J Korean Neurosurg Soc.
2015 Feb;57(2):127-130. 10.3340/jkns.2015.57.2.127.
Paradoxical Exacerbation of Symptoms with Obstruction of the Venous Outflow after Gamma Knife Radiosurgery for Treatment of a Dural Arteriovenous Fistula of the Cavernous Sinus
- Affiliations
-
- 1Department of Neurosurgery, Medical Research Institute, Pusan National University Hospital, Busan, Korea. chwachoi@pusan.ac.kr
- 2Department of Diagnostic Radiology, Medical Research Institute, Pusan National University Hospital, Busan, Korea.
- KMID: 2191195
- DOI: http://doi.org/10.3340/jkns.2015.57.2.127
Abstract
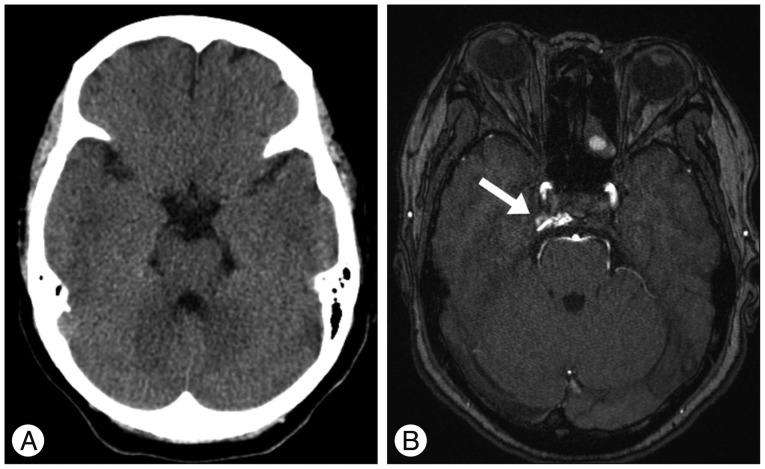
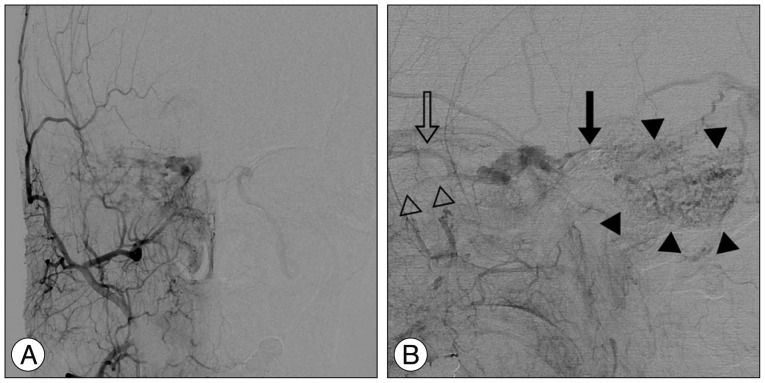
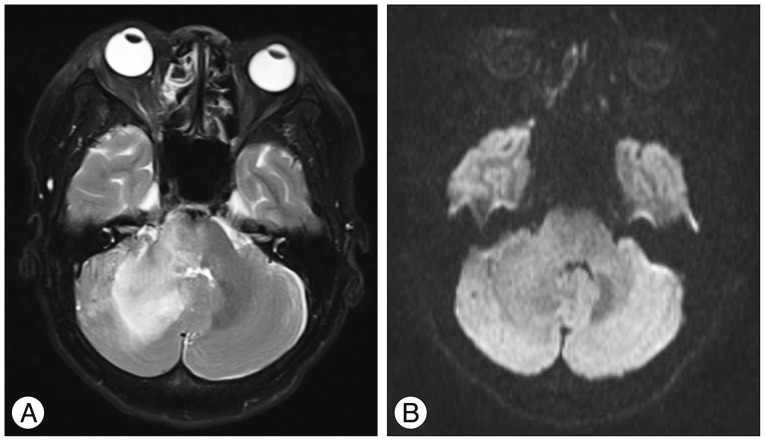
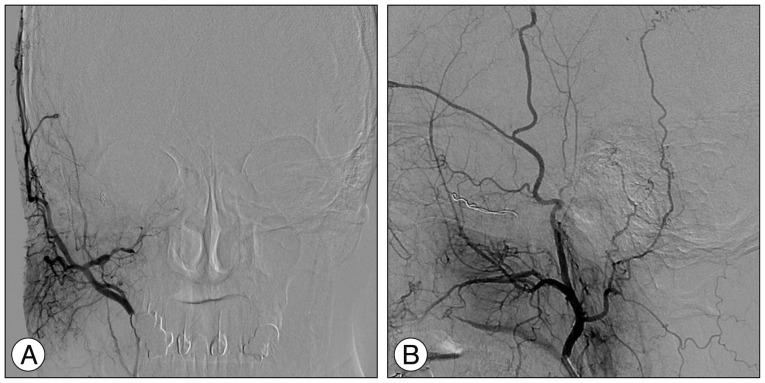
- A 59-year-old female presented with progressive right proptosis, chemosis and ocular pain. An imaging work-up including conventional catheter angiography showed a right-sided dural arteriovenous fistula of the cavernous sinus, which drained into the right superior petrosal sinus, right superior ophthalmic vein, and right inferior ophthalmic vein, and cortical venous reflux was seen via the right petrosal vein in the right posterior fossa. After failure of transvenous embolization, the patient underwent Gamma Knife radiosurgery (GKRS). At one month after GKRS, she developed increasing ocular pain and occipital headache. Repeat angiography showed partial obliteration of the fistula and loss of drainage via the superior and inferior ophthalmic veins with severe congestion, resulting in slow flow around the right cerebellar hemisphere. Prompt transarterial embolization relieved the patient's ocular symptoms and headache. We report on a case of paradoxical exacerbation of symptoms resulting from obstruction of the venous outflow after GKRS for treatment of a dural arteriovenous fistula of the cavernous sinus.
MeSH Terms
Figure
Reference
-
1. Barcia-Salorio JL, Soler F, Barcia JA, Hernández G. Stereotactic radiosurgery for the treatment of low-flow carotid-cavernous fistulae : results in a series of 25 cases. Stereotact Funct Neurosurg. 1994; 63:266–270. PMID: 7624645.
Article2. Chiou HJ, Chou YH, Guo WY, Teng MM, Hsu CC, Tiu CM, et al. Verifying complete obliteration of carotid artery-cavernous sinus fistula : role of color Doppler ultrasonography. J Ultrasound Med. 1998; 17:289–295. PMID: 9586700.
Article3. Choi BS, Park JW, Kim JL, Kim SY, Park YS, Kwon HJ, et al. Treatment Strategy Based on Multimodal Management Outcome of Cavernous Sinus Dural Arteriovenous Fistula (CSDAVF). Neurointervention. 2011; 6:6–12. PMID: 22125741.
Article4. Dalyai RT, Ghobrial G, Chalouhi N, Dumont AS, Tjoumakaris S, Gonzalez LF, et al. Radiosurgery for dural arterio-venous fistulas : a review. Clin Neurol Neurosurg. 2013; 115:512–516. PMID: 23481896.5. Flickinger JC, Kondziolka D, Maitz AH, Lunsford LD. An analysis of the dose-response for arteriovenous malformation radiosurgery and other factors affecting obliteration. Radiother Oncol. 2002; 63:347–354. PMID: 12142099.
Article6. Ghobrial GM, Marchan E, Nair AK, Dumont AS, Tjoumakaris SI, Gonzalez LF, et al. Dural arteriovenous fistulas : a review of the literature and a presentation of a single institution's experience. World Neurosurg. 2013; 80:94–102. PMID: 22381858.
Article7. Jung HH, Chang JH, Whang K, Pyen JS, Chang JW, Park YG. Gamma Knife surgery for low-flow cavernous sinus dural arteriovenous fistulas. J Neurosurg. 2010; 113(Suppl):21–27. PMID: 21121783.
Article8. Kida Y. Radiosurgery for dural arteriovenous fistula. Prog Neurol Surg. 2009; 22:38–44. PMID: 18948718.
Article9. Korkmazer B, Kocak B, Tureci E, Islak C, Kocer N, Kizilkilic O. Endovascular treatment of carotid cavernous sinus fistula : a systematic review. World J Radiol. 2013; 5:143–155. PMID: 23671750.
Article10. Lau LI, Wu HM, Wang AG, Yen MY, Hsu WM. Paradoxical worsening with superior ophthalmic vein thrombosis after gamma knife radiosurgery for dural arteriovenous fistula of cavernous sinus : a case report suggesting the mechanism of the phenomenon. Eye (Lond). 2006; 20:1426–1428. PMID: 16485013.
Article11. Loumiotis I, Lanzino G, Daniels D, Sheehan J, Link M. Radiosurgery for intracranial dural arteriovenous fistulas (DAVFs) : a review. Neurosurg Rev. 2011; 34:305–315. discussion 315. PMID: 21584687.
Article12. O'Leary S, Hodgson TJ, Coley SC, Kemeny AA, Radatz MW. Intracranial dural arteriovenous malformations : results of stereotactic radiosurgery in 17 patients. Clin Oncol (R Coll Radiol). 2002; 14:97–102. PMID: 12069135.13. Onizuka M, Mori K, Takahashi N, Kawahara I, Hiu T, Toda K, et al. Gamma knife surgery for the treatment of spontaneous dural carotid-cavernous fistulas. Neurol Med Chir (Tokyo). 2003; 43:477–482. discussion 482-483. PMID: 14620198.
Article14. Pan HC, Sun MH, Yang DY, Wang YC, Lee SD, Chen WH, et al. Multidisciplinary treatment of cavernous sinus dural arteriovenous fistulae with radiosurgery and embolization. J Clin Neurosci. 2005; 12:744–749. PMID: 16169730.
Article15. Pollock BE, Nichols DA, Garrity JA, Gorman DA, Stafford SL. Stereotactic radiosurgery and particulate embolization for cavernous sinus dural arteriovenous fistulae. Neurosurgery. 1999; 45:459–466. discussion 466-467. PMID: 10493367.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Dural Arterio-venous Malformation Involving the Cavernous Sinus
- Transvenous Embolization of Cavernous Sinus Dural Arteriovenous Fistula Using the Direct Superior Ophthalmic Vein Approach: A Case Report
- Endovascular management of cavernous sinus dural arteriovenous fistulas: Overall review and considerations
- Facilitated Retrograde Access via the Facial Vein for Transvenous Embolization of the Cavernous Sinus Dural Arteriovenous Fistula with Isolated Ophthalmic Venous Drainage
- Middle temporal vein access for transvenous embolization of Cavernous sinus dural arteriovenous fistula: A case report and review of literature