J Korean Soc Endocrinol.
2005 Oct;20(5):467-475. 10.3803/jkes.2005.20.5.467.
Therapeutic Effects of Metformin and Rosiglitazone in Korean Women with Polycystic Ovary Syndrome
- Affiliations
-
- 1Department of Internal Medicine, Ewha Womans University College of Medicine, Korea.
- 2Department of Obstetrics and Gynecology, Ewha Womans University College of Medicine, Korea.
- KMID: 2200594
- DOI: http://doi.org/10.3803/jkes.2005.20.5.467
Abstract
-
BACKGROUND: Insulin resistance is a central feature of polycystic ovary syndrome (PCOS), and hyperinsulinemia contributes to anovulation, oligo or amenorrhea, hyperandrogenism and infertility in women with PCOS. The use of insulin sensitizers, such as metformin or thiazolidinedione, in PCOS is becoming increasingly accepted. The purpose of our study was to evaluate the therapeutic effects of metformin and rosiglitazone on the metabolic and reproductive derangement, and find parameters predicting their therapeutic efficacy in Korean PCOS women.
METHODS
Sixty-two women with PCOS were recruited. The baseline characteristics, including BMI, glucose tolerance test, lipid profiles, sex hormones and hyperinsulinemic euglycemic clamp test, were assessed. After the administration of the insulin sensitizer (metformin 1.5g/day or rosiglitazone 4mg/day) for 3 months, the insulin sensitivity was reassessed. A drug response was defined as menstrual restoration or pregnancy.
RESULTS
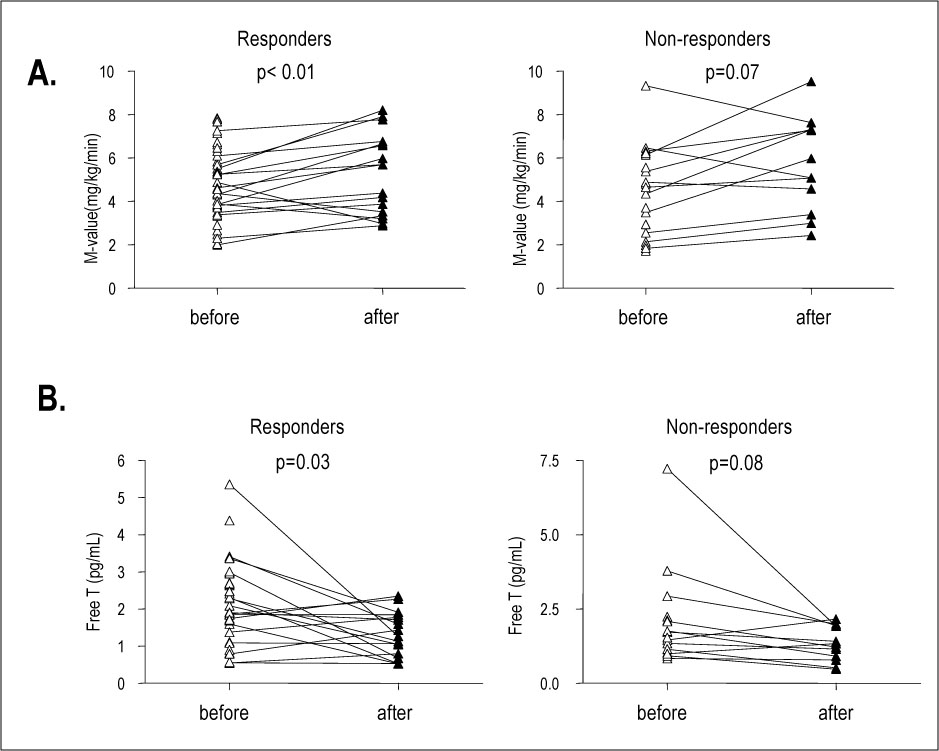
Of the 62 women with PCOS, 36 gained restored regular menstruation, and a further 5 conceived (a drug response rate of 66.7%). There were no significant clinical differences between responders and nonresponders. Twelve weeks after taking the drugs, the insulin sensitivity was significantly improved (M-value 4.7+/-0.2 vs. 5.5+/-0.4mg/kg/min, P<0.05), and the free testosterone levels(72.5+/-39.9 vs. 45.8 +/-3.8pmol/L, P<0.05) were significantly decreased, without significant weight reduction.
CONCLUSION
Metformin and rosiglitazone restored menstruation in 66.1% of women with PCOS. Hyperandrogenemia and insulin sensitivity were significantly improved with the use of the two drugs. However, metabolic or hormonal markers for predicting the drug response could not be found.
MeSH Terms
-
Amenorrhea
Anovulation
Female
Glucose Clamp Technique
Glucose Tolerance Test
Gonadal Steroid Hormones
Humans
Hyperandrogenism
Hyperinsulinism
Infertility
Insulin
Insulin Resistance
Menstruation
Metformin*
Polycystic Ovary Syndrome*
Pregnancy
Testosterone
Weight Loss
Gonadal Steroid Hormones
Insulin
Metformin
Testosterone
Figure
Reference
-
1. Knochenhauser ES, Key TJ, Kahsar-Miller M, waggoner W, Boots LR, Azziz R. Prevalence of the polycystic ovary syndrome in unselected black and white women of the southeastern United States: a prospective study. J Clin Endocrinol Metab. 1998. 83:3078–3082.2. Nestler JE. Role of hyperinsulinemia in the pathogenesis of the polycystic ovary syndrome, and its clinical implications. Sem Reprod Endocrinol. 1997. 15:111–122.3. Reaven GM. Role of insulin resistance in human disease. Diabetes. 1988. 37:1595–1607.4. Dunaif A. Insulin action in the polycystic ovary syndrome. Endocrinol Metab Clin North Am. 1999. 28:341–359.5. Dunaif A, Futterweit W, Segal KR. Profound peripheral insulin resistance, independent of obesity, in the polycystic ovary syndrome. Diabetes. 1989. 38:1165–1174.8. Gambineri A. Obesity and the PCO syndrome. Int J Obest Metab Dis. 2002. 26:883–896.9. Iuorno J, Nestler E. Insulin lowering drugs in polycystic ovary syndrome. Obstet Gynecol Clinic. 2001. 28:153–164.10. Velazquez EM, Mendoza S, Hamer T, Sosa F, Glueck CJ. Metformin therapy in polycystic ovary syndrome reduces hyperinsulinemia, insulin resistance, hyperandrogenemia, and systolic blood pressure, while facilitating normal menses and pregnancy. Metabolism. 1994. 43:647–654.11. Morin-Papunen LC, Koivunen RM, Ruokonen A, Martikainen HK. Metformin therapy improves the menstrual pattern with minimal endocrine and metabolic effects in women with polycystic ovary syndrome. Fertil Steril. 1998. 69:691–696.12. Nestler JE, Jakubowicz DJ, Evans WS, Pasquali R. Effects of metformin on spontaneous and clomiphene-induced ovulation in the polycystic ovary syndrome. N Engl J Med. 1998. 338:1876–1880.13. Glueck CJ, Wang P, Fontaine R, Tracy T, Sieve-Smith L. Metformin-induced resumption of normal menses in 39 of 43 (91%) previously amenorrheic women with the polycystic ovary syndrome. Metabolism. 1999. 48:511–519.14. Ibanez L, Valls C, Potau N, Marcos MV, de Zegher F. Sensitization to insulin in adolescent girls to normalize hirsutism, hyperandrogenism, oligomenorrhea, dyslipidemia, and hyperinsulinism after precocious pubarche. J Clin Endocrinol Metab. 2000. 85:3526–3530.15. Dunaif A, Scott D, Finegood D, Quintana B, Whitcomb R. The insulin-sensitizing agent troglitazone improves metabolic and reproductive abnormalities in the polycystic ovary syndrome The insulin-sensitizing agent troglitazone improves metabolic and reproductive abnormalities in the polycystic ovary syndrome. J Clin Endocrinol Metab. 1996. 81:3299–3306.16. Cataldo NA, Abbasi F, McLaughlin TL, Lamendola C, Reaven GM. Improvement in insulin sensitivity followed by ovulation and pregnancy in a woman with polycystic ovary syndrome who was treated with rosiglitazone. Fertil Steril. 2001. 76:1057–1059.17. The Rotterdam ESHRE/ASRM-sponsored PCOS consensus workshop group. Revised 2003 consensus on diagnostic criteria and long health risks related to polycystic ovary syndrome. Hum Reprod. 2004. 19:41–47.19. World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its complication: Report of a WHO consultation. Diagnosis and classification of diabetes mellitus. 1999. Geneva: World Health Organization.20. DeFronzo RA, Tobin JD, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979. 237:E214–E223.21. Tsai EC, Matsumoto AM, Fujimoto WY, Boyko EJ. Association of bioavailable, free, and total testosterone with insulin resistance: influence of sex hormone-binding globulin and body fat. Diabetes Care. 2004. 27:861–868.22. Jayagopal V, Kilpatrick ES, Jennings PE, Hepburn DA, Atkin SL. The biological variation of testosterone and sex hormone-binding globulin (SHBG) in polycystic ovarian syndrome: implications for SHBG as a surrogate marker of insulin resistance. J Clin Endocrinol Metab. 2003. 88:1528–1533.23. Rajkhowa M, Bicknell J, Jones M, Clayton RN. Insulin sensitivity in women with polycystic ovary syndrome: relationship to hyperandrogenemia. Fertil Steril. 1994. 61:605–612.24. Kriplani A, Agarwal N. Effects of metformin on clinical and biochemical parameters in polycystic ovary syndrome. J Reproduc Med. 2004. 49:361–367.25. Ghazeeri G, Kutteh WH, Bryer-Ash M, Haas D, Ke RW. Effect of rosiglitazone on spontaneous and clomiphen citrate-induced ovulation in women with polycystic ovary syndrome. Fertil Steril. 2003. 79:562–566.26. Belli SH, Graffigna MN, Oneto A, Otero P, Schurman L, Levalle OA. Effect of rosiglitazone on insulin resistance, growth factors, and reproductive disturbances in women with polycystic ovary syndrome. Fertil Steril. 2004. 81:624–629.27. Mehnert H. Metformin, the rebirth of a biguanide: mechanism of action and place in the prevention and treatment of insulin resistance. Exp Clin Endocrinol Diabetes. 2001. 109:S259–S264.28. Witters LA. The blooming of the French lilac. J CLin Invest. 2001. 108:1105–1107.29. Zhou G, Myers R, Li Y, Chen Y, Shen X, Fenyk-Melody J, Wu M, Ventre J, Doebber T, Fujii N, Musi N, Hirshman MF, Goodyear LJ, Moller DE. Role of AMP-activated protein kinase in mechanism of metformin action. J Clin Invest. 2001. 108:1167–1174.30. Attia GR, Rainey WE, Carr BR. Metformin directly inhibits androgen production in human theca cells. Fertil Steril. 2001. 76:517–524.31. Arlt W, Auchus RJ, Miller WL. Thiazolidinediones but not metformin directly inhibit the steroidogenic enzymes P450c17 and 3beta-hydroxysteroid dehydrogenase. J Biol Chem. 2001. 276:16767–16771.32. Azziz R, Ehrmann DA, Legro RS, Fereshetian AG, O'Keefe M, Ghazzi MN. PCOS/Troglitazone study Group Troglitazone decreases adrenal androgen levels in women with polycystic ovary syndrome. Fertil Steril. 2003. 79:927–937.33. Zheng Z, Li M, Lin Y, Ma Y. Effect of rosiglitazone on insulin resistance and hyperandrogenism in polyc ystic ovary syndrome. Zhonghua Fu Chan Ke Za Zhi. 2002. 37:271–273.34. Baillargeon JP, Kahubowicz DJ, Iuorno MJ, Jakubowicz S, Nestler JE. Effects of metformin and rosiglitazone, alone and in combination, in nonobese women with polycystic ovary syndrome and normal indices of insulin sensitivity. Fertil Steril. 2004. 82:893–902.35. Brettenthaler N, De Geyter C, Huber PR, Keller U. Effect of the insulin sensitizer pioglitazone on insulin resistance, hyperandrogenism, and ovulatory dysfuction in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2004. 89:3835–3840.36. Glueck CJ, Moreira A, Goldenberg N, Sieve L, Wang P. Pioglitazone and metformin in obese women with polycystic ovary syndrome not optimally responsive to metformin. Hum Reprod. 2003. 18:1618–1625.37. Guido M, Romualdi D, Suriano R, Giuliani M, Costantini B, Apa R, Lanzone A. Effect of pioglitazone treatment on the adrenal androgen response to corticotrophin in obese patients with polycystic ovary syndrome. Hum Reprod. 2004. 19:534–539.38. Vandermolen DT, Ratts VS, Evans WS, Stovall DW, Kauma SW, Nestler JE. Metformin increases the ovulatory rate and pregnancy rate from clomiphen cirate in patients with polycystic ovary syndrome who are resistant to clomiphene citrate alone. Fertil Steril. 2001. 75:310–315.39. De Leo V, la Marca A, Ditto A, Morgante G, Cianci A. Effects of metformin on gonadotropin-induced ovulation in women with polycystic ovary syndrome. Steril Fertil. 1999. 72:282–285.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Metformin and Rosiglitazone in Overweight or Obese Women with Polycystic Ovarian Syndrome
- Recent Treatment Strategies for Polycystic Ovary Syndrome
- Studies on Fibrinolytic System Behavior in Women with Polycystic Ovary Syndrome
- The Effect of Metformin in Non-Obese Women with Polycystic Ovary Syndrome; Pilot Stud
- Medical diagnosis and treatment of polycystic ovary syndrome