J Korean Neurosurg Soc.
2024 Jan;67(1):22-30. 10.3340/jkns.2023.0059.
Frequency and Characteristics of Paraclinoid Aneurysm in Ruptured Cerebral Aneurysms
- Affiliations
-
- 1Department of Neurosurgery, Medical Science College, Tokai University, Kanagawa, Japan
- KMID: 2550456
- DOI: http://doi.org/10.3340/jkns.2023.0059
Abstract
Objective
: This study aimed to determine the frequency of paraclinoid aneurysms among ruptured cerebral aneurysms and compare paraclinoid aneurysms with other aneurysms to clarify the characteristics of ruptured paraclinoid aneurysms.
Methods
: This study included 970 ruptured cerebral aneurysms treated at our hospital between 2003 and 2020.
Results
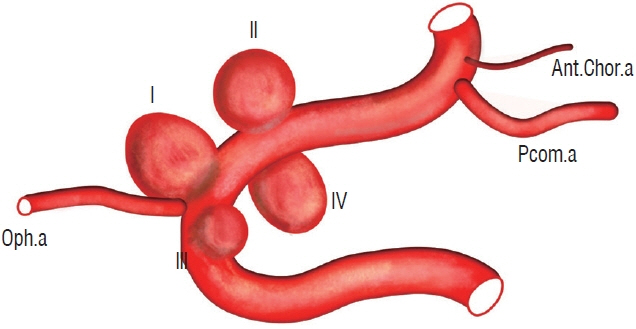
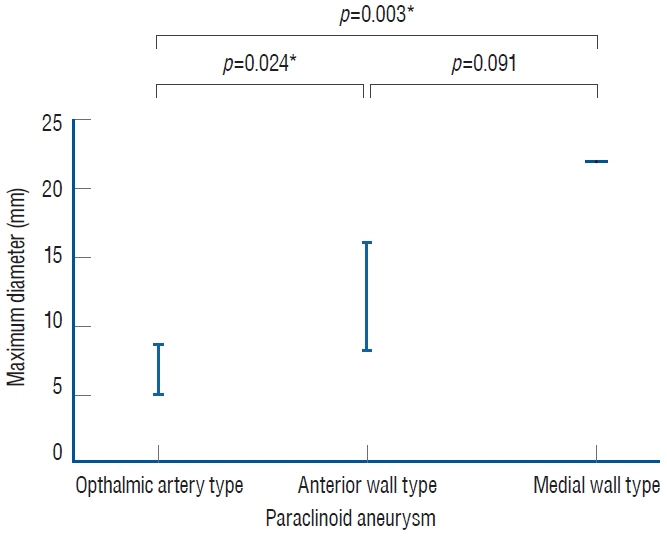
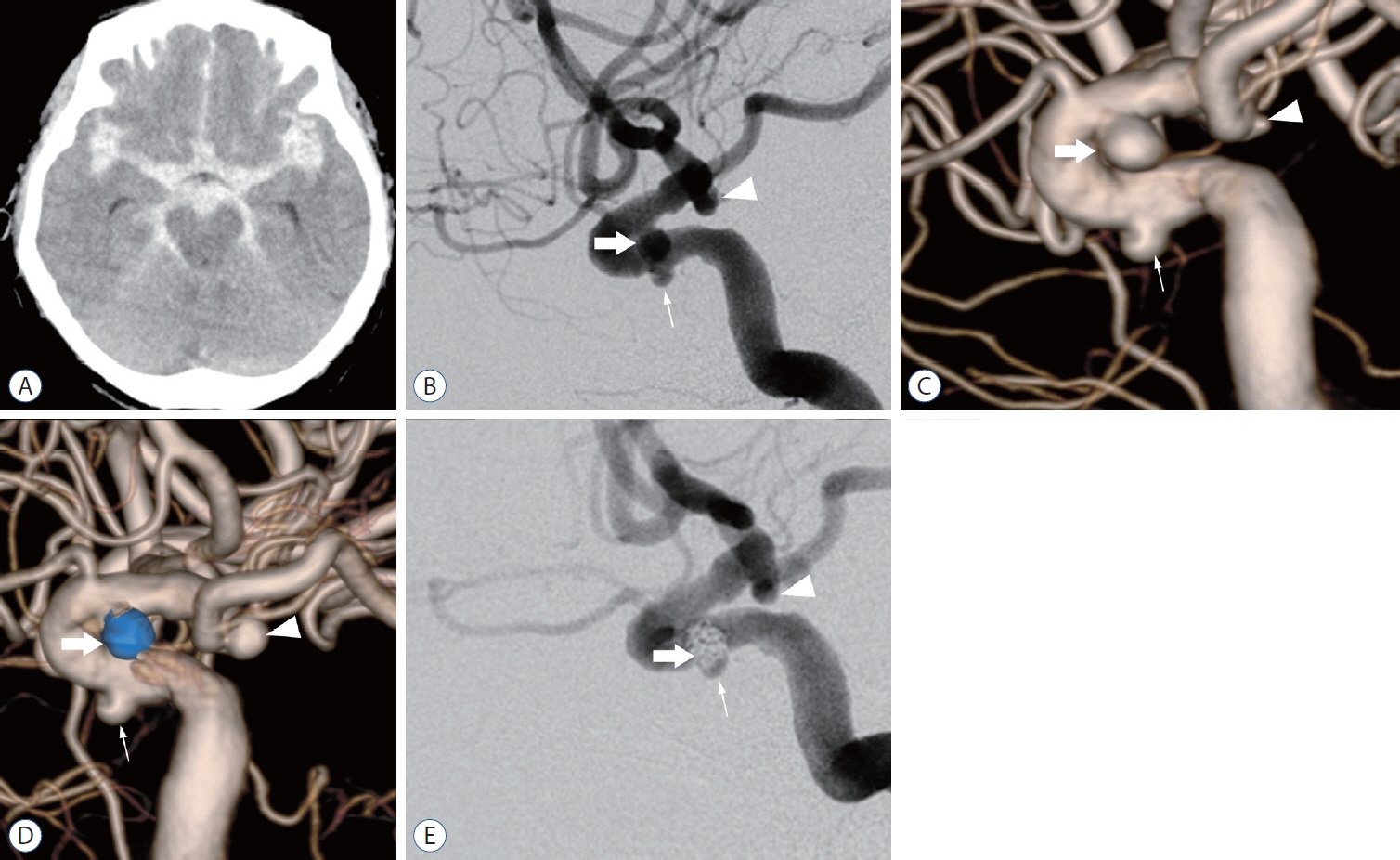
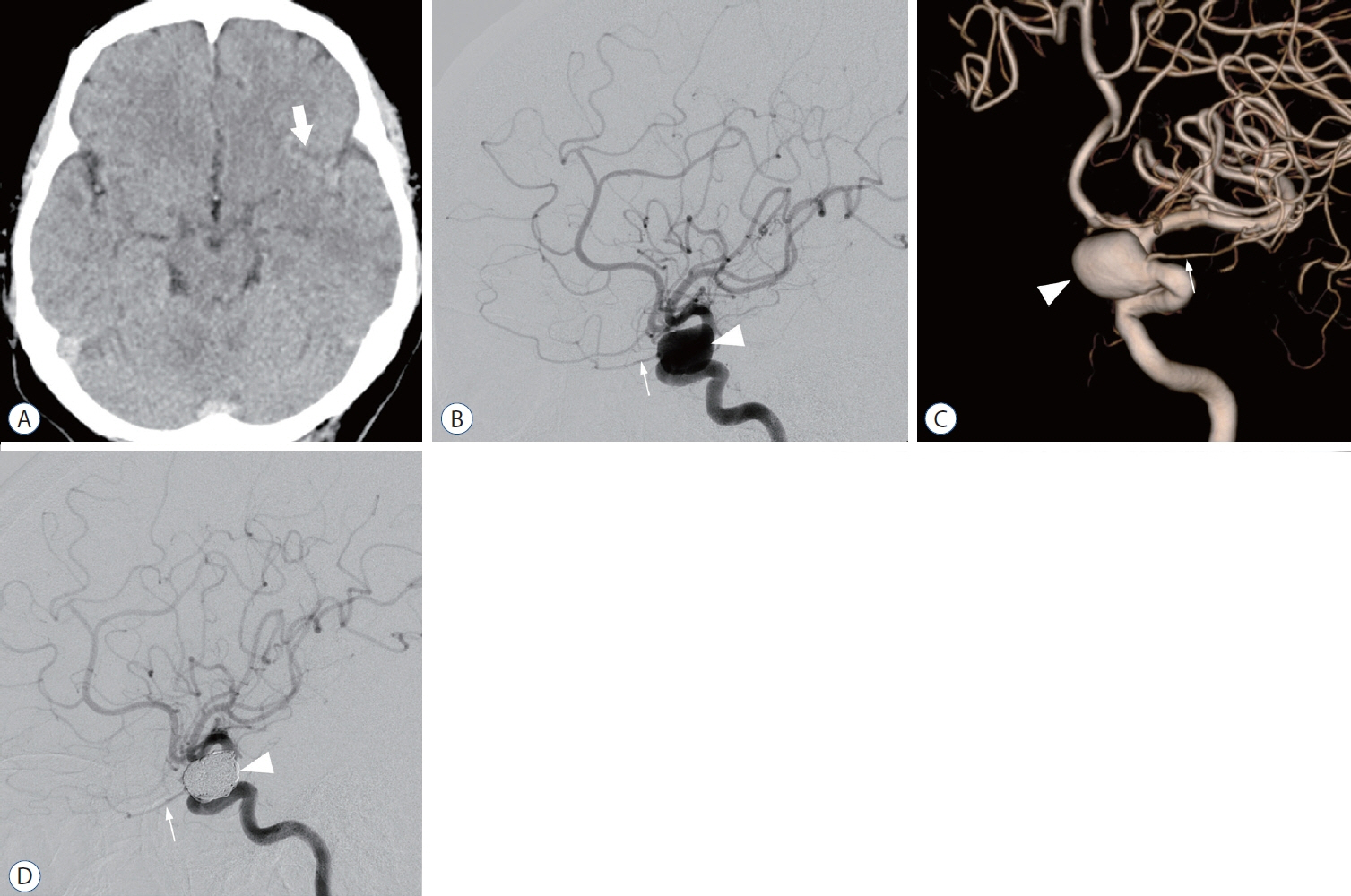
: There were 15 cases (1.3%) of paraclinoid aneurysms with maximum diameters of 5–22 mm (mean±standard deviation [SD], 11.6±5.4 mm). Treatment consisted of clipping in four patients and endovascular treatment in 11. Factors significantly different in multivariate analysis for paraclinoid aneurysms compared with those for other aneurysms were a history of hypertension (odds ratio [OR], 1.2–9.8; p=0.021) and aneurysm ≥10 mm (OR, 7.5–390.3; p<0.001). The sites of paraclinoid aneurysm were ophthalmic artery type in nine patients, anterior wall type in five, medial wall type in one, and ventral wall type in zero. The medial wall type (22 mm) was significantly larger than the ophthalmic artery type (mean±SD, 7.2±2.0 mm) (p=0.003), and the anterior wall type (mean±SD, 12.2±4.8 mm) was significantly larger than the ophthalmic artery type (p=0.024).
Conclusion
: This study showed a low frequency of paraclinoid aneurysms among ruptured cerebral aneurysms. Most were upward-facing with relatively large aneurysms, and no aneurysms were smaller than 5 mm. With recent advances in endovascular treatment devices, paraclinoid aneurysms are easily treatable. However, the treatment indication of each paraclinoid aneurysm should be carefully considered.
Figure
Reference
-
References
1. Barami K, Hernandez VS, Diaz FG, Guthikonda M. Paraclinoid carotid aneurysms: surgical management, complications, and outcome based on a new classification scheme. Skull Base. 13:31–41. 2003.
Article2. Fukaya S, Kawamoto S, Kikuchi S, Sumi T, Kawano R, Okunuki K, et al. Clinical management of unruptured paraclinoid aneurysm according to the CISS image and the observation period of 5 years on average. Nosocyu no Geka. 49:367–372. 2021.
Article3. Greving JP, Wermer MJ, Brown RD Jr, Morita A, Juvela S, Yonekura M, et al. Development of the PHASES score for prediction of risk of rupture of intracranial aneurysms: a pooled analysis of six prospective cohort studies. Lancet Neurol. 13:59–66. 2014.
Article4. Imaizumi Y, Mizutani T, Shimizu K, Sato Y, Taguchi J. Detection rates and sites of unruptured intracranial aneurysms according to sex and age: an analysis of MR angiography-based brain examinations of 4070 healthy Japanese adults. J Neurosurg. 130:573–578. 2018.
Article5. Jeon JS, Ahn JH, Huh W, Son YJ, Bang JS, Kang HS, et al. A retrospective analysis on the natural history of incidental small paraclinoid unruptured aneurysm. J Neurol Neurosurg Psychiatry. 85:289–294. 2014.
Article6. Jin SC, Kwon DH, Ahn JS, Kwun BD, Song Y, Choi CG. Clinical and radiogical outcomes of endovascular detachable coil embolization in paraclinoid aneurysms : a 10-year experience. J Korean Neurosurg Soc. 45:5–10. 2009.
Article7. Kalluri AG, Sukumaran M, Nazari P, Golnari P, Ansari SA, Hurley MC, et al. Retrospective review of 290 small carotid cave aneurysms over 17 years. J Neurosurg. 133:1473–1477. 2019.
Article8. Kinouchi H, Mizoi K, Nagamine Y, Yanagida N, Mikawa S, Suzuki A, et al. Anterior paraclinoid aneurysms. J Neurosurg. 96:1000–1005. 2002.
Article9. Loumiotis I, D’Urso PI, Tawk R, Cloft HJ, Kallmes DF, Kairouz V, et al. Endovascular treatment of ruptured paraclinoid aneurysms: results, complications, and follow-up. AJNR Am J Neuroradiol. 33:632–637. 2012.
Article10. Molyneux AJ, Clarke A, Sneade M, Mehta Z, Coley S, Roy D, et al. Cerecyte coil trial: angiographic outcomes of a prospective randomized trial comparing endovascular coiling of cerebral aneurysms with either cerecyte or bare platinum coils. Stroke. 43:2544–2550. 2012.11. Nguyen TN, Raymond J, Guilbert F, Roy D, Bérubé MD, Mahmoud M, et al. Association of endovascular therapy of very small ruptured aneurysms with higher rates of procedure-related rupture. J Neurosurg. 108:1088–1092. 2008.
Article12. Oh SY, Kim MJ, Kim BM, Lee KS, Kim BS, Shin YS. Angiographic characteristics of ruptured paraclinoid aneurysms: risk factors for rupture. Acta Neurochir (Wien). 155:1493–1499. 2013.
Article13. Park HK, Horowitz M, Jungreis C, Genevro J, Koebbe C, Levy E, et al. Periprocedural morbidity and mortality associated with endovascular treatment of intracranial aneurysms. AJNR Am J Neuroradiol. 26:506–514. 2005.14. Shimizu K, Imamura H, Mineharu Y, Adachi H, Sakai C, Sakai N. Endovascular treatment of unruptured paraclinoid aneurysms: single-center experience with 400 cases and literature review. AJNR Am J Neuroradiol. 37:679–685. 2016.
Article15. Sorimachi T, Ito Y, Morita K, Jimbo Y, Nishino K, Sasaki O, et al. Longterm follow-up of intra-aneurysmal coil embolization for unruptured paraclinoid aneurysms. Neurol Res. 34:864–870. 2012.
Article16. Sturiale CL, Auricchio AM, Stifano V, Maugeri R, Albanese A. Timing and outcome of bystanders treatment in patients with subarachnoid hemorrhage associated with multiple aneurysms. Neurosurg Rev. 45:2837–2844. 2022.
Article17. Tominari S, Morita A, Ishibashi T, Yamazaki T, Takao H, Murayama Y, et al. Prediction model for 3-year rupture risk of unruptured cerebral aneurysms in Japanese patients. Ann Neurol. 77:1050–1059. 2015.
Article18. UCAS Japan Investigators, Morita A, Kirino T, Hashi K, Aoki N, Fukuhara S, et al. The natural course of unruptured cerebral aneurysms in a Japanese cohort. N Engl J Med. 366:2474–2482. 2012.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Progressive Visual Loss after Endovascular Coiling Treatment of a Large Paraclinoid Aneurysm
- Surgical Treatment of Unruptured Cerebral Aneurysms
- Unruptured Paraclinoid Carotid Aneurysms Occur More Frequently in Younger Ages
- A Ruptured Aneurysm in a Patient with Systemic Lupus Erythematosus: Case Report
- A Study of Morphological Characteristics of Cerebral Aneurysms