J Clin Neurol.
2014 Jul;10(3):267-271. 10.3988/jcn.2014.10.3.267.
Role of High-Resolution Magnetic Resonance Imaging in the Diagnosis of Primary Angiitis of the Central Nervous System
- Affiliations
-
- 1Department of Neurology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. nmboy@unitel.co.kr
- 2Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Clinical Research Center, Samsung Biomedical Research Institute, Seoul, Korea.
- KMID: 2179456
- DOI: http://doi.org/10.3988/jcn.2014.10.3.267
Abstract
- BACKGROUND
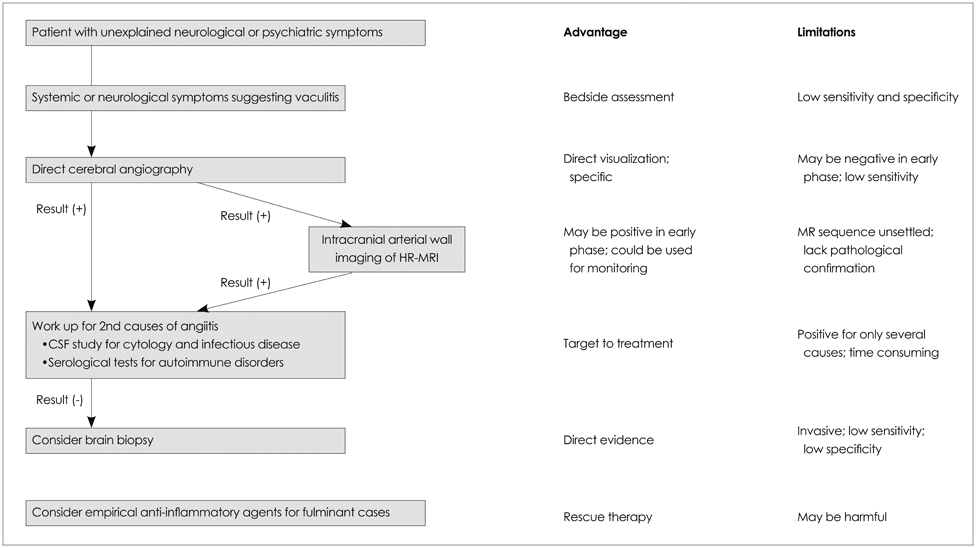
Primary angiitis of the central nervous system (PACNS) is a rare disorder and is often difficult to diagnose due to the lack of a confirmatory test. PACNS can generally be diagnosed based on typical angiographic findings. We describe herein a patient diagnosed with PACNS despite the presence of normal findings on conventional angiography.
CASE REPORT
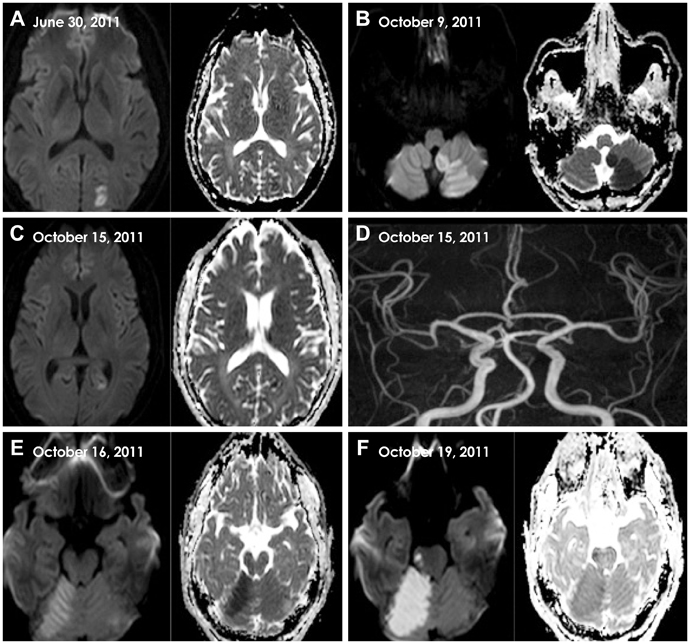
A 44-year-old man with a recent history of ischemic stroke in the right posterior cerebral artery territory developed acute-onset vertigo. Diffusion-weighted imaging revealed an acute infarction within the left posterior inferior cerebellar artery. His medical history was unremarkable except for hyperlipidemia; the initial examination revealed mild gait imbalance. During the 10 days of hospital admission, the patient experienced four recurrent ischemic strokes within the posterior circulation territory (occipital lobe, pons, and cerebellum). He was diagnosed with recurrent cerebral infarctions due to PACNS. The basilar artery exhibited no demonstrable luminal stenosis, but there were direct imaging signs of central nervous system angiitis including wall thickening and contrast enhancement. High-dose intravenous steroid therapy followed by oral prednisolone was administered. There was no further stroke recurrence and follow-up imaging of the arterial walls showed normalization of their characteristics.
CONCLUSIONS
The present case emphasizes the importance of wall imaging in the diagnosis and treatment of PACNS.
MeSH Terms
-
Adult
Angiography
Arteries
Basilar Artery
Central Nervous System*
Cerebral Infarction
Constriction, Pathologic
Diagnosis*
Follow-Up Studies
Gait
Humans
Hyperlipidemias
Infarction
Inflammation
Magnetic Resonance Imaging*
Phenobarbital
Pons
Posterior Cerebral Artery
Prednisolone
Recurrence
Stroke
Vasculitis*
Vasculitis, Central Nervous System
Vertigo
Phenobarbital
Prednisolone
Figure
Reference
-
1. Salvarani C, Brown RD Jr, Calamia KT, Christianson TJ, Weigand SD, Miller DV, et al. Primary central nervous system vasculitis: analysis of 101 patients. Ann Neurol. 2007; 62:442–451.
Article2. Hajj-Ali RA, Singhal AB, Benseler S, Molloy E, Calabrese LH. Primary angiitis of the CNS. Lancet Neurol. 2011; 10:561–572.
Article3. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article4. Küker W. Cerebral vasculitis: imaging signs revisited. Neuroradiology. 2007; 49:471–479.
Article5. Molloy ES, Langford CA. Vasculitis mimics. Curr Opin Rheumatol. 2008; 20:29–34.
Article6. Scolding NJ. Central nervous system vasculitis. Semin Immunopathol. 2009; 31:527–536.
Article7. Calabrese LH, Mallek JA. Primary angiitis of the central nervous system. Report of 8 new cases, review of the literature, and proposal for diagnostic criteria. Medicine (Baltimore). 1988; 67:20–39.8. Cupps TR, Moore PM, Fauci AS. Isolated angiitis of the central nervous system. Prospective diagnostic and therapeutic experience. Am J Med. 1983; 74:97–105.9. Alhalabi M, Moore PM. Serial angiography in isolated angiitis of the central nervous system. Neurology. 1994; 44:1221–1226.
Article10. Küker W, Gaertner S, Nagele T, Dopfer C, Schoning M, Fiehler J, et al. Vessel wall contrast enhancement: a diagnostic sign of cerebral vasculitis. Cerebrovasc Dis. 2008; 26:23–29.
Article11. Kissin EY, Merkel PA. Diagnostic imaging in Takayasu arteritis. Curr Opin Rheumatol. 2004; 16:31–37.
Article12. Swartz RH, Bhuta SS, Farb RI, Agid R, Willinsky RA, Terbrugge KG, et al. Intracranial arterial wall imaging using high-resolution 3-tesla contrast-enhanced MRI. Neurology. 2009; 72:627–634.
Article13. Saam T, Habs M, Pollatos O, Cyran C, Pfefferkorn T, Dichgans M, et al. High-resolution black-blood contrast-enhanced T1 weighted images for the diagnosis and follow-up of intracranial arteritis. Br J Radiol. 2010; 83:e182–e184.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Childhood Primary Angiitis of the Central Nervous System Presenting as Isolated Middle Cerebral Artery Dissection
- Primary Angiitis of the Central Nervous System Presenting Tumefactive Lesions and Small Arteriolar Ectasias
- The Value of High-Resolution Vessel Wall Magnetic Resonance Imaging in the Diagnosis and Management of Primary Angiitis of the Central Nervous System in Children
- Primary Angiitis of the Central Nervous System Diagnosed by High-Resolution Vessel Wall MRI
- A Case of Primary Angiitis of the Central Nervous System: A Case Presentation