J Korean Neurotraumatol Soc.
2010 Jun;6(1):6-12. 10.13004/jknts.2010.6.1.6.
The Usefulness of CT Brain Perfusion Image on Evaluation of Traumatic Brain Injury
- Affiliations
-
- 1Department of Neurosurgery, Wonju College of Medicine, Yonsei University, Wonju, Korea. whangkum@yonsei.ac.kr
- 2Department of Radiology, Wonju College of Medicine, Yonsei University, Wonju, Korea.
- KMID: 2192353
- DOI: http://doi.org/10.13004/jknts.2010.6.1.6
Abstract
OBJECTIVE
The purpose of this study is to evaluate the finding of computed tomography brain perfusion (CBP) in early traumatic brain injury patient.
METHODS
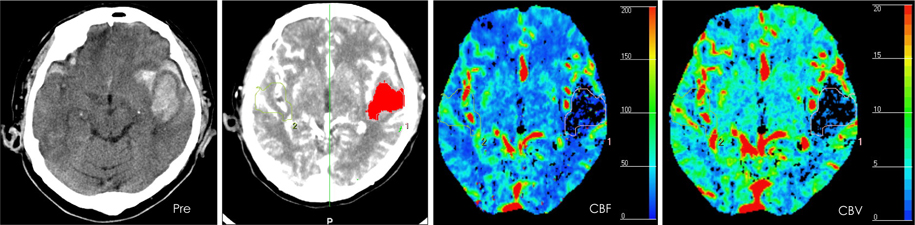
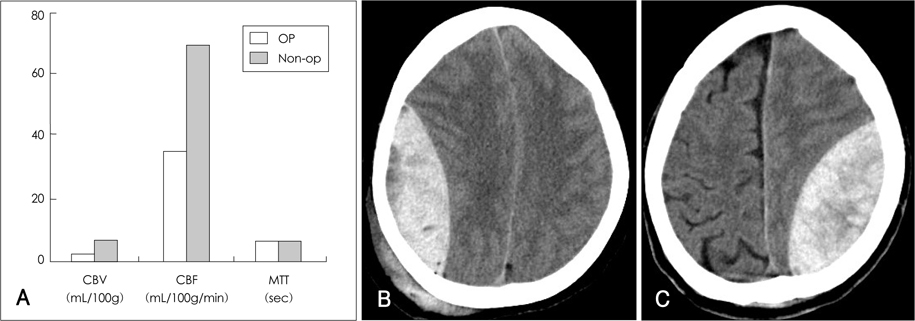
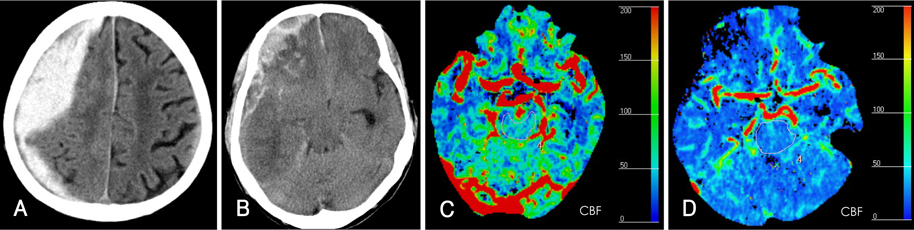
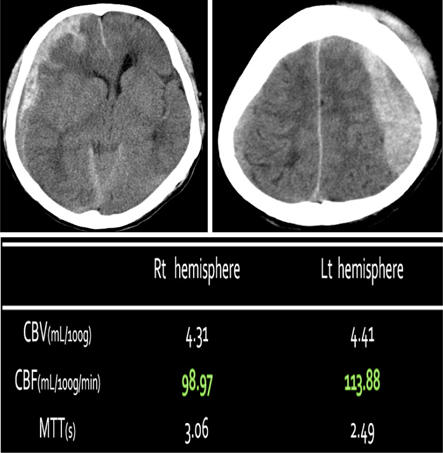
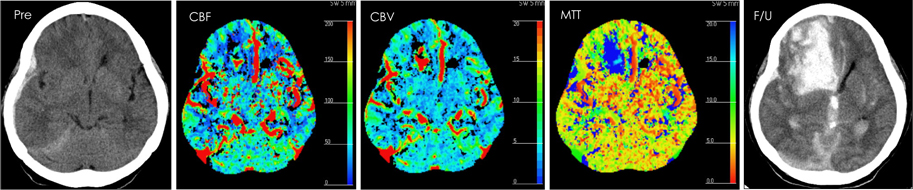
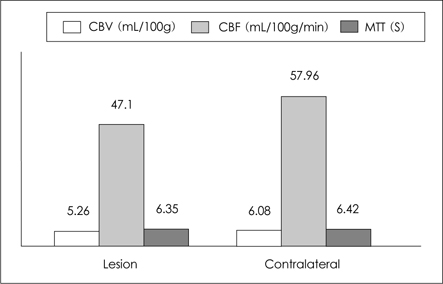
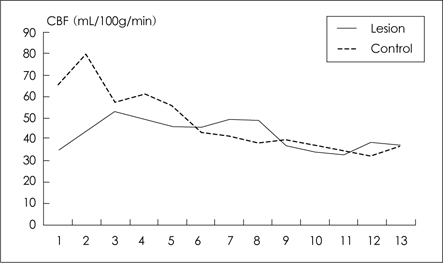
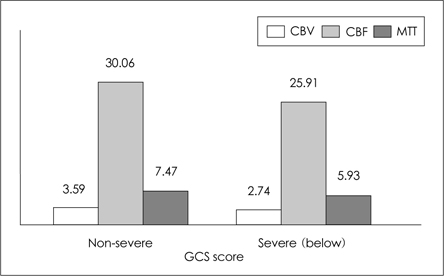
33 patients with head trauma were evaluated and the patients were classified into 4 categories: traumatic subarachnoid hemorrhage (T-SAH), actue epidural hematoma (EDH), acutue subdural hematoma (SDH), traumatic intracerebral hemorrhage (T-ICH). We evaluated the cerebral blood flow (CBF), cerebral blood volume (CBV), mean transit time (MTT) of the lesion vs contralateral lesion, lesion's hemisphere and brain stem vs contralateral side and compared them.
RESULTS
T-SAH was found in 7 cases. And the all T-SAH patients have no perfusion defect and they have no ischemic change on follow up brain CT. EDH was found in 11 cases. 3 of the 11 EDH patients have perfusion defect that was not revealed by non-contrast CT. According to the EDH size, brain stem perfusion value was different. And at the same size of EDH, the value was low if patients have low initial GCS. SDH was found in 9 cases. The 2 cases have different operation. Decompressive craniectomy was made for one patient who have low perfusion value of brain stem. And osteoplastic craniotomy was made for the other patient who have relative high perfusion value. The low perfusion value of brain stem was correleated with brain swelling. T-ICH was found in 12 cases. Contusion sites have decreased perfusion value and the DTICH (delayed traumatic intracerebral hemorrhage) was developed perfusion defect area on initial CT brain perfusion.
CONCLUSION
The CBP give us meaningful information of traumatic brain injury that associated with patient's unexplained symptom, and may be useful for deciding operative plan, and predicting the prognosis of the patient.
Keyword
MeSH Terms
Figure
Reference
-
1. Andrews BT, Chiles BW 3rd, Olsen WL, Pitts LH. The effect of intracerebral hematoma location on the risk of brain-stem compression and on clinical outcome. J Neurosurg. 1988; 69:518–522.
Article2. Barzó P, Marmarou A, Fatouros P, Hayasaki K, Corwin F. Contribution of vasogenic and cellular edema to traumatic brain swelling measured by diffusion-weighted imaging. J Neurosurg. 1997; 87:900–907.
Article3. Fukamachi A, Nagaseki Y, Kohno K, Wakao T. The incidence and developmental process of delayed traumatic intracerebral haematomas. Acta Neurochir (Wien). 1985; 74:35–39.
Article4. Gudeman SK, Kishore PR, Miller JD, Girevendulis AK, Lipper MH, Becker DP. The genesis and significance of delayed traumatic intracerebral hematoma. Neurosurgery. 1979; 5:309–313.
Article5. Komeda Y, Kato H, Saito K, Morishita F, Mori Y. [Adverse effect of iodine contrast media.]. Hinyokika Kiyo. 1987; 33:183–186.6. Koide M, Nishizawa S, Ohta S, Yokoyama T, Namba H. Chronological changes of the contractile mechanism in prolonged vasospasm after subarachnoid hemorrhage: from protein kinase C to protein tyrosine kinase. Neurosurgery. 2002; 51:1468–1474. discussion 1474-1476.
Article7. Kim JT, Shin DS, Nam TS, Jung ES, Choi SM, Son EJ, et al. Clinical usefulness of perfusion CT in acute ischemic stroke. J Korean Neurol Assoc. 2002; 20:585–591.8. Kim PG, Whang K, Cho SM, Kim HJ, Lee MS, Kim MS. Perfusion brain magnetic resonance image in patients of head trauma. J Korean Neurosurg Soc. 2002; 32:448–452.9. Martin NA, Patwardhan RV, Alexander MJ, Africk CZ, Lee JH, Shalmon E, et al. Characterization of cerebral hemodynamic phases following severe head trauma: hypoperfusion, hyperemia, and vasospasm. J Neurosurg. 1997; 87:9–19.
Article10. Sander D, Klingelhöfer J. Cerebral vasospasm following post-traumatic subarachnoid hemorrhage evaluated by transcranial Doppler ultrasonography. J Neurol Sci. 1993; 119:1–7.
Article11. Smith DH, Meaney DF, Lenkinski RE, Alsop DC, Grossman R, Kimura H, et al. New magnetic resonance imaging techniques for the evaluation of traumatic brain injury. J Neurotrauma. 1995; 12:573–577.
Article12. Wintermark M, van Melle G, Schnyder P, Revelly JP, Porchet F, Regli L, Meuli R, Maeder P, Chiolero R. Admission perfusion CT: prognostic value in patients with severe head trauma. Radiology. 2004; 232:211–220.
Article13. Wu CW, Liu HL, Chen JH, Yang Y. Effects of CBV, CBF, and blood-brain barrier permeability on accuracy of PASL and VASO measurement. Magn Reson Med. 2010; 63:601–608.
Article14. Xie A, Aihara Y, Bouryi VA, Nikitina E, Jahromi BS, Zhang ZD, et al. Novel mechanism of endothelin-1-induced vasospasm after subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2007; 27:1692–1701.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Initial Evaluation of Patients with Head Injury using CT Brain Perfusion Imaging in the Emergency Room: Two Cases
- The Role of Tc-99m HMPAO Brain Perfusion SPECT in the Psychiatric Disability Evaluation of Patients with Chronic Traumatic Brain Injury
- Traumatic Brain injury and Sleep Disorder
- Animal Models of Traumatic Brain Injury
- Anesthetic management of the traumatic brain injury patients undergoing non-neurosurgery