Radiation Exposure to the Orthopaedic Surgeon during Fracture Surgery
- Affiliations
-
- 1Department of Orthopedic Surgery, Asan Medical Center, Uiversity of Ulsan College of Medicine, Seoul, Korea. jjkim2@amc.seoul.kr
- 2Department of Orthopedic Surgery, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- KMID: 2185577
- DOI: http://doi.org/10.4055/jkoa.2010.45.2.107
Abstract
- PURPOSE
To assess the risk of radiation exposure by measuring the equivalent dose during fracture surgery.
MATERIALS AND METHODS
Two orthopedic trauma surgeons were enrolled in this study from April to June 2009. The equivalent dose was measured using thermoluminiscent dosimeters placed at the left (in and out of the lead apron).
RESULTS
The equivalent dose measured from the apron over the 3 month period were 5.22 mSv, 4.34 mSv(outside), and 1.83 mSv and 0.71 mSv(inside). The rate of radiation reduction was 64.9% and 83.6% respectively.
CONCLUSION
The estimated annual equivalent dose outside the apron was close to or higher than the maximum limit of radiation exposure. These findings highlight the need for surgeons to be more cautious about radiation exposure during fracture management and take active steps to minimize radiation exposure, such as wearing a radio-protective apron.
MeSH Terms
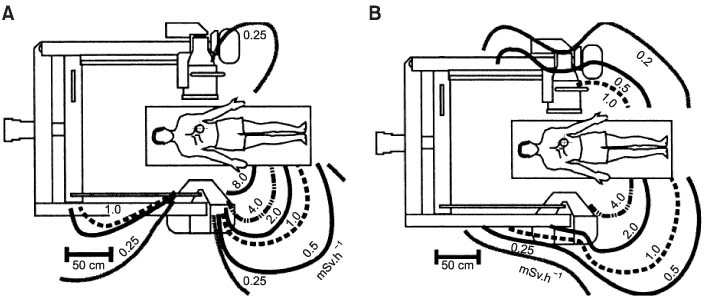
Figure
Cited by 5 articles
-
Radiation Exposure Over the Course of a Year from an Image Intensifier in the Orthopaedic Operating Room
Gu-Hee Jung, Jae-Ho Jang, Jae-Do Kim, Chung-Kyu Kim
J Korean Fract Soc. 2012;25(1):58-63. doi: 10.12671/jkfs.2012.25.1.58.Radiation Exposure Over the Course of a Year from an Image Intensifier in the Orthopaedic Operating Room
Gu-Hee Jung, Jae-Ho Jang, Jae-Do Kim, Chung-Kyu Kim
J Korean Fract Soc. 2012;25(1):58-63. doi: 10.12671/jkfs.2012.25.1.58.Surgical Treatment of Clavicle Midshaft Fractures Using a Locking Compression Plate: Conventional Open Reduction and Plating with Internal Fixation versus Minimal Invasive Plate Osteosynthesis
Jin-Young Bang, Byung Ook Park, Yong Min Seo, Dae Wook Kim, Dong-Hyun Lee, Youngbok Kim, Young Chang Kim, Ji Wan Kim
J Korean Orthop Assoc. 2017;52(6):529-536. doi: 10.4055/jkoa.2017.52.6.529.Factors Affecting Radiation Protection Behaviors among Operating Room Nurses
Jin Kim, Jin Sun Kim, Hyunlye Kim
Korean J Adult Nurs. 2016;28(6):680-690. doi: 10.7475/kjan.2016.28.6.680.Basosquamous Carcinoma of the Hand in a Radiologist with Prolonged Radiation Exposure
Jong Chan Kim, Sung Gyun Jung, Kyung Ho Kim, Hong Lim Kim
J Korean Soc Surg Hand. 2016;21(3):162-166. doi: 10.12790/jkssh.2016.21.3.162.
Reference
-
1. Oh CW, Kim JJ, Byun YS, et al. Minimally invasive plate osteosynthesis of subtrochanteric femur fractures with a locking plate: a prospective series of 20 fractures. Arch Orthop Trauma Surg. 2009. 129:1659–1665.
Article2. Apivatthakakul T, Chiewcharntanakit S. Minimally invasive plate osteosynthesis (MIPO) in the treatment of the femoral shaft fracture where intramedullary nailing is not indicated. Int Orthop. 2008. 33:1119–1126.
Article3. Zhiquan A, Bingfang Z, Yeming W, Chi Z, Peiyan H. Minimally invasive plating osteosynthesis (MIPO) of middle and distal third humeral shaft fractures. J Orthop Trauma. 2007. 21:628–633.
Article4. Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury. 2007. 38:365–370.
Article5. Hazarika S, Chakravarthy J, Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia--results in 20 patients. Injury. 2006. 37:877–887.
Article6. Perren SM. The technology of minimally invasive percutaneous osteosynthesis (MIPO). Injury. 2002. 33:Suppl 1. VI–VII.7. Krettek C, Muller M, Miclau T. Evolution of minimally invasive plate osteosynthesis (MIPO) in the femur. Injury. 2001. 32:Suppl 3. SC14–SC23.
Article8. Maxon HR, Thomas SR, Saenger EL, Buncher CR, Kereiakes JG. Ionizing irradiation and the induction of clinically significant disease in the human thyroid gland. Am J Med. 1977. 63:967–978.
Article9. Merriam GR Jr., Focht EF. A clinical study of radiation cataracts and the relationship to dose. Am J Roentgenol Radium Ther Nucl Med. 1957. 77:759–785.10. 1990 Recommendations of the International Commission on Radiological Protection. Ann ICRP. 1991. 21:1–201.11. Ron E. Cancer risks from medical radiation. Health Phys. 2003. 85:47–59.
Article12. Bross ID, Ball M, Falen S. A dosage response curve for the one rad range: adult risks from diagnostic radiation. Am J Public Health. 1979. 69:130–136.
Article13. Korea Food and Drug Administration. 2007 Report occupational radiation exposure in diagnostic radiology in korea. 2008. Seoul: Food and Drug Administration.14. Kempf I, Grosse A, Beck G. Closed locked intramedullary nailing. Its application to comminuted fractures of the femur. J Bone Joint Surg Am. 1985. 67:709–720.
Article15. Levin PE, Schoen RW Jr, Browner BD. Radiation exposure to the surgeon during closed interlocking intramedullary nailing. J Bone Joint Surg Am. 1987. 69:761–766.
Article16. Müller LP, Suffner J, Wenda K, Mohr W, Rommens PM. Radiation exposure to the hands and the thyroid of the surgeon during intramedullary nailing. Injury. 1998. 29:461–468.
Article17. Madan S, Blakeway C. Radiation exposure to surgeon and patient in intramedullary nailing of the lower limb. Injury. 2002. 33:723–727.
Article18. Devalia KL, Peter VK, Madanur MA, Braithwaite IJ. Exposure of the thyroid to radiation during routine orthopaedic procedures. Acta Orthop Belg. 2006. 72:615–620.19. Barry TP. Radiation exposure to an orthopedic surgeon. Clin Orthop Relat Res. 1984. (182):160–164.
Article20. Goldstone KE, Wright IH, Cohen B. Radiation exposure to the hands of orthopaedic surgeons during procedures under fluoroscopic X-ray control. Br J Radiol. 1993. 66:899–901.
Article21. Fuchs M, Schmid A, Eiteljörge T, Modler M, Sturmer KM. Exposure of the surgeon to radiation during surgery. Int Orthop. 1998. 22:153–156.
Article22. Dosch JC, Dupuis M, Beck G. [Radiation measurements during interlocking nailing]. Hefte Unfallheilkd. 1983. 161:36–38.23. Mehlman CT, DiPasquale TG. Radiation exposure to the orthopaedic surgical team during fluoroscopy: "how far away is far enough?". J Orthop Trauma. 1997. 11:392–398.
Article24. Tremains MR, Georgiadis GM, Dennis MJ. Radiation exposure with use of the inverted-c-arm technique in upper-extremity surgery. J Bone Joint Surg Am. 2001. 83-A:674–678.
Article25. Balter S. Stray radiation in the cardiac catheterisation laboratory. Radiat Prot Dosimetry. 2001. 94:183–188.
Article26. Jackson G, Brennan PC. Radio-protective aprons during radiological examinations of the thorax: An optimum strategy. Radiation Protection Dosimetry. 2006. 121:391–394.
Article27. Blattert TR, Fill UA, Kunz E, Panzer W, Weckbach A, Regulla DF. Skill dependence of radiation exposure for the orthopaedic surgeon during interlocking nailing of long-bone shaft fractures: a clinical study. Arch Orthop Trauma Surg. 2004. 124:659–664.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiation Exposure Over the Course of a Year from an Image Intensifier in the Orthopaedic Operating Room
- Radiation Induced Hand Necrosis of an Orthopaedic Surgeon Who Had Treated a Patient with Fluoroscopy-Guided Spine Injection
- Radiation Exposure from a Patient Treated with I-131 during Emergency Operation: A case report
- Current status of medical radiation exposure and regulation efforts
- Fluoroscopic Radiation Exposure during Percutaneous Kyphoplasty