J Korean Med Assoc.
2007 Dec;50(12):1109-1118. 10.5124/jkma.2007.50.12.1109.
Update of Moyamoya Disease
- Affiliations
-
- 1Division of Pediatric Neurosurgery, Seoul National University College of Medicine, Korea. nsthomas@snu.ac.kr
- KMID: 2184959
- DOI: http://doi.org/10.5124/jkma.2007.50.12.1109
Abstract
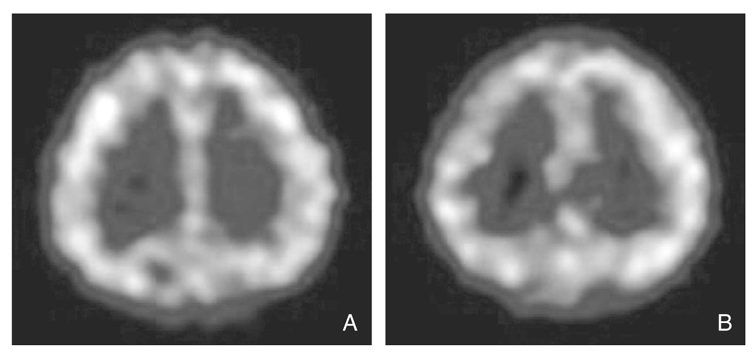
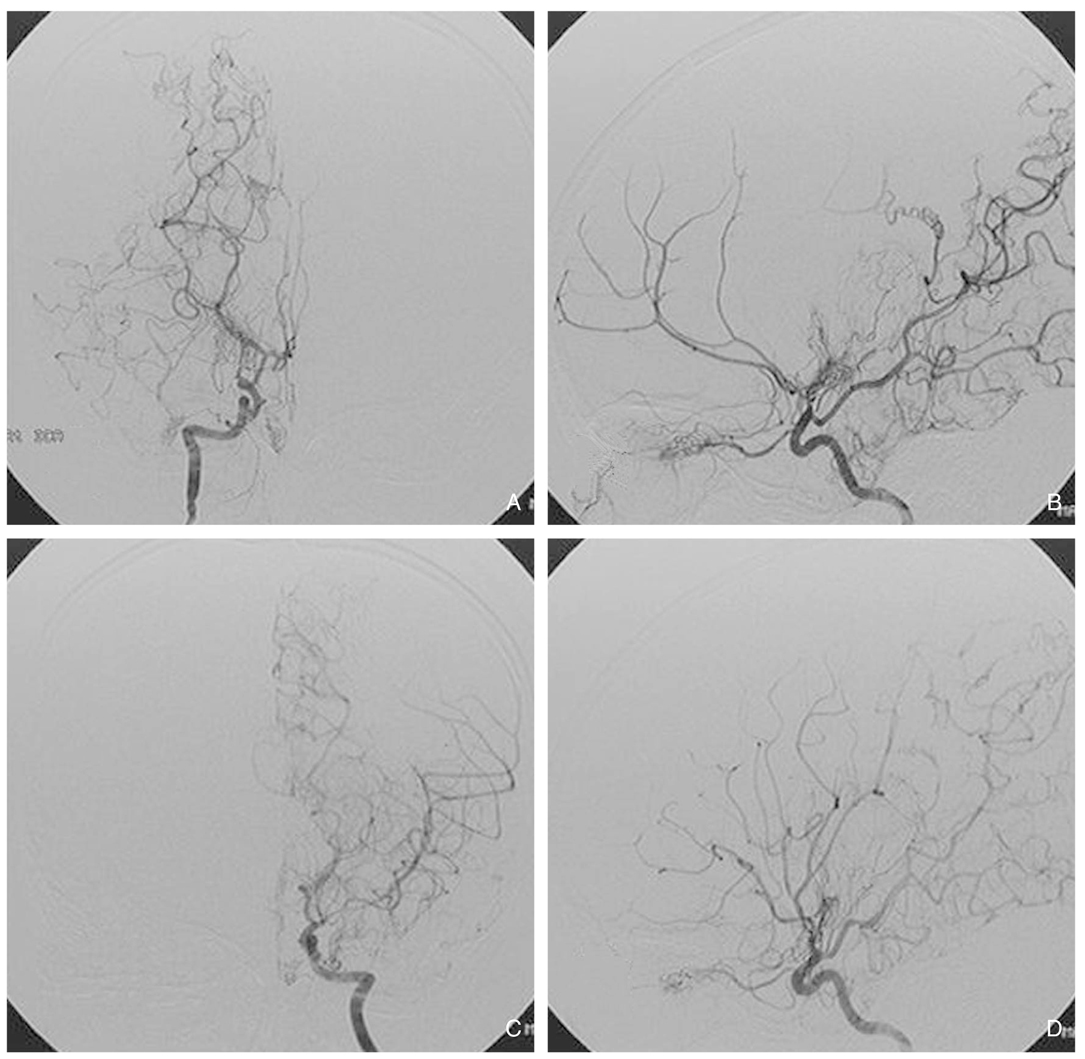
- Moyamoya disease is characterized by bilateral stenosis or occlusion of distal internal carotid artery (ICA) bifurcation including its proximal branches and abnormal vascular network (moyamoya vessel, MMV) in the vicinity of the arterial occlusions. It is the most common pediatric cerebrovascular disease in Eastern Asia, particularly in Korea and Japan. The etiology is still unknown, but much about the pathology from autopsies, factors involved in its pathogenesis, and its genetics have been studied and reported. It may cause ischemic attacks or cerebral infarctions in children and cerebral hemorrhage in adults. Because of its aggressive clinical course in very young children, the need for early detection and treatment has been recognized. Magnetic resonance imaging (MRI)/MR angiography (MRA), cerebral hemodynamic studies, and cerebral angiography are used for the diagnosis. The treatment basically focuses on prevention of further ischemia and infarction through revascularization. Technically, direct and indirect bypass methods are used. The treatment strategy needs to be individualized in each patient. Outcomes of revascularization procedures are excellent in preventing transient ischemic attacks (TIAs) in most patients.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Acute Ischemic Stroke in Moyamoya Syndrome Associated with Thyrotoxicosis
Donggook Kang, Gi-Hun Seong, Jong Seok Bae, Ju-Hun Lee, Hong-Ki Song, Yerim Kim
J Neurocrit Care. 2018;11(2):129-133. doi: 10.18700/jnc.180046.
Reference
-
1. Suzuki J, Takaku A. Cerebrovascular "moyamoya" disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969. 20:288–299.2. Natori Y, Ikezaki K, Matsushima T, Fukui M. 'Angiographic moyamoya' its definition, classification, and therapy. Clin Neurol Neurosurg. 1997. 99:S2. S168–S172.
Article3. Ikezaki K, Han DH, Kawano T, Kinukawa N, Fukui M. A clinical comparison of definite moyamoya disease between South Korea and Japan. Stroke. 1997. 28:2513–2517.
Article4. Suzuki J, Kodama N. Moyamoya disease-a review. Stroke. 1983. 14:104–109.
Article5. Nakashima H, Meguro T, Kawada S, Hirotsune N, Ohmoto T. Long-term results of surgically treated moyamoya disease. Clin Neurol Neurosurg. 1997. 99:S2. S156–S161.
Article6. Ikezaki K. Ikezaki K, Loftus C, editors. Clinical manifestations: epidemiology, symptoms and signs, laboratory findings. Moyamoya Disease. 2001. Rolling Meadows: American Association of Neurological Surgeons;43–54.7. Wakai K, Tamakoshi A, Ikezaki K, Fukui M, Kawamura T, Aoki R, Kojima M, Lin Y, Ohno Y. Epidemiological features of moyamoya disease in Japan: findings from a nationwide survey. Clin Neurol Neurosurg. 1997. 99:S2. S1–S5.
Article8. Kim SK, Wang KC, Kim DG, Paek SH, Chung HT, Han MH, Ahn Y, Cho BK. Clinical feature and outcome of pediatric cerebrovascular disease: a neurosurgical series. Childs Nerv Syst. 2000. 16:421–428.
Article9. Fukui M, Kono S, Sueishi K, Ikezaki K. Moyamoya disease. Neuropathology. 2000. 20:S2. S61–S64.
Article10. Malek AM, Connors S, Robertson RL, Folkman J, Scott RM. Elevation of cerebrospinal fluid levels of basic fibroblast growth factor in moyamoya and central nervous system disorders. Pediatr Neurosurg. 1997. 27:182–189.
Article11. Hojo M, Hoshimaru M, Miyamoto S, Taki W, Nagata I, Asahi M, Matsuura N, Ishizaki R, Kikuchi H, Hashimoto N. Role of transforming growth factor-beta1 in the pathogenesis of moyamoya disease. J Neurosurg. 1998. 89:623–629.
Article12. Kim SK, Yoo JI, Cho BK, Hong SJ, Kim YK, Moon JA, Kim JH, Chung YN, Wang KC. Elevation of CRABP-I in the cerebrospinal fluid of patients with Moyamoya disease. Stroke. 2003. 34:2835–2841.
Article13. Yamada H, Deguchi K, Tanigawara T, Takenaka K, Nishimura Y, Shinoda J, Hattori T, Andoh T, Sakai N. The relationship between moyamoya disease and bacterial infection. Clin Neurol Neurosurg. 1997. 99:S2. S221–S224.
Article14. Ikezaki K, Kono S, Fukui M. Ikezaki K, Loftus C, editors. Etiology of moyamoya disease: pathology, pathophysiology, and genetics. Moyamoya Disease. 2001. Rolling Meadows: American Association of Neurological Surgeons;55–64.15. Kang HS, Kim SK, Cho BK, Kim YY, Hwang YS, Wang KC. Single nucleotide polymorphisms of tissue inhibitor of metalloproteinase genes in familial moyamoya disease. Neurosurgery. 2006. 58:1074–1080.
Article16. Kim SK, Seol HJ, Cho BK, Hwang YS, Lee DS, Wang KC. Moyamoya disease among young patients: its aggressive clinical course and the role of active surgical treatment. Neurosurgery. 2004. 54:840–844. discussion 4-6.
Article17. Ogawa A, Nakamura N, Yoshimoto T, Suzuki J. Cerebral blood flow in moyamoya disease. Part 2: Autoregulation and CO2 response. Acta Neurochir (Wien). 1990. 105:107–111.
Article18. Seol HJ, Wang KC, Kim SK, Hwang YS, Kim KJ, Cho BK. Headache in pediatric moyamoya disease: review of 204 consecutive cases. J Neurosurg. 2005. 103:439–442.
Article19. Ikezaki K, Fukui M, Inamura T, Kinukawa N, Wakai K, Ono Y. The current status of the treatment for hemorrhagic type moyamoya disease based on a 1995 nationwide survey in Japan. Clin Neurol Neurosurg. 1997. 99:S2. S183–S186.
Article20. Saeki N, Nakazaki S, Kubota M, Yamaura A, Hoshi S, Sunada S, Sunami K. Hemorrhagic type moyamoya disease. Clin Neurol Neurosurg. 1997. 99:S2. S196–S201.
Article21. Iwama T, Morimoto M, Hashimoto N, Goto Y, Todaka T, Sawada M. Mechanism of intracranial rebleeding in moyamoya disease. Clin Neurol Neurosurg. 1997. 99:S2. S187–S190.
Article22. Houkin K, Yoshimoto T, Kuroda S, Ishikawa T, Takahashi A, Abe H. Angiographic analysis of moyamoya disease-how does moyamoya disease progress? Neurol Med Chir (Tokyo). 1996. 36:783–787. discussion 8.23. Kuroda S, Kamiyama H, Isobe M, Houkin K, Abe H, Mitsumori K. Cerebral hemodynamics and "re-build-up" phenomenon on electroencephalogram in children with moyamoya disease. Childs Nerv Syst. 1995. 11:214–219.
Article24. Ikezaki K, Matsushima T, Kuwabara Y, Suzuki SO, Nomura T, Fukui M. Cerebral circulation and oxygen metabolism in childhood moyamoya disease: a perioperative positron emission tomography study. J Neurosurg. 1994. 81:843–850.
Article25. Kim SK, Wang KC, Oh CW, Kim IO, Lee DS, Song IC, Cho BK. Evaluation of cerebral hemodynamics with perfusion MRI in childhood moyamoya disease. Pediatr Neurosurg. 2003. 38:68–75.
Article26. Kuwabara Y, Ichiya Y, Sasaki M, Yoshida T, Masuda K, Matsushima T, Fukui M. Response to hypercapnia in moyamoya disease. Cerebrovascular response to hypercapnia in pediatric and adult patients with moyamoya disease. Stroke. 1997. 28:701–707.27. Seol HJ, Wang KC, Kim SK, Lee CS, Lee DS, Kim IO, Cho BK. Unilateral (probable) moyamoya disease: long-term follow-up of seven cases. Childs Nerv Syst. 2006. 22:145–150.
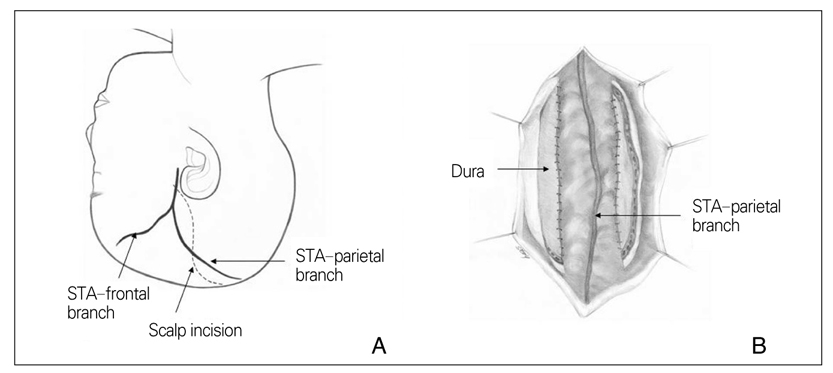
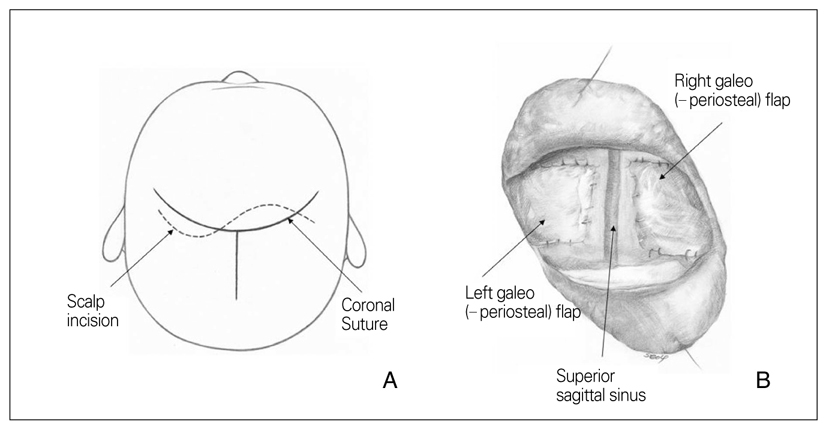
Article28. Okada Y, Shima T, Matsumura S, Nishida M, Yamada T, Okita S. [Pathophysiological studies in moyamoya disease by rCBF and cortical artery pressure measurements in comparison to those in ICA or MCA occlusion]. No To Shinkei. 1988. 40:899–903.29. Matsushima Y, Inaba Y. Moyamoya disease in children and its surgical treatment. Introduction of a new surgical procedure and its follow-up angiograms. Childs Brain. 1984. 11:155–170.30. Kim SK, Wang KC, Kim IO, Lee DS, Cho BK. Combined encephaloduroarteriosynangiosis and bifrontal encephalogaleo (periosteal)synangiosis in pediatric moyamoya disease. Neurosurgery. 2002. 50:88–96.
Article31. Kim CY, Wang KC, Kim SK, Chung YN, Kim HS, Cho BK. Encephaloduroarteriosynangiosis with bifrontal encephalogaleo (periosteal) synangiosis in the pediatric moyamoya disease: the surgical technique and its outcomes. Childs Nerv Syst. 2003. 19:316–324.
Article32. Chung YN, Wang KC, Cho BK. Kim DG, editor. Moyamoya disease, Encephaloduroarteriosynangiosis. Practical Points in Neurosurgery. 2007. Seoul: Ilchokak;385–389.33. Kim SK, Wang KC, Cho BK. Kim DG, editor. Moyamoya disease, Bifrontal Encephalogaleo (periosteal) synangiosis. Practical Points in Neurosurgery. 2007. Seoul: Ilchokak;390–394.34. Choi IJ, Hong SH, Cho BK, Wang KC, Kim SK. Encephalo-duro-arterio-synangiosis (EDAS) using occipital artery in children with moyamoya disease. J Korean Neurosurg Soc. 2005. 38:413–418.35. Sainte-Rose C, Oliveira R, Puget S, Beni-Adani L, Boddaert N, Thorne J, Wray A, Zerah M, Bourgeois M. Multiple bur hole surgery for the treatment of moyamoya disease in children. J Neurosurg. 2006. 105:437–443.
Article36. Karasawa J, Touho H, Ohnishi H, Miyamoto S, Kikuchi H. Long-term follow-up study after extracranial-intracranial bypass surgery for anterior circulation ischemia in childhood moyamoya disease. J Neurosurg. 1992. 77:84–89.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The News on Moyamoya Disease: Review Article
- A Recent Update of Clinical and Research Topics Concerning Adult Moyamoya Disease
- Neuroimaging Diagnosis and Treatment of Moyamoya Disease
- Moyamoya-like Disease Associated with Intracranial Aneurysm
- Familial Occurrence of Moyamoya Disease in a Father and a Son