J Cerebrovasc Endovasc Neurosurg.
2015 Mar;17(1):32-35. 10.7461/jcen.2015.17.1.32.
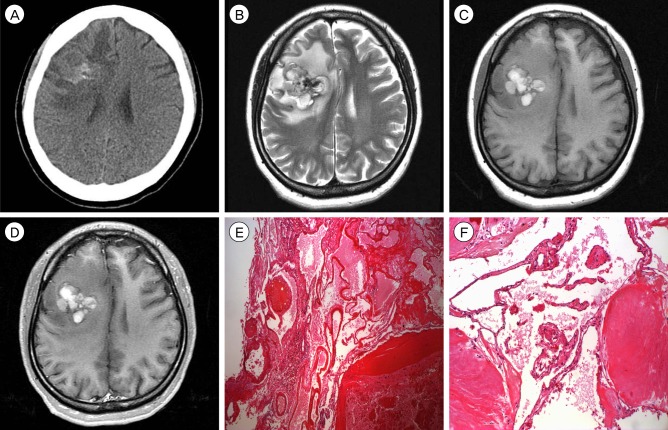
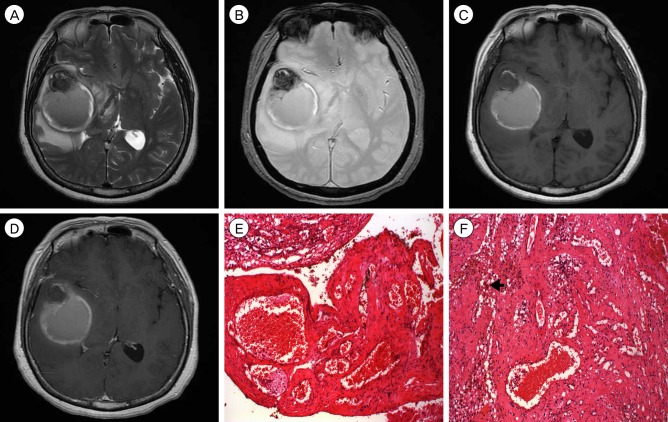
Two Cases of Cavernous Malformation Presenting with Unusual and Large Intracerebral Hemorrhages
- Affiliations
-
- 1Department of Neurosurgery, Kyungpook National University School of Medicine, Daegu, Korea. jhwang@knu.ac.kr
- KMID: 1963147
- DOI: http://doi.org/10.7461/jcen.2015.17.1.32
Abstract
- Cavernous malformations (CMs), characterized by the presence of a hemosiderin rim and intralesional hemorrhage, are relatively common intracranial vascular malformations. Extralesional hemorrhages arising from CMs are seen in a minority of cases, but most of them show typical CM findings on magnetic resonance imaging. Here, the authors report two cases of pathologically confirmed CM presenting with unusual and large intracerebral hemorrhages, which were not surrounded by the typical hemosiderin rim. CMs presenting with large intracerebral hemorrhage should be considered in the differential diagnosis of massive intracerebral hemorrhages.
MeSH Terms
Figure
Reference
-
1. Awad IA, Robinson JR Jr, Mohanty S, Estes ML. Mixed vascular malformations of the brain: clinical and pathogenetic considerations. Neurosurgery. 1993; 8. 33(2):179–188. PMID: 8367039.2. Chicani CF, Miller NR, Tamargo RJ. Giant cavernous malformation of the occipital lobe. J Neuroophthalmol. 2003; 6. 23(2):151–153. PMID: 12782930.
Article3. Corapçioğlu F, Akansel G, Gönüllü E, Yildiz K, Etuş V. Fatal giant pediatric intracranial cavernous angioma. Turk J Pediatr. 2006; Jan-Mar. 48(1):89–92. PMID: 16562795.4. Flemming KD, Link MJ, Christianson TJ, Brown RD Jr. Prospective hemorrhage risk of intracerebral cavernous malformations. Neurology. 2012; 2. 78(9):632–636. PMID: 22302553.
Article5. Furlan AJ, Whisnant JP, Elveback LR. The decreasing incidence of primary intracerebral hemorrhage: a population study. Ann Neurol. 1979; 4. 5(4):367–373. PMID: 375807.
Article6. Garner TB, Del Curling, Kelly DL Jr, Laster DW. The natural history of intracranial venous angiomas. J Neurosurg. 1991; 11. 75(5):715–722. PMID: 1919693.
Article7. Jain KK, Robertson E. Recurrence of an excised cavernous hemangioma in the opposite cerebral hemisphere. Case report. J Neurosurg. 1970; 10. 33(4):453–456. PMID: 5471935.8. Kim YS, Lee JI, Choi CH, Ko JK. Massive intracerebral hemorrhage caused by a cavernous malformation. J Korean Neurosurg Soc. 2012; 1. 51(1):37–39. PMID: 22396841.
Article9. Kondziolka D, Lunsford LD, Kestle JR. The natural history of cerebral cavernous malformations. J Neurosurg. 1995; 11. 83(5):820–824. PMID: 7472549.
Article10. Schmitt AJ, Mitha AP, Germain R, Eschbacher J, Spetzler RF. Subdural hematoma from a cavernous malformation. World Neurosurg. 2014; Sep-Oct. 82(3-4):535. e1-3. PMID: 23314025.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Massive Intracerebral Hemorrhage Caused by a Cavernous Malformation
- Analysis of Spontaneous Intracerebral Hematomas Confirmed by CT
- Traumatic Carotid-cavernous Fistula Bringing about Intracerebral Hemorrhage
- Dural Arteriovenous Malformation on the Anterior Cranial Fossa
- Surgical Treatment of Cavernous Malformation of Pineal Region