J Korean Neurosurg Soc.
2012 Jan;51(1):37-39. 10.3340/jkns.2012.51.1.37.
Massive Intracerebral Hemorrhage Caused by a Cavernous Malformation
- Affiliations
-
- 1Department of Neurosurgery, Medical Reserch Institute, Pusan National University Hospital, Busan, Korea. redcheek09@naver.com
- KMID: 2190466
- DOI: http://doi.org/10.3340/jkns.2012.51.1.37
Abstract
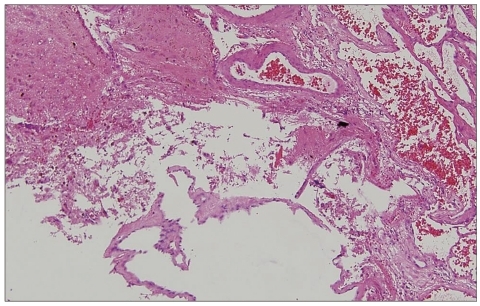
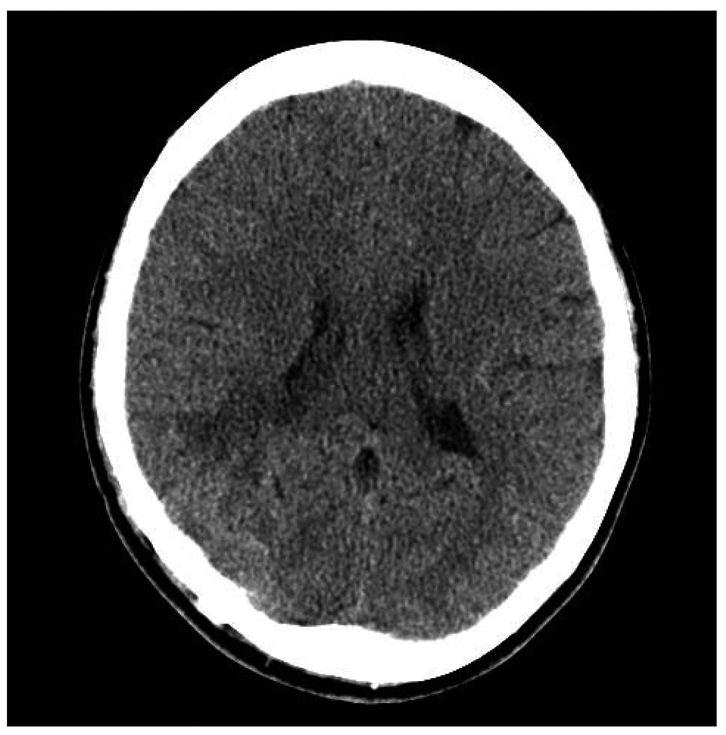
- We present a rare case of massive intracerebral hemorrhage resulting from a small, superficially-located supratentorial cavernous malformation, or cavernoma. These lesions rarely lead to massive, life-threatening intracerebral hemorrhages. A 17-year-old female presented with a 3-week history of declining mental status. Brain computed tomography and magnetic resonance imaging revealed a sizable intracranial hemorrhage, within the right occipital region, associated with a small nodule at the hematoma's posterior margin. An emergency operation removed the entire hematoma and nodule. Histological examination of the nodule was compatible with a diagnosis of cavernous malformation. The patient's post-operative course was uneventful.
MeSH Terms
Figure
Cited by 2 articles
-
Two Cases of Cavernous Malformation Presenting with Unusual and Large Intracerebral Hemorrhages
Yeon-Ju Choi, Ki-Su Park, Seong-Hyun Park, Jeong-Hyun Hwang
J Cerebrovasc Endovasc Neurosurg. 2015;17(1):32-35. doi: 10.7461/jcen.2015.17.1.32.Chronic Encapsulated Intracerebral Hematoma Associated with Cavernous Malformation
Satoru Takeuchi, Kojiro Wada, Fumihiro Sakakibara, Kentaro Mori
J Korean Neurosurg Soc. 2014;55(2):89-91. doi: 10.3340/jkns.2014.55.2.89.
Reference
-
1. Acciarri N, Galassi E, Giulioni M, Pozzati E, Grasso V, Palandri G, et al. Cavernous malformations of the central nervous system in the pediatric age group. Pediatr Neurosurg. 2009; 45:81–104. PMID: 19307743.
Article2. Aiba T, Tanaka R, Koike T, Kameyama S, Takeda N, Komata T. Natural history of intracranial cavernous malformations. J Neurosurg. 1995; 83:56–59. PMID: 7782850.
Article3. Avci E, Oztürk A, Baba F, Karabağ H, Cakir A. Huge cavernoma with massive intracerebral hemorrhage in a child. Turk Neurosurg. 2007; 17:23–26. PMID: 17918674.4. Chicani CF, Miller NR, Tamargo RJ. Giant cavernous malformation of the occipital lobe. J Neuroophthalmol. 2003; 23:151–153. PMID: 12782930.
Article5. Clatterbuck RE, Eberhart CG, Crain BJ, Rigamonti D. Ultrastructural and immunocytochemical evidence that an incompetent blood-brain barrier is related to the pathophysiology of cavernous malformations. J Neurol Neurosurg Psychiatry. 2001; 71:188–192. PMID: 11459890.
Article6. Consales A, Piatelli G, Ravegnani M, Pavanello M, Striano P, Zoli ML, et al. Treatment and outcome of children with cerebral cavernomas : a survey on 32 patients. Neurol Sci. 2010; 31:117–123. PMID: 19834644.
Article7. Corapçioğlu F, Akansel G, Gönüllü E, Yildiz K, Etuş V. Fatal giant pediatric intracranial cavernous angioma. Turk J Pediatr. 2006; 48:89–92. PMID: 16562795.8. D'Angelo VA, De Bonis C, Amoroso R, Cali A, D'Agruma L, Guarnieri V, et al. Supratentorial cerebral cavernous malformations : clinical, surgical, and genetic involvement. Neurosurg Focus. 2006; 21:e9. PMID: 16859262.9. Del Curling O Jr, Kelly DL Jr, Elster AD, Craven TE. An analysis of the natural history of cavernous angiomas. J Neurosurg. 1991; 75:702–708. PMID: 1919691.
Article10. Kim DS, Park YG, Choi JU, Chung SS, Lee KC. An analysis of the natural history of cavernous malformations. Surg Neurol. 1997; 48:9–17. discussion 17-18. PMID: 9199678.
Article11. Kivelev J, Niemelä M, Kivisaari R, Dashti R, Laakso A, Hernesniemi J. Long-term outcome of patients with multiple cerebral cavernous malformations. Neurosurgery. 2009; 65:450–455. discussion 455. PMID: 19687688.
Article12. Kondziolka D, Lunsford LD, Kestle JR. The natural history of cerebral cavernous malformations. J Neurosurg. 1995; 83:820–824. PMID: 7472549.
Article13. Kupersmith MJ, Kalish H, Epstein F, Yu G, Berenstein A, Woo H, et al. Natural history of brainstem cavernous malformations. Neurosurgery. 2001; 48:47–53. discussion 53-54. PMID: 11152360.
Article14. Porter RW, Detwiler PW, Spetzler RF, Lawton MT, Baskin JJ, Derksen PT, et al. Cavernous malformations of the brainstem : experience with 100 patients. J Neurosurg. 1999; 90:50–58. PMID: 10413155.15. Washington CW, McCoy KE, Zipfel GJ. Update on the natural history of cavernous malformations and factors predicting aggressive clinical presentation. Neurosurg Focus. 2010; 29:E7. PMID: 20809765.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Cavernous Malformation Presenting with Unusual and Large Intracerebral Hemorrhages
- Repeated Intracerebral Hemorrhage from Developmental Venous Anomaly Alone
- Traumatic Carotid-cavernous Fistula Bringing about Intracerebral Hemorrhage
- Surgical Treatment of Cavernous Malformation of Pineal Region
- Cavernous Malformation of the Optic Chiasm : Case Report