J Korean Neurosurg Soc.
2015 Sep;58(3):197-204. 10.3340/jkns.2015.58.3.197.
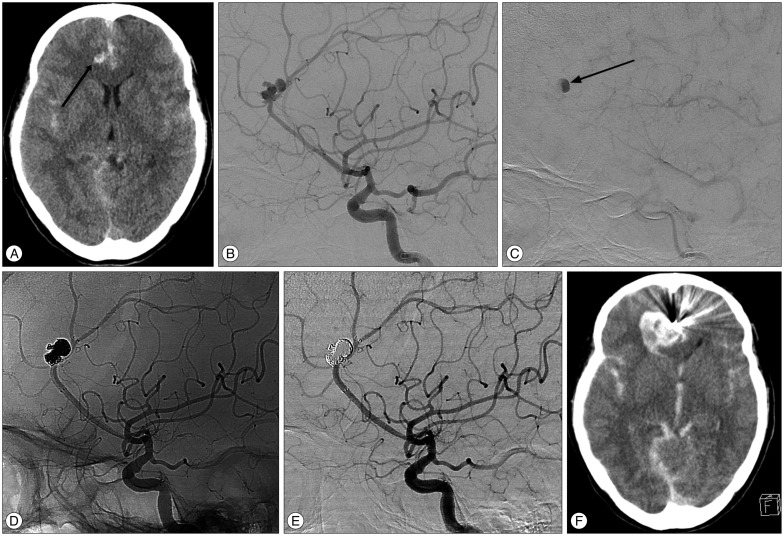
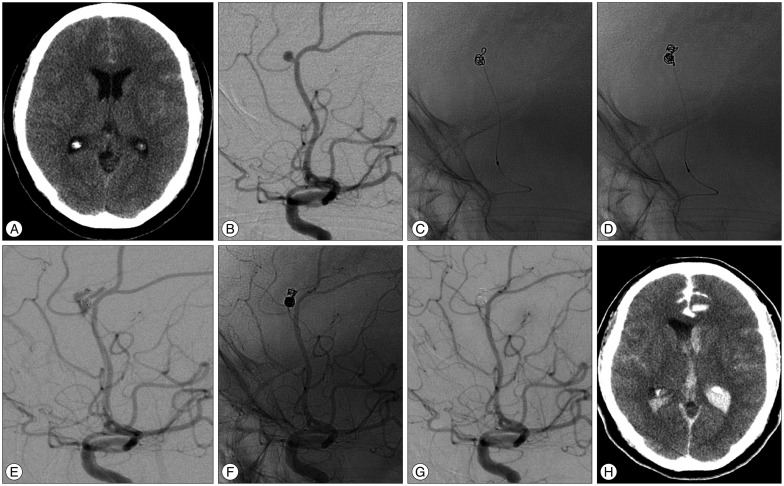
Endovascular Treatment of Ruptured Pericallosal Artery Aneurysms
- Affiliations
-
- 1Department of Neurosurgery, Medical Research Institute, Pusan National University Hospital, Busan, Korea. chwachoi@pusan.ac.kr
- 2Department of Diagnostic Radiology, Medical Research Institute, Pusan National University Hospital, Busan, Korea.
- 3Department of Biostatistics, Medical Research Institute, Pusan National University Hospital, Busan, Korea.
- KMID: 2191360
- DOI: http://doi.org/10.3340/jkns.2015.58.3.197
Abstract
OBJECTIVE
Aneurysms arising from the pericallosal artery (PA) are uncommon and challenging to treat. The aim of this study was to report our experiences of the endovascular treatment of ruptured PA aneurysms.
METHODS
From September 2003 to December 2013, 30 ruptured PA aneurysms in 30 patients were treated at our institution via an endovascular approach. Procedural data, clinical and angiographic results were retrospectively reviewed.
RESULTS
Regarding immediate angiographic control, complete occlusion was achieved in 21 (70.0%) patients and near-complete occlusion in 9 (30.0%). Eight procedure-related complications occurred, including intraprocedural rupture and early rebleeding in three each, and thromboembolic event in two. At last follow-up, 18 patients were independent with a modified Rankin Scale (mRS) score of 0-2, and the other 12 were either dependent or had expired (mRS score, 3-6). Adjacent hematoma was found to be associated with an increased risk of poor clinical outcome. Seventeen of 23 surviving patients underwent follow-up conventional angiography (mean, 16.5 months). Results showed stable occlusion in 14 (82.4%), minor recanalization in two (11.8%), and major recanalization, which required recoiling, in one (5.9%).
CONCLUSION
Our experiences demonstrate that endovascular treatment for a ruptured PA aneurysms is both feasible and effective. However, periprocedural rebleedings were found to occur far more often (20.0%) than is generally suspected and to be associated with preoperative contrast retention. Analysis showed existing adjacent hematoma is predictive of a poor clinical outcome.
MeSH Terms
Figure
Reference
-
1. Chalif DJ, Weinberg JS. Surgical treatment of aneurysms of the anterior cerebral artery. Neurosurg Clin N Am. 1998; 9:797–821. PMID: 9738108.
Article2. Cho YD, Lee JY, Seo JH, Kang HS, Kim JE, Kwon OK, et al. Early recurrent hemorrhage after coil embolization in ruptured intracranial aneurysms. Neuroradiology. 2012; 54:719–726. PMID: 21969241.
Article3. de Sousa AA, Dantas FL, de Cardoso GT, Costa BS. Distal anterior cerebral artery aneurysms. Surg Neurol. 1999; 52:128–135. discussion 135-136PMID: 10447278.
Article4. Hernesniemi J, Tapaninaho A, Vapalahti M, Niskanen M, Kari A, Luukkonen M. Saccular aneurysms of the distal anterior cerebral artery and its branches. Neurosurgery. 1992; 31:994–998. discussion 998-999PMID: 1470334.
Article5. Huang Q, Shen J, Xu Y, Liu J. Endovascular treatment of ruptured distal anterior cerebral artery aneurysm. Neurol India. 2010; 58:259–263. PMID: 20508346.
Article6. Jartti P, Isokangas JM, Karttunen A, Jartti A, Haapea M, Koskelainen T, et al. Early rebleeding after coiling of ruptured intracranial aneurysms. Acta Radiol. 2010; 51:1043–1049. PMID: 20849318.
Article7. Johnston SC, Dowd CF, Higashida RT, Lawton MT, Duckwiler GR, Gress DR, et al. Predictors of rehemorrhage after treatment of ruptured intracranial aneurysms : the Cerebral Aneurysm Rerupture After Treatment (CARAT) study. Stroke. 2008; 39:120–125. PMID: 18048860.
Article8. Kassell NF, Torner JC. Size of intracranial aneurysms. Neurosurgery. 1983; 12:291–297. PMID: 6843800.
Article9. Keston P, White PM, Horribine L, Sellar R. The endovascular management of pericallosal artery aneurysms. J Neuroradiol. 2004; 31:384–390. PMID: 15687957.
Article10. Lee JW, Lee KC, Kim YB, Huh SK. Surgery for distal anterior cerebral artery aneurysms. Surg Neurol. 2008; 70:153–159. discussion 159PMID: 18482760.
Article11. Lehecka M, Lehto H, Niemelä M, Juvela S, Dashti R, Koivisto T, et al. Distal anterior cerebral artery aneurysms : treatment and outcome analysis of 501 patients. Neurosurgery. 2008; 62:590–601. discussion 590-601PMID: 18425008.12. Martines F, Blundo C, Chiappetta F. Surgical treatment of the distal anterior cerebral artery aneurysms. J Neurosurg Sci. 1996; 40:189–194. PMID: 9165426.13. Menovsky T, van Rooij WJ, Sluzewski M, Wijnalda D. Coiling of ruptured pericallosal artery aneurysms. Neurosurgery. 2002; 50:11–14. discussion 14-15PMID: 11844229.
Article14. Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms : a randomised trial. Lancet. 2002; 360:1267–1274. PMID: 12414200.
Article15. Nguyen TN, Raymond J, Roy D, Chagnon M, Weill A, Iancu-Gontard D, et al. Endovascular treatment of pericallosal aneurysms. J Neurosurg. 2007; 107:973–976. PMID: 17977269.
Article16. Nomura M, Kida S, Uchiyama N, Yamashima T, Yoshikawa J, Yamashita J, et al. Ruptured irregularly shaped aneurysms : pseudoaneurysm formation in a thrombus located at the rupture site. J Neurosurg. 2000; 93:998–1002. PMID: 11117874.
Article17. Oishi H, Nonaka S, Yamamoto M, Arai H. Feasibility and efficacy of endovascular therapy for ruptured distal anterior cerebral artery aneurysms. Neurol Med Chir (Tokyo). 2013; 53:304–309. PMID: 23708221.
Article18. Pandey A, Rosenwasser RH, Veznedaroglu E. Management of distal anterior cerebral artery aneurysms : a single institution retrospective analysis (1997-2005). Neurosurgery. 2007; 61:909–916. discussion 916-917PMID: 18091267.19. Park HS, Kwon SC, Kim MH, Park ES, Sim HB, Lyo IU. Endovascular coil embolization of distal anterior cerebral artery aneurysms : angiographic and clinical follow-up results. Neurointervention. 2013; 8:87–91. PMID: 24024072.
Article20. Park KY, Kim BM, Lim YC, Chung J, Kim DJ, Joo JY, et al. The role of endovascular treatment for ruptured distal anterior cerebral artery aneurysms : comparison with microsurgical clipping. J Neuroimaging. 2015; 25:81–86. PMID: 24299470.
Article21. Proust F, Toussaint P, Hannequin D, Rabenenoïna C, Le Gars D, Fréger P. Outcome in 43 patients with distal anterior cerebral artery aneurysms. Stroke. 1997; 28:2405–2409. PMID: 9412622.
Article22. Sluzewski M, van Rooij WJ. Early rebleeding after coiling of ruptured cerebral aneurysms : incidence, morbidity, and risk factors. AJNR Am J Neuroradiol. 2005; 26:1739–1743. PMID: 16091523.23. Sturiale CL, Brinjikji W, Murad MH, Cloft HJ, Kallmes DF, Lanzino G. Endovascular treatment of distal anterior cerebral artery aneurysms : single-center experience and a systematic review. AJNR Am J Neuroradiol. 2013; 34:2317–2320. PMID: 23868164.
Article24. Suzuki S, Kurata A, Yamada M, Iwamoto K, Nakahara K, Sato K, et al. Outcomes analysis of ruptured distal anterior cerebral artery aneurysms treated by endosaccular embolization and surgical clipping. Interv Neuroradiol. 2011; 17:49–57. PMID: 21561558.
Article25. Waldenberger P, Petersen J, Chemelli A, Schenk C, Gruber I, Strasak A, et al. Endovascular therapy of distal anterior cerebral artery aneurysms-an effective treatment option. Surg Neurol. 2008; 70:368–377. PMID: 18291498.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pterional or Subfrontal Access for Proximal Vascular Control in Anterior Interhemispheric Approach for Ruptured Pericallosal Artery Aneurysms at Risk of Premature Rupture
- Traumatic Aneurysm of the Pericallosal artery
- Frequency and Characteristics of Paraclinoid Aneurysm in Ruptured Cerebral Aneurysms
- Endovascular Treatment of Basilar Bifurcation Aneurysm with Open Access of Vertebral Artery
- Current Update on the Randomized Controlled Trials of Intracranial Aneurysms