Korean J Urol.
2014 Dec;55(12):789-796. 10.4111/kju.2014.55.12.789.
Overview of Pediatric Testicular Tumors in Korea
- Affiliations
-
- 1Department of Urology, Pusan National University School of Medicine, Yangsan, Korea. lsd@pusan.ac.kr
- KMID: 2070092
- DOI: http://doi.org/10.4111/kju.2014.55.12.789
Abstract
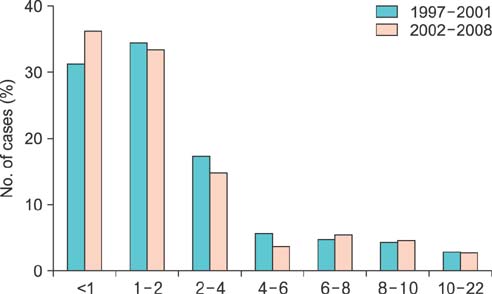
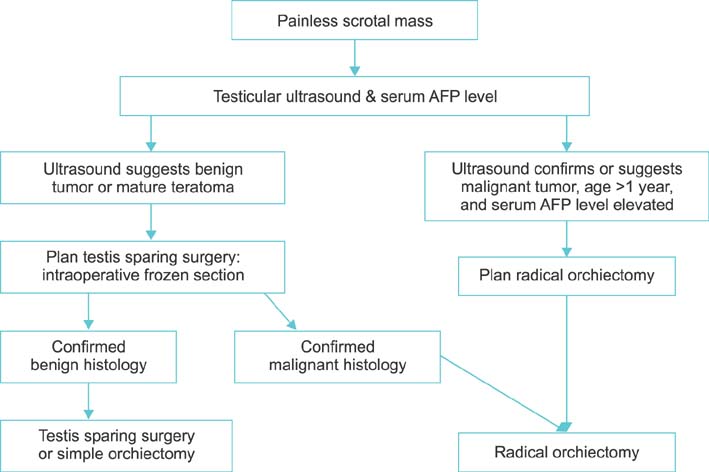
- Prepubertal testicular tumors are rare compared with postpubertal testicular tumors. The incidence of prepubertal testicular tumors peaks at 2 years of age, tapers off after 4 years of age, and then begins to rise again at puberty. Prepubertal and postpubertal testicular tumors show many differences, including the typical tumor histology, molecular biological differences, and the malignant potential of tumors at different ages. Pediatric testicular tumors are classified as benign or malignant on the basis of their clinical behavior and histologically are divided into germ cell and gonadal stromal (nongerm cell) tumors. Many histological and biological studies have further confirmed the distinct nature of prepubertal and postpubertal testicular tumors. These differences have led to various management strategies for prepubertal and postpubertal tumors. Because overall about 75% of prepubertal testicular tumors are benign, a testis-sparing approach is becoming more common in children. Orchiectomy and observation with very selective use of chemotherapy has become the standard approach when a malignant tumor is identified. Retroperitoneal lymph node dissection and radiation therapy play very limited roles.
MeSH Terms
Figure
Reference
-
1. Kaplan GW, Cromie WC, Kelalis PP, Silber I, Tank ES Jr. Prepubertal yolk sac testicular tumors: report of the testicular tumor registry. J Urol. 1988; 140(5 Pt 2):1109–1112.2. Kay R. Prepubertal Testicular Tumor Registry. J Urol. 1993; 150(2 Pt 2):671–674.3. Ross JH, Rybicki L, Kay R. Clinical behavior and a contemporary management algorithm for prepubertal testis tumors: a summary of the Prepubertal Testis Tumor Registry. J Urol. 2002; 168(4 Pt 2):1675–1678.4. Metcalfe PD, Farivar-Mohseni H, Farhat W, McLorie G, Khoury A, Bagli DJ. Pediatric testicular tumors: contemporary incidence and efficacy of testicular preserving surgery. J Urol. 2003; 170(6 Pt 1):2412–2415.5. J.S. Valla for the Group D'Etude en Urologie Pédiatrique. Testis-sparing surgery for benign testicular tumors in children. J Urol. 2001; 165(6 Pt 2):2280–2283.6. Baik K, Kang M, Park K, Choi H. Prepubertal testicular tumors in Korea: a single surgeon's experience of more than 20 years. Korean J Urol. 2013; 54:399–403.7. Korean Society of Pediatric Urology. Pediatric Testicular Tumor Registry in Korea: 1997-2001. Korean J Urol. 2004; 45:563–572.8. Chung JM, Lee SD. Korean Society of Pediatric Urology. Pediatric testicular tumor registry in Korea: 2002-2008 (primitive report). Korean J Urol. 2010; 51:Suppl 1. 237.9. Lee SD. Korean Society of Pediatric Urology. Epidemiological and clinical behavior of prepubertal testicular tumors in Korea. J Urol. 2004; 172:674–678.10. Ross JH. Testicular tumors. In : Wilcox D, Godbole P, Cooper C, editors. Pediatric urology book [monograph on the Internet]. [cited 2014 Jul 3]. Available from: http://www.pediatricurologybook.com/tumors.html.11. Walsh TJ, Grady RW, Porter MP, Lin DW, Weiss NS. Incidence of testicular germ cell cancers in U.S. children: SEER program experience 1973 to 2000. Urology. 2006; 68:402–405.12. Pohl HG, Shukla AR, Metcalf PD, Cilento BG, Retik AB, Bagli DJ, et al. Prepubertal testis tumors: actual prevalence rate of histological types. J Urol. 2004; 172(6 Pt 1):2370–2372.13. Ciftci AO, Bingol-Kologlu M, Senocak ME, Tanyel FC, Buyukpamukcu M, Buyukpamukcu N. Testicular tumors in children. J Pediatr Surg. 2001; 36:1796–1801.14. Ritchey ML, Shamberger RC. Pediatric urologic oncology. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 10th ed. Philadelphia: Saunders;2011. p. 3696–3730.15. Ramani P, Yeung CK, Habeebu SS. Testicular intratubular germ cell neoplasia in children and adolescents with intersex. Am J Surg Pathol. 1993; 17:1124–1133.16. Cortes D, Thorup J, Petersen BL. Testicular neoplasia in undescended testes of cryptorchid boys-does surgical strategy have an impact on the risk of invasive testicular neoplasia? Turk J Pediatr. 2004; 46:35–42.17. Pettersson A, Richiardi L, Nordenskjold A, Kaijser M, Akre O. Age at surgery for undescended testis and risk of testicular cancer. N Engl J Med. 2007; 356:1835–1841.18. Green DM. Testicular tumors in infants and children. Semin Surg Oncol. 1986; 2:156–162.19. Harms D, Zahn S, Gobel U, Schneider DT. Pathology and molecular biology of teratomas in childhood and adolescence. Klin Padiatr. 2006; 218:296–302.20. Hawkins E, Heifetz SA, Giller R, Cushing B. The prepubertal testis (prenatal and postnatal): its relationship to intratubular germ cell neoplasia: a combined Pediatric. Hum Pathol. 1997; 28:404–410.21. Rushton HG, Belman AB, Sesterhenn I, Patterson K, Mostofi FK. Testicular sparing surgery for prepubertal teratoma of the testis: a clinical and pathological study. J Urol. 1990; 144:726–730.22. Manivel JC, Reinberg Y, Niehans GA, Fraley EE. Intratubular germ cell neoplasia in testicular teratomas and epidermoid cysts. Correlation with prognosis and possible biologic significance. Cancer. 1989; 64:715–720.23. Renedo DE, Trainer TD. Intratubular germ cell neoplasia (ITGCN) with p53 and PCNA expression and adjacent mature teratoma in an infant testis. An immunohistochemical and morphologic study with a review of the literature. Am J Surg Pathol. 1994; 18:947–952.24. Wu JT, Book L, Sudar K. Serum alpha fetoprotein (AFP) levels in normal infants. Pediatr Res. 1981; 15:50–52.25. Lahdenne P, Kuusela P, Siimes MA, Ronnholm KA, Salmenpera L, Heikinheimo M. Biphasic reduction and concanavalin A binding properties of serum alpha-fetoprotein in preterm and term infants. J Pediatr. 1991; 118:272–276.26. Brewer JA, Tank ES. Yolk sac tumors and alpha-fetoprotein in first year of life. Urology. 1993; 42:79–80.27. Luker GD, Siegel MJ. Pediatric testicular tumors: evaluation with gray-scale and color Doppler US. Radiology. 1994; 191:561–564.28. Pizzocaro G, Zanoni F, Salvioni R, Milani A, Piva L, Pilotti S. Difficulties of a surveillance study omitting retroperitoneal lymphadenectomy in clinical stage I nonseminomatous germ cell tumors of the testis. J Urol. 1987; 138:1393–1396.29. Wiener ES, Lawrence W, Hays D, Lobe TE, Andrassy R, Donaldson S, et al. Retroperitoneal node biopsy in paratesticular rhabdomyosarcoma. J Pediatr Surg. 1994; 29:171–177.30. Stephenson AJ, Gilligan TD. Neoplasms of the testis. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 10th ed. Philadelphia: Saunders;2011. p. 837–870.31. Rescorla FJ. Pediatric germ cell tumors. Semin Pediatr Surg. 2012; 21:51–60.32. Leonard MP, Jeffs RD, Leventhal B, Gearhart JP. Pediatric testicular tumors: the Johns Hopkins experience. Urology. 1991; 37:253–256.33. Carroll WL, Kempson RL, Govan DE, Freiha FS, Shochat SJ, Link MP. Conservative management of testicular endodermal sinus tumor in childhood. J Urol. 1985; 133:1011–1014.34. Weissbach L, Altwein JE, Stiens R. Germinal testicular tumors in childhood. Report of observations and literature review. Eur Urol. 1984; 10:73–85.35. Marshall S, Lyon RP, Scott MP. A conservative approach to testicular tumors in children: 12 cases and their management. J Urol. 1983; 129:350–351.36. Sugita Y, Clarnette TD, Cooke-Yarborough C, Chow CW, Waters K, Hutson JM. Testicular and paratesticular tumours in children: 30 years' experience. Aust N Z J Surg. 1999; 69:505–508.37. Connolly JA, Gearhart JP. Management of yolk sac tumors in children. Urol Clin North Am. 1993; 20:7–14.38. Shukla AR, Woodard C, Carr MC, Huff DS, Canning DA, Zderic SA, et al. Experience with testis sparing surgery for testicular teratoma. J Urol. 2004; 171:161–163.39. Bracken RB, Johnson DE, Cangir A, Ayala A. Regional lymph nodes in infants with embryonal carcinoma of testis. Urology. 1978; 11:376–379.40. Brosman SA. Testicular tumors in prepubertal children. Urology. 1979; 13:581–588.41. Haas RJ, Schmidt P, Gobel U, Harms D. Testicular germ cell tumors, an update. Results of the German cooperative studies 1982-1997. Klin Padiatr. 1999; 211:300–304.42. Mann JR, Pearson D, Barrett A, Raafat F, Barnes JM, Wallendszus KR. Results of the United Kingdom Children's Cancer Study Group's malignant germ cell tumor studies. Cancer. 1989; 63:1657–1667.43. Haas RJ, Schmidt P. Testicular germ-cell tumors in childhood and adolescence. World J Urol. 1995; 13:203–208.44. Rogers PC, Olson TA, Cullen JW, Billmire DF, Marina N, Rescorla F, et al. Treatment of children and adolescents with stage II testicular and stages I and II ovarian malignant germ cell tumors: A Pediatric Intergroup Study--Pediatric Oncology Group 9048 and Children's Cancer Group 8891. J Clin Oncol. 2004; 22:3563–3569.45. Cushing B, Giller R, Cullen JW, Marina NM, Lauer SJ, Olson TA, et al. Randomized comparison of combination chemotherapy with etoposide, bleomycin, and either high-dose or standard-dose cisplatin in children and adolescents with high-risk malignant germ cell tumors: a pediatric intergroup study--Pediatric Oncology Group 9049 and Children's Cancer Group 8882. J Clin Oncol. 2004; 22:2691–2700.46. Ablin AR, Krailo MD, Ramsay NK, Malogolowkin MH, Isaacs H, Raney RB, et al. Results of treatment of malignant germ cell tumors in 93 children: a report from the Childrens Cancer Study Group. J Clin Oncol. 1991; 9:1782–1792.47. Grady RW, Ross JH, Kay R. Epidemiological features of testicular teratoma in a prepubertal population. J Urol. 1997; 158(3 Pt 2):1191–1192.48. Gobel U, Calaminus G, Engert J, Kaatsch P, Gadner H, Bokkerink JP, et al. Teratomas in infancy and childhood. Med Pediatr Oncol. 1998; 31:8–15.49. Altadonna V, Snyder HM 3rd, Rosenberg HK, Duckett JW. Simple cysts of the testis in children: preoperative diagnosis by ultrasound and excision with testicular preservation. J Urol. 1988; 140:1505–1507.50. Elert A, Olbert P, Hegele A, Barth P, Hofmann R, Heidenreich A. Accuracy of frozen section examination of testicular tumors of uncertain origin. Eur Urol. 2002; 41:290–293.51. De Backer A, Madern GC, Pieters R, Haentjens P, Hakvoort-Cammel FG, Oosterhuis JW, et al. Influence of tumor site and histology on long-term survival in 193 children with extracranial germ cell tumors. Eur J Pediatr Surg. 2008; 18:1–6.52. Hasegawa T, Maeda K, Kamata N, Okita Y. A case of immature teratoma originating in intra-abdominal undescended testis in a 3-month-old infant. Pediatr Surg Int. 2006; 22:570–572.53. Ross JH, Kay R, Elder J. Testis sparing surgery for pediatric epidermoid cysts of the testis. J Urol. 1993; 149:353–356.54. Wilson BE, Netzloff ML. Primary testicular abnormalities causing precocious puberty Leydig cell tumor, Leydig cell hyperplasia, and adrenal rest tumor. Ann Clin Lab Sci. 1983; 13:315–320.55. Thomas JC, Ross JH, Kay R. Stromal testis tumors in children: a report from the prepubertal testis tumor registry. J Urol. 2001; 166:2338–2340.56. Petkovic V, Salemi S, Vassella E, Karamitopoulou-Diamantis E, Meinhardt UJ, Fluck CE, et al. Leydig-cell tumour in children: variable clinical presentation, diagnostic features, follow-up and genetic analysis of four cases. Horm Res. 2007; 67:89–95.57. Shukla AR, Huff DS, Canning DA, Filmer RB, Snyder HM 3rd, Carpintieri D, et al. Juvenile granulosa cell tumor of the testis: contemporary clinical management and pathological diagnosis. J Urol. 2004; 171:1900–1902.58. Young RH, Koelliker DD, Scully RE. Sertoli cell tumors of the testis, not otherwise specified: a clinicopathologic analysis of 60 cases. Am J Surg Pathol. 1998; 22:709–721.59. Urban MD, Lee PA, Plotnick LP, Migeon CJ. The diagnosis of Leydig cell tumors in childhood. Am J Dis Child. 1978; 132:494–497.60. Konrad D, Schoenle EJ. Ten-year follow-up in a boy with Leydig cell tumor after selective surgery. Horm Res. 1999; 51:96–100.61. Henderson CG, Ahmed AA, Sesterhenn I, Belman AB, Rushton HG. Enucleation for prepubertal leydig cell tumor. J Urol. 2006; 176:703–705.62. Wegner HE, Dieckmann KP, Herbst H, Andresen R, Miller K. Leydig cell tumor: comparison of results of radical and testis-sparing surgery in a single center. Urol Int. 1997; 59:170–173.63. Cortez JC, Kaplan GW. Gonadal stromal tumors, gonadoblastomas, epidermoid cysts, and secondary tumors of the testis in children. Urol Clin North Am. 1993; 20:15–26.64. Young RH, Lawrence WD, Scully RE. Juvenile granulosa cell tumor--another neoplasm associated with abnormal chromosomes and ambiguous genitalia. A report of three cases. Am J Surg Pathol. 1985; 9:737–743.65. Dudani R, Giordano L, Sultania P, Jha K, Florens A, Joseph T. Juvenile granulosa cell tumor of testis: case report and review of literature. Am J Perinatol. 2008; 25:229–231.66. Gabrilove JL, Freiberg EK, Leiter E, Nicolis GL. Feminizing and non-feminizing Sertoli cell tumors. J Urol. 1980; 124:757–767.67. Goswitz JJ, Pettinato G, Manivel JC. Testicular sex cord-stromal tumors in children: clinicopathologic study of sixteen children with review of the literature. Pediatr Pathol Lab Med. 1996; 16:451–470.68. Kolon TF, Hochman HI. Malignant Sertoli cell tumor in a prepubescent boy. J Urol. 1997; 158:608–609.69. Nonomura K, Koyama T, Kakizaki H, Murakumo M, Shinohara N, Koyanagi T. Testicular-sparing surgery for the prepubertal testicular tumor. Experience of two cases with large cell calcifying Sertoli cell tumors. Eur Urol. 2001; 40:699–704.70. Rosvoll RV, Woodard JR. Malignant Sertoli cell tumor of the testis. Cancer. 1968; 22:8–13.71. Manuel M, Katayama PK, Jones HW Jr. The age of occurrence of gonadal tumors in intersex patients with a Y chromosome. Am J Obstet Gynecol. 1976; 124:293–300.72. Schellhas HF. Malignant potential of the dysgenetic gonad. Part 1. Obstet Gynecol. 1974; 44:298–309.73. Olsen MM, Caldamone AA, Jackson CL, Zinn A. Gonadoblastoma in infancy: indications for early gonadectomy in 46XY gonadal dysgenesis. J Pediatr Surg. 1988; 23:270–271.74. Gourlay WA, Johnson HW, Pantzar JT, McGillivray B, Crawford R, Nielsen WR. Gonadal tumors in disorders of sexual differentiation. Urology. 1994; 43:537–540.75. Cools M, Drop SL, Wolffenbuttel KP, Oosterhuis JW, Looijenga LH. Germ cell tumors in the intersex gonad: old paths, new directions, moving frontiers. Endocr Rev. 2006; 27:468–484.76. Askin FB, Land VJ, Sullivan MP, Ragab AH, Steuber CP, Dyment PG, et al. Occult testicular leukemia: testicular biopsy at three years continuous complete remission of childhood leukemia: a Southwest Oncology Group Study. Cancer. 1981; 47:470–475.77. Finn LS, Viswanatha DS, Belasco JB, Snyder H, Huebner D, Sorbara L, et al. Primary follicular lymphoma of the testis in childhood. Cancer. 1999; 85:1626–1635.78. Lamm DL, Kaplan GW. Urological manifestations of Burkitt's lymphoma. J Urol. 1974; 112:402–405.79. Noh PH, Cooper CS, Snyder HM 3rd. Conservative management of cystic dysplasia of the testis. J Urol. 1999; 162:2145.80. Toffolutti T, Gamba PG, Cecchetto G, Talenti E, Tchaprassian Z. Testicular cystic dysplasia: evaluation of 3 new cases treated without surgery. J Urol. 1999; 162:2146–2148.81. Eberli D, Gretener H, Dommann-Scherrer C, Pestalozzi D, Fehr JL. Cystic dysplasia of the testis: a very rare paediatric tumor of the testis. Urol Int. 2002; 69:1–6.82. Furness PD 3rd, Husmann DA, Brock JW 3rd, Steinhardt GF, Bukowski TP, Freedman AL, et al. Multi-institutional study of testicular microlithiasis in childhood: a benign or premalignant condition? J Urol. 1998; 160(3 Pt 2):1151–1154.83. Dell'Acqua A, Toma P, Oddone M, Ciccone MA, Marsili E, Derchi LE. Testicular microlithiasis: US findings in six pediatric cases and literature review. Eur Radiol. 1999; 9:940–944.84. Leenen AS, Riebel TW. Testicular microlithiasis in children: sonographic features and clinical implications. Pediatr Radiol. 2002; 32:575–579.