J Lipid Atheroscler.
2012 Jun;1(1):35-39. 10.12997/jla.2012.1.1.35.
Sudden Cardiac Arrest in a Low-Risk Patient During Elective Spinal Surgery
- Affiliations
-
- 1Korea Cardiovascular Stent Research Institute of Chonnam National University, Gwangju, Korea. myungho@chollian.net
- KMID: 2198374
- DOI: http://doi.org/10.12997/jla.2012.1.1.35
Abstract
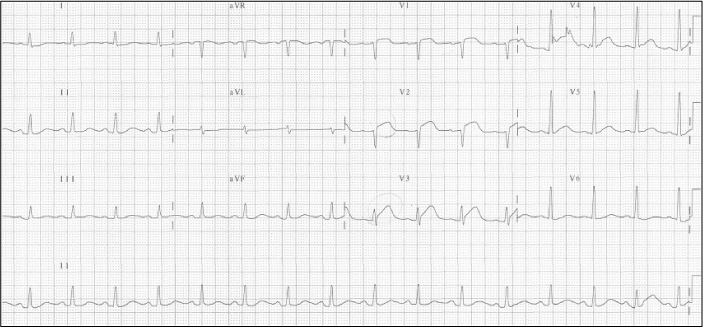
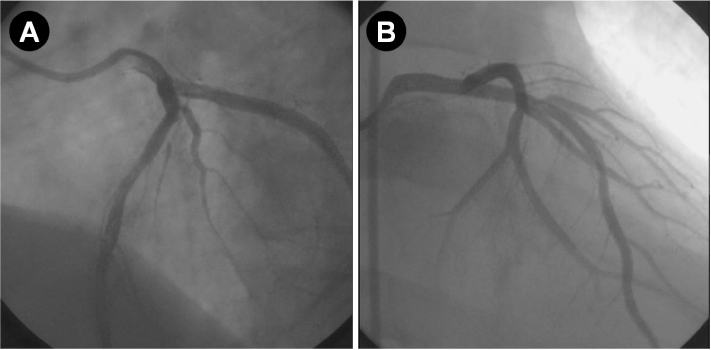
- Patients with intermittent claudication secondary to spinal problem may have asymptomatic cardiac disease. We experienced a case of sudden cardiac arrest in a low-risk male patient during elective spinal surgery which was performed in accordance with the current guidelines. A 54-year-old male, who did not have active cardiac conditions or clinical risk factors for perioperative cardiovascular events, was scheduled to have a planned surgery for spinal stenosis without preoperative testing for cardiovascular events according to the current guidelines. But, he developed sudden cardiac arrest during elective spinal surgery. Emergent coronary angiogram showed significant stenosis in the distal left main coronary artery and proximal left anterior descending coronary artery. We successfully deployed 2 bare metal stents with intravascular ultrasound guidance. His mental state recovered and he was extubated 4 hours later. On day 8 in the hospital, he was transferred to the local hospital for care of his spinal problem.
MeSH Terms
Figure
Reference
-
1. Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WR, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet. 2008; 372:139–144.
Article2. Gunzburg R, Szpalski M. The conservative surgical treatment of lumbar spinal stenosis in the elderly. Eur Spine J. 2003; 12:Suppl 2. S176–S180.
Article3. Faciszewski T, Jensen R, Rokey R, Berg R. Cardiac risk stratification of patients with symptomatic spinal stenosis. Clin Orthop Relat Res. 2001; 110–115.
Article4. Shin DG. Current Perspectives on Methods for Predicting Risk of Sudden Cardiac Death. Korean Circ J. 2002; 32:637–645.
Article5. Devereaux PJ, Yang H, Yusuf S, Guyatt G, Leslie K, Villar JC, et al. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008; 371:1839–1847.
Article6. Fleischmann KE, Goldman L, Young B, Lee TH. Association between cardiac and noncardiac complications in patients undergoing noncardiac surgery: outcomes and effects on length of stay. Am J Med. 2003; 115:515–520.
Article7. Landesberg G, Shatz V, Akopnik I, Wolf YG, Mayer M, Berlatzky Y, et al. Association of cardiac troponin, CK-MB, and postoperative myocardial ischemia with long-term survival after major vascular surgery. J Am Coll Cardiol. 2003; 42:1547–1554.
Article8. Fleisher LA, Beckman JA, Brown KA, Calkins H, Chaikof EL, Fleischmann KE, et al. 2009 ACCF/AHA focused update on perioperative beta blockade incorporated into the ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American college of cardiology foundation/American heart association task force on practice guidelines. Circulation. 2009; 120:e169–e276.9. Goldman L, Caldera DL, Nussbaum SR, Southwick FS, Krogstad D, Murray B, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med. 1977; 297:845–850.
Article10. Detsky AS, Abrams HB, Forbath N, Scott JG, Hilliard JR. Cardiac assessment for patients undergoing noncardiac surgery. A multifactorial clinical risk index. Arch Intern Med. 1986; 146:2131–2134.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Sudden Cardiac Arrest during Spinal Anesthesia
- Medullary Infarction Presenting as Sudden Cardiac Arrest: Report of Two Cases and Review of the Literature
- Sudden Cardiac Arrest Postoperative Day due to Pulmonary Embolism
- Vasovagal cardiac arrest during spinal anesthesia for Cesarean section: A case report
- Cardiac Arrest during Tracheostomy Cannula Misplacement - A Case of Diphtheria