J Korean Soc Clin Pharmacol Ther.
2013 Dec;21(2):166-173. 10.12793/jkscpt.2013.21.2.166.
Validation of LC-MS/MS Method for Determination of Bivalirudin in Human Plasma: Application to a Pharmacokinetic Study
- Affiliations
-
- 1Department of Clinical Pharmacology and Therapeutics, Asan Medical Center, Seoul, Korea. ksbae@amc.seoul.kr
- 2Department of Clinical Pharmacology and Therapeutics, University of Ulsan College of Medicine, Korea.
- 3Clinical Trial Center, Asan Medical Center, Seoul, Korea.
- KMID: 2203230
- DOI: http://doi.org/10.12793/jkscpt.2013.21.2.166
Abstract
- BACKGROUND
Bivalirudin is a direct thrombin inhibitor for patients with unstable angina undergoing percutaneous coronary intervention.
METHODS
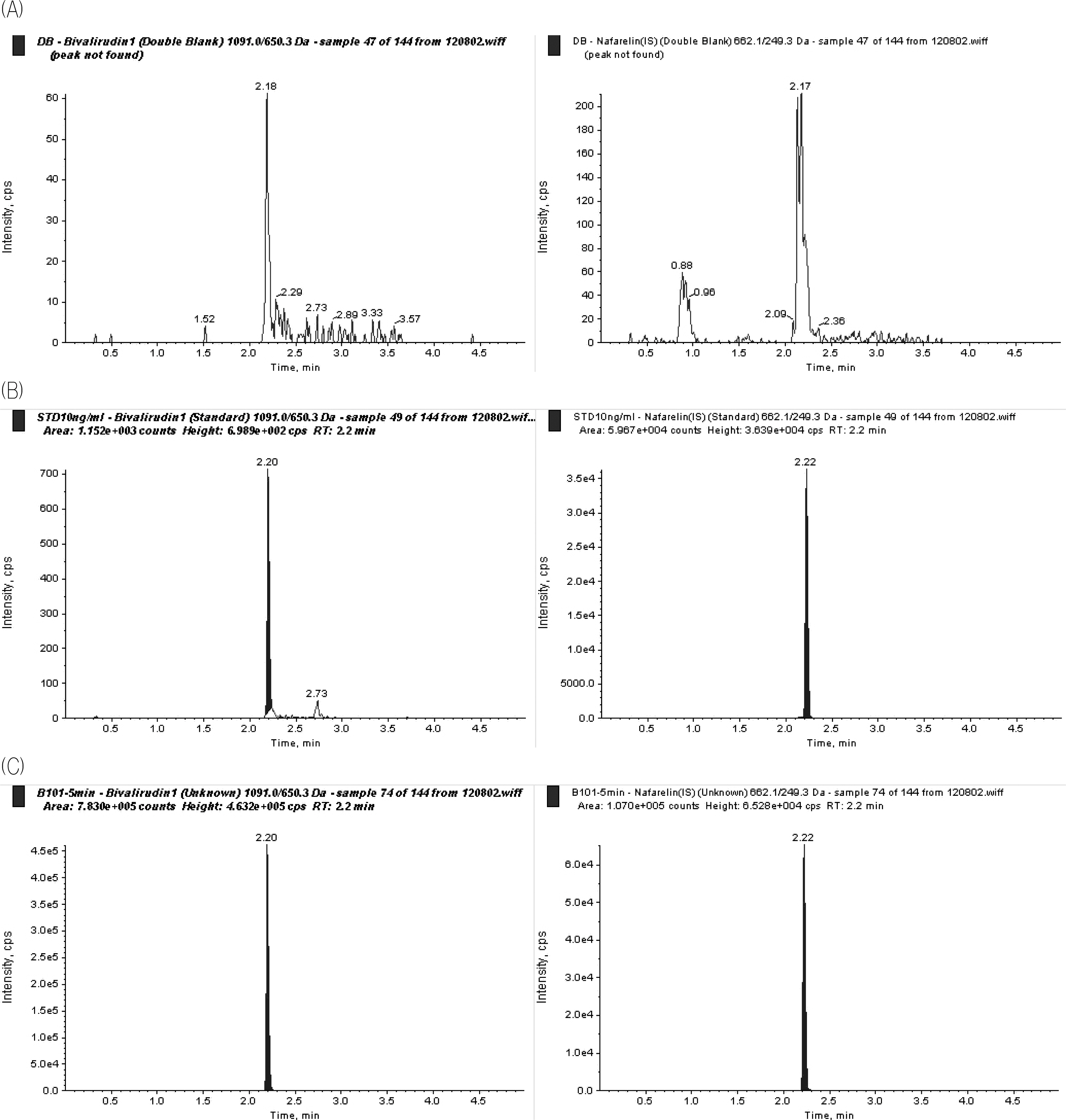
A sensitive liquid chromatography-tandem mass spectrometry (LC/MS/MS) method was developed and validated for the determination of bivalirudin, in human plasma using nafarelin as internal standard (IS). Chromatographic separation was performed using a Shiseido MG3 mm column (2.0 x 50 mm) with a gradient mobile phase consisting of water and acetonitrile containing 0.1 % formic acid at a flow rate of 0.4 mL/min, and total run time was within 5 min. Detection and quantification was performed by the mass spectrometer using a multiple reaction-monitoring mode at m/z 1091.0 --> 650.3 for bivalirudin, and m/z 662.1 --> 249.3 for IS.
RESULTS
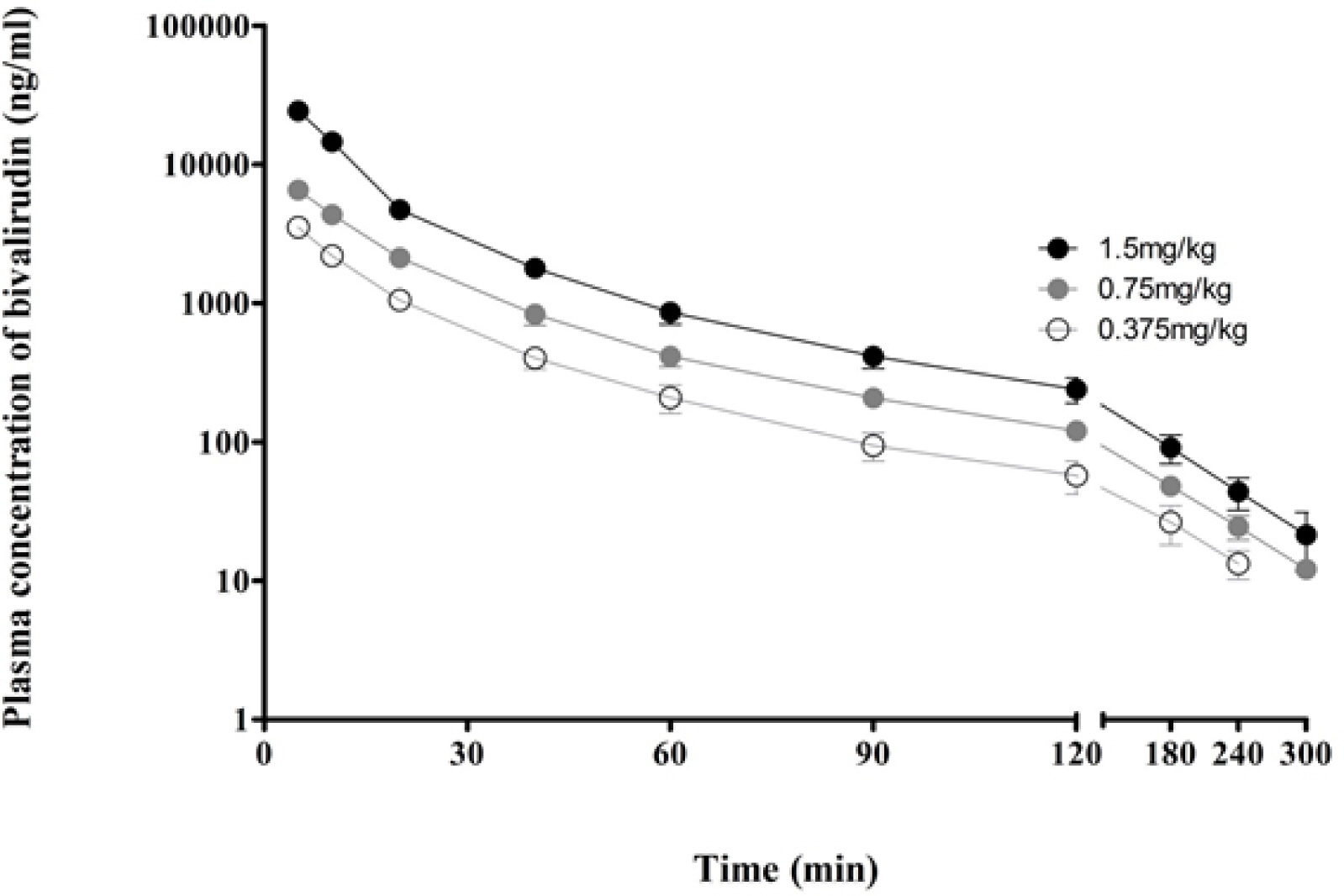
The assay was linear over a concentration range of 10 - 10000 ng/mL with a lower limit of quantification of 10 ng/mL in human plasma.
CONCLUSION
This method was successfully applied for pharmacokinetics study after intravenous administration of bivalirudin to healthy Korean male volunteers.
Keyword
MeSH Terms
Figure
Reference
-
1. Gladwell TD. Bivalirudin: a direct thrombin inhibitor. Clin Ther. 2002; 24(1):38–58.
Article2. Lincoff AM, Bittl JA, Harrington RA, Feit F, Kleiman NS, Jackman JD, Sarembock IJ, Cohen DJ, Spriggs D, Ebrahimi R, Keren G, Carr J, Cohen EA, Betriu A, Desmet W, Kereiakes DJ, Rutsch W, Wilcox RG, de Feyter PJ, Vahanian A, Topol EJ, Investigators R. Bivalirudin and provisional glycoprotein IIb/IIIa blockade compared with heparin and planned glycoprotein IIb/IIIa blockade during percutaneous coronary intervention: REPLACE-2 randomized trial. JAMA. 2003; 289(7):853–863.3. EMEA. Scientific discussion for the approval of Bivalirudin [cited 2013 31 Oct]. Available from. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Scientific_Discussion/human/000562/WC500025072.pdf.4. FDA. NDA 020873 Angiomax (Bivalirudin): Clinical Pharmacology Biopharmaceutics Review. Rockville, MD: Department of Health and Human Services, US Food and Drug Administration;2003.5. Robson R, White H, Aylward P, Frampton C. Bivalirudin pharmacokinetics and pharmacodynamics: effect of renal function, dose, and gender. Clin Pharmacol Ther. 2002; 71(6):433–439.
Article6. Lidon RM, Theroux P, Juneau M, Adelman B, Maraganore J. Initial experience with a direct antithrombin, Hirulog, in unstable angina. Anticoagulant, antithrombotic, and clinical effects. Circulation. 1993; 88(4 Pt 1):1495–1501.
Article7. Topol EJ, Bonan R, Jewitt D, Sigwart U, Kakkar VV, Rothman M, de Bono D, Ferguson J, Willerson JT, Strony J, et al. Use of a direct antithrombin, hirulog, in place of heparin during coronary angioplasty. Circulation. 1993; 87(5):1622–1629.
Article8. Reed MD, Bell D. Clinical pharmacology of bivalirudin. Pharmacotherapy. 2002; 22(6 Pt 2): 105S–111S.
Article9. Anand SX, Viles-Gonzalez JF, Mahboobi SK, Heerdt PM. Bivalirudin utilization in cardiac surgery: shifting anticoagulation from indirect to direct thrombin inhibition. Can J Anaesth. 2011; 58(3):296–311.
Article10. Shammas NW. Bivalirudin: pharmacology and clinical applications. Cardiovasc Drug Rev. 2005; 23(4):345–360.
Article11. Pan G, Wang X, Huang Y, Gao X, Wang Y. Development and validation of a LC-MS/MS method for determination of bivalirudin in human plasma: Application to a clinical pharmacokinetic study. J Pharm Biomed Anal. 2010; 52(1):105–109.
Article12. Farthing D, Larus T, Fakhry I, Gehr T, Prats J, Sica D. Liquid chromatography method for determination of bivalirudin in human plasma and urine using automated ortho-phthalaldehyde derivatization and fluorescence detection. J Chromatogr B Analyt Technol Biomed Life Sci. 2004; 802(2):355–359.
Article13. Maraganore JM, Bourdon P, Jablonski J, Ramachandran KL, Fenton JW 2nd. Design and characterization of hirulogs: a novel class of bivalent peptide inhibitors of thrombin. Biochemistry. 1990; 29(30):7095–7101.
Article14. Zhang X, Nieforth K, Lang JM, Rouzier-Panis R, Reynes J, Dorr A, Kolis S, Stiles MR, Kinchelow T, Patel IH. Pharmacokinetics of plasma enfuvirtide after subcutaneous administration to patients with human immunodeficiency virus: Inverse Gaussian density absorption and 2-compartment disposition. Clin Pharmacol Ther. 2002; 72(1):10–19.15. Douglas SA. Human urotensin-II as a novel cardiovascular target: ‘heart’ of the matter or simply a fishy ‘tail’? Curr Opin Pharmacol. 2003; 3(2):159–167.
Article16. John H, Walden M, Schafer S, Genz S, Forssmann WG. Analytical procedures for quantification of peptides in pharmaceutical research by liquid chromatography-mass spectrometry. Anal Bioanal Chem. 2004; 378(4):883–897.
Article17. FDA. Bioanalytical Method Validation (Draft Guidance). Rockville, MD: Department of Health and Human Services, US Food and Drug Administration;2013.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development and validation of a UPLC-MS/MS method for the quantification of acetaminophen in human plasma and its application to pharmacokinetic studies
- Development and validation of analytical method for the determination of radotinib in human plasma using liquid chromatography-tandem mass spectrometry
- Qualification and application of liquid chromatography-quadrupole time-offlight mass spectrometric method for the determination of carisbamate in rat plasma and prediction of its human pharmacokinetics using physiologically based pharmacokinetic modeling
- Determination of sumatriptan in human plasma using liquid chromatography-mass spectrometry for pharmacokinetic study in healthy Korean volunteers
- Performance Evaluation of MassTrak LC/MS/MS Tacrolimus Kit