J Korean Soc Radiol.
2013 Aug;69(2):157-163. 10.3348/jksr.2013.69.2.157.
Ultrasonographic Findings of Torsed Testicular Appendages in Prepubertal Children
- Affiliations
-
- 1Department of Radiology, SMG-SNU Boramae Medical Center, Seoul, Korea. susemi513@hanmail.net
- KMID: 2208821
- DOI: http://doi.org/10.3348/jksr.2013.69.2.157
Abstract
- PURPOSE
To characterize the sonographic findings of torsed testicular appendages and to evaluate the sonographic findings in making erroneous diagnosis of epididymitis or torsion of testis in prepubertal children.
MATERIALS AND METHODS
From June 2010 to November 2012, we retrospectively analyzed the duplex sonography of fifteen children with torsion of testicular appendages. The presence or absence of the extratesticular nodule and secondary inflammatory changes were evaluated. Six patients had follow-up sonography and two patients underwent surgery.
RESULTS
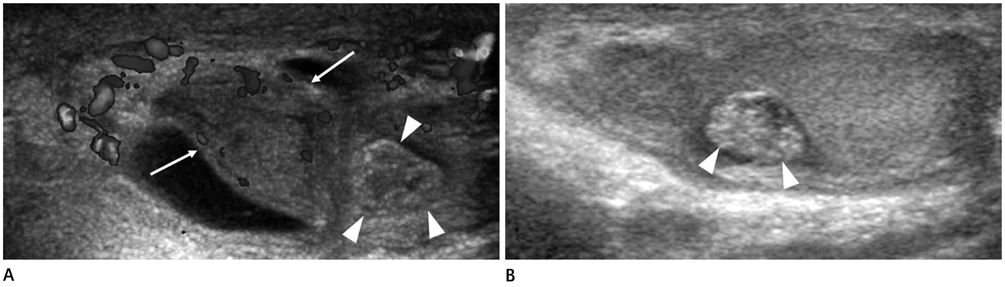
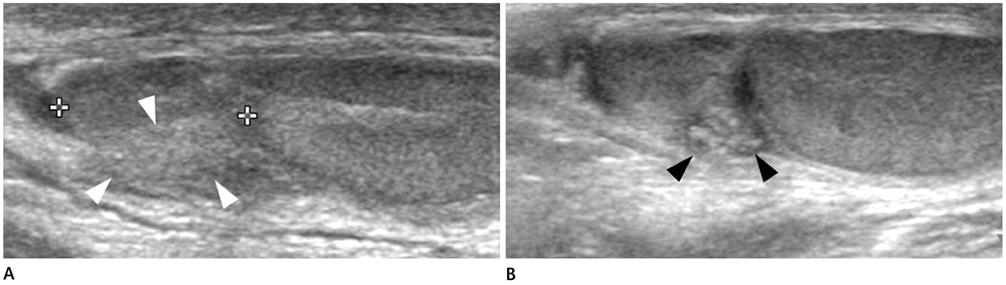
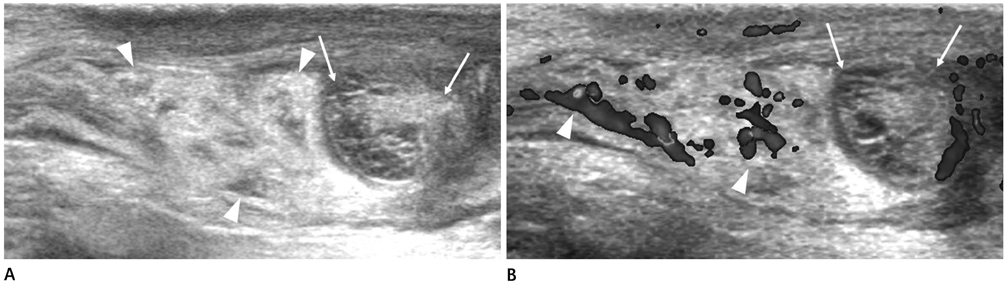
Sonography demonstrated the extratesticular nodule in 13 (87%) children. Four of these 13 children were misdiagnosed as epididymitis due to imperceptions of the nodule. Out of remaining two (13%) children without the nodule, one mimicked epididymitis and the other was misdiagnosed as torsion of testis. Secondary inflammatory changes included enlarged epididymis in 14 children (93%), scrotal wall edema in 11 (73%), hydrocele in 10 (67%), and enlarged testis in 3 (20%).
CONCLUSION
Ultrasonographic findings of secondary inflammatory changes in the absence or imperception of the nodules for epididymo-testicular groove or epididymal head may suggest an erroneous diagnosis of epididymitis or torsion of testis in children with torsed testicular appendages. Meticulous evaluation for the nodule is important when differentiating the torsed testicular appendages from the two entities of prepubertal children.
MeSH Terms
Figure
Reference
-
1. Strauss S, Faingold R, Manor H. Torsion of the testicular appendages: sonographic appearance. J Ultrasound Med. 1997; 16:189–192. quiz 193-194.2. Baldisserotto M, de Souza JC, Pertence AP, Dora MD. Color Doppler sonography of normal and torsed testicular appendages in children. AJR Am J Roentgenol. 2005; 184:1287–1292.3. Karmazyn B, Steinberg R, Livne P, Kornreich L, Grozovski S, Schwarz M, et al. Duplex sonographic findings in children with torsion of the testicular appendages: overlap with epididymitis and epididymoorchitis. J Pediatr Surg. 2006; 41:500–504.4. Atkinson GO Jr, Patrick LE, Ball TI Jr, Stephenson CA, Broecker BH, Woodard JR. The normal and abnormal scrotum in children: evaluation with color Doppler sonography. AJR Am J Roentgenol. 1992; 158:613–617.5. Sellars ME, Sidhu PS. Ultrasound appearances of the testicular appendages: pictorial review. Eur Radiol. 2003; 13:127–135.6. Siegel MJ. Male genital tract. In : Siegel MJ, editor. Pediatric sonography. Philadelphia: Lippincott Williams & Wilkins;2002. p. 579–624.7. Kadish HA, Bolte RG. A retrospective review of pediatric patients with epididymitis, testicular torsion, and torsion of testicular appendages. Pediatrics. 1998; 102(1 Pt 1):73–76.8. Kass EJ, Lundak B. The acute scrotum. Pediatr Clin North Am. 1997; 44:1251–1266.9. Hesser U, Rosenborg M, Gierup J, Karpe B, Nyström A, Hedenborg L. Gray-scale sonography in torsion of the testicular appendages. Pediatr Radiol. 1993; 23:529–532.10. McCombe AW, Scobie WG. Torsion of scrotal contents in children. Br J Urol. 1988; 61:148–150.11. Park SJ, Lee HK, Yi BH, Cha JG, Joh JH, Hong HS, et al. Manual reduction of torsion of an intrascrotal appendage under ultrasonographic monitoring. J Ultrasound Med. 2007; 26:293–299.12. Johnson KA, Dewbury KC. Ultrasound imaging of the appendix testis and appendix epididymis. Clin Radiol. 1996; 51:335–337.13. Park SJ, Kim HL, Yi BH. Sonography of intrascrotal appendage torsion: varying echogenicity of the torsed appendage according to the time from onset. J Ultrasound Med. 2011; 30:1391–1396.14. Frush DP, Sheldon CA. Diagnostic imaging for pediatric scrotal disorders. Radiographics. 1998; 18:969–985.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasonography of intrascrotal torsed appendages: size and interval between symptom onset and the ultrasonographic examination according to echogenicity
- Early exploration of acute scrotum in children
- Overview of Pediatric Testicular Tumors in Korea
- Penile circumference and stretched penile length in prepubertal children: A retrospective, single-center pilot study
- Ultrasonographic Findings of Prepubertal Testicular Teratoma