J Korean Soc Radiol.
2014 Nov;71(5):201-204. 10.3348/jksr.2014.71.5.201.
Osmotic Demyelination Syndrome with Recent Chemotherapy in Normonatremic Patient: A Case Report
- Affiliations
-
- 1Department of Radiology, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. sartre81@gmail.com
- KMID: 2208789
- DOI: http://doi.org/10.3348/jksr.2014.71.5.201
Abstract
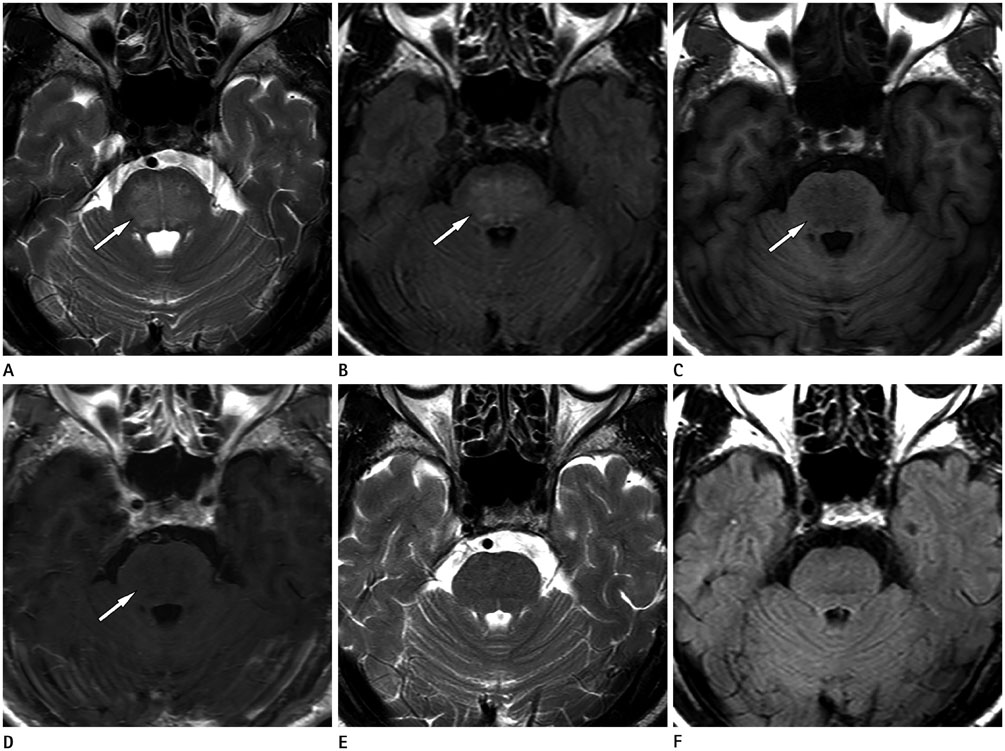
- Osmotic demyelination syndrome (ODS), an acquired demyelinating condition of the central pons and/or other regions of the brain, is frequently associated with rapid correction of hyponatremia. There are several reports of ODS in other clinical setting such as malnutrition, alcoholism, transplantation, malignancy, and chronic debilitating illness. However, cases of ODS associated with chemotherapy have not been frequently reported. Here, we describe a case of ODS in a normonatremic patient recently underwent chemotherapy for colon cancer. The diagnosis was confirmed by MRI showing a typical T2 hyperintensity in the central pons. This case suggests that ODS is not always associated with hyponatremia and that ODS can have a favorable clinical and radiologic prognosis.
MeSH Terms
Figure
Reference
-
1. Adams RD, Victor M, Mancall EL. Central pontine myelinolysis: a hitherto undescribed disease occurring in alcoholic and malnourished patients. AMA Arch Neurol Psychiatry. 1959; 81:154–172.2. Martin RJ. Central pontine and extrapontine myelinolysis: the osmotic demyelination syndromes. J Neurol Neurosurg Psychiatry. 2004; 75:Suppl 3. iii22–iii28.3. Dolciotti C, Nuti A, Cipriani G, Borelli P, Baldacci F, Logi C, et al. Cerebellar ataxia with complete clinical recovery and resolution of MRI lesions related to central pontine myelinolysis: case report and literature review. Case Rep Neurol. 2010; 2:157–162.4. King JD, Rosner MH. Osmotic demyelination syndrome. Am J Med Sci. 2010; 339:561–567.5. Huq S, Wong M, Chan H, Crimmins D. Osmotic demyelination syndromes: central and extrapontine myelinolysis. J Clin Neurosci. 2007; 14:684–688.6. Lupato A, Fazio P, Fainardi E, Cesnik E, Casetta I, Granieri E. A case of asymptomatic pontine myelinolysis. Neurol Sci. 2010; 31:361–364.7. Cramer SC, Stegbauer KC, Schneider A, Mukai J, Maravilla KR. Decreased diffusion in central pontine myelinolysis. AJNR Am J Neuroradiol. 2001; 22:1476–1479.8. Hurley RA, Filley CM, Taber KH. Central pontine myelinolysis: a metabolic disorder of myelin. J Neuropsychiatry Clin Neurosci. 2011; 23:369–374.9. Yau TK, Yiu HY, Lee WM. Central pontine myelinolysis: report of two occurrences after cisplatin-containing chemotherapy for nasopharyngeal carcinoma. Clin Oncol (R Coll Radiol). 1993; 5:395–339.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cortical Laminar Necrosis associated with Osmotic Demyelination Syndrome
- Osmotic Demyelination Syndrome Resulting from an Unexpected Response to Tolvaptan in a Patient with Heart Failure
- Initial Transient Neurologic Recovery Followed by Delayed Deterioration of Osmotic Demyelination Syndrome: A Case Report
- Serial Magnetic Resonance Imaging Findings in Hyperglycemia-Related Osmotic Demyelination Syndrome: A Case Report
- A Case of Osmotic Demyelination Syndrome after Hemodialysis Treatment in a Uremic Patient with Severe Hyperosmolality