six of which were confirmed using sagittal images alone. In contrast, for the eleven extraforaminal disc herniations, sagittal MR images were not at all helpful in the diagnosis; however, six(55%) were confirmed from axial images, but the other five could not be confirmed until additional studies, such as enhanced MRI(4 cases), 1 mm-sliced CT (1) and CT-discography (3), were carried out. All 5 mimicking lesions were upper endplates of the lower vertebrae.
CONCLUSIONS
Simple MRI is useful in the diagnosis of foraminal herniations, but not so helpful for extraforaminal herniations; particularly, sagittal images are of little use. Therefore, whenever a patient complaining of severe radiating pain presents with no causative finding on simple MRI, the extraforaminal regions on the axial images should be diligently scrutinized again, and additional studies considered when necessary. Conversely, mimicking lesions, such as an upper endplate, should be differentiated when a lateral disc herniation is suspected.
Figure
Cited by 1 articles
-
Inter- and Intra-observer Reliability of MRI for Lumbar Lateral Disc Herniation
Seong Wan Kim, Jin S. Yeom, Seong Kyu Park, Bong Soon Chang, Dong-Ho Lee, Jae Hyup Lee, Kun-Woo Park, Eun Seok Seo, Choon-Ki Lee
Clin Orthop Surg. 2009;1(1):34-39. doi: 10.4055/cios.2009.1.1.34.
Reference
-
1). Abdullah AF, Ditton EW III, Byrd EB. Extreme-lateral lumbar disc herniations: clinical syndrome and special problems of diagnosis. J Neurosurg. 1974; 41:229–234.2). Antuaco EJC, Holder JC, Boop WC, Binet EF. Computed tomographic diagnosis in the evaluation of extreme lateral disc herniation. Neurosurgery. 1984; 14:350–352.3). Benini A. Der Zugang zu den lateralen lumbalen diskush -ernien am beispiel einer hernie L4/L5. Operat Orthop Traumatol. 1988; 10:103–116. (cited from Greiner-Perth R, Bohm H, Allam Y: A new technique for the treatment of lumbar far lateral disc herniation: technical note and preliminary results. Eur Spine J. 2003; 12:320–324. .).4). Jackson RP, Clah JJ. Foraminal and extraforaminal lumbar disc herniation: Diagnosis and treatment. Spine. 1987; 12:577–585.
Article5). Kornberg M. Extreme lateral lumbar disc herniations: clinical syndrome and computed tomography recognition. Spine. 1987; 12:586–589.6). Lindblom K. Protrusions of disks and nerve compression in the lumbar region. Acta Radiol. 1944; 25:195–212.
Article7). Macnab I. Negative disc exploration: an analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg. 1971; 53-A:891–903.8). Maroon JC, Kopitnik TA, Schulhof LA, Abla A, Wilberger JE. Diagnosis and microsurgical approach to far-lateral disc herniation in the lumbar spine. J Neurosurg. 1990; 72:378–382.
Article9). O'Hara LJ, Marshall RW. Far lateral lumbar disc herniation. The key to the intertransverse approach. J Bone Joint Surg. 1997; 79-B:943–947.10). Ohmori K, Kanamori M, Kawaguchi Y, Ishihara H, Kimura T. Clinical features of extraforaminal lumbar disc herniation based on the radiographic location of the dorsal root ganglion. Spine. 2001; 26:662–666.
Article11). Osborn AG, Hood RS, Sherry RG. CT/MR spectrum of far lateral and anterior lumbosacral disk herniations. Am J Neuroradiol. 1998; 9:775–778.12). Patrick BS. Extreme lateral ruptures of lumbar intervertebral discs. Surg Neurol. 1975; 3:301–304.13). Schlesinger SM, Fankhauser H, de Tribolet N. Microsurgical anatomy and operative technique for extreme lateral lumbar disc herniations. Acta Neurochir (Wien). 1992; 118:117–129.
Article14). Segnarbieux F, Van de Kelft E, Candon E, Bitoun J, Frerebeau P. Disco-computed tomography in extraforaminal and foraminal lumbar disc herniation: influence on surgical approaches. Neurosurgery. 1994; 34:643–647.15). Williams AL, Haughton VM, Daniels DL, Thornton RS. CT recognition of lateral lumbar disk herniation. Am J Roentgenol. 1982; 139:345–347.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cervical Far Lateral Disc Herniation-Case Report-
- Spinal Nerve Root Swelling Mimicking Intervertebral Disc Herniation in Magnetic Resonance Imaging: A Case Report
- The Relationship between the Lower Lumbar Disc Herniation and the Morphology of the Iliolumbar Ligaments Using Magnetic Resonance Imaging
- The Role of CT Discography in Far Lateral Disk Herniation
- Ordinary Disc Herniation Changing into Posterior Epidural Migration of Lumbar Disc Fragments Confirmed by Magnetic Resonance Imaging: A Case Report of a Successful Endoscopic Treatment