J Korean Diabetes Assoc.
2007 Nov;31(6):520-524. 10.4093/jkda.2007.31.6.520.
A Case of Cured Diabetes Mellitus after Occult Malignant Pheochromocytoma Removal
- Affiliations
-
- 1Department of Internal Medicine, Keimyung University School of Medicine.
- 2Department of Surgery, Keimyung University School of Medicine.
- 3Department of Pathology, Keimyung University School of Medicine.
- KMID: 2177566
- DOI: http://doi.org/10.4093/jkda.2007.31.6.520
Abstract
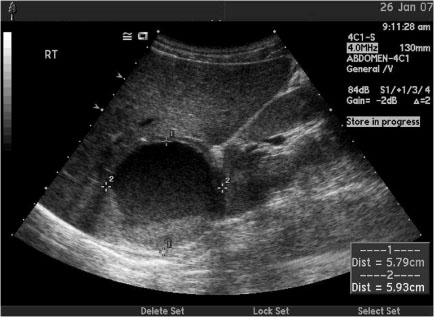
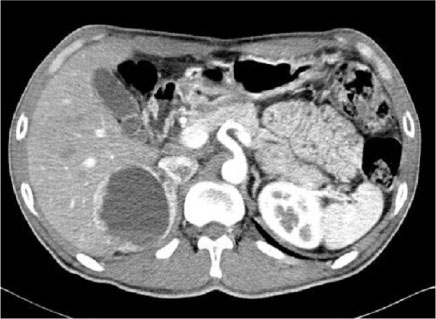
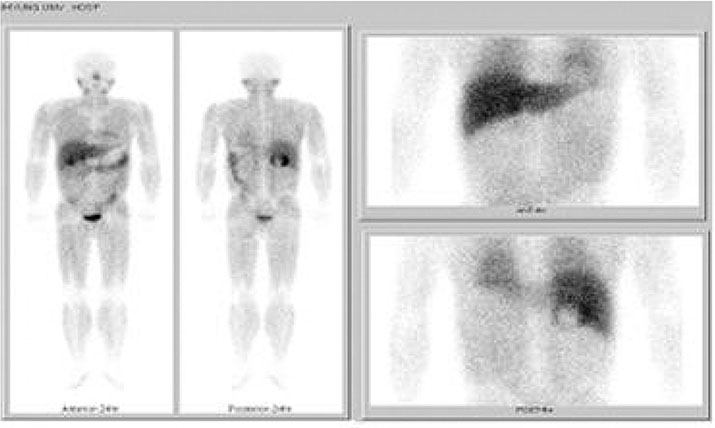
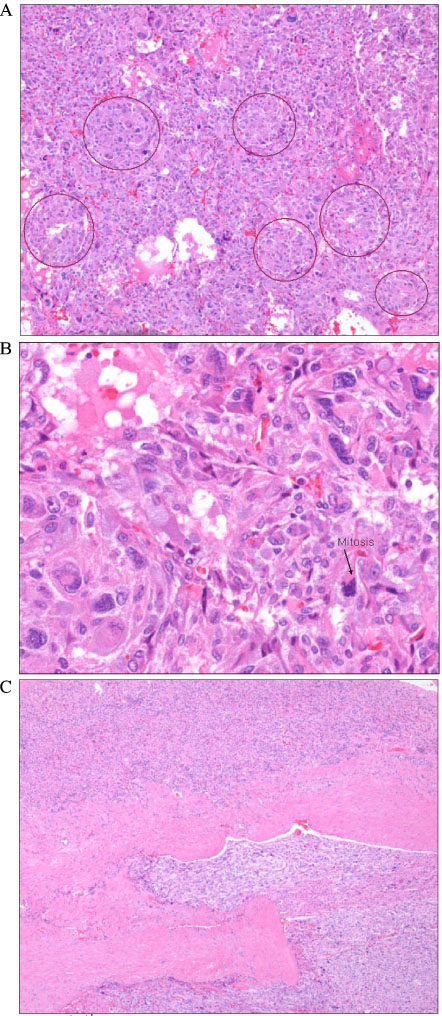
- Pheochromocytoma is characterized by a combination of various clinical manifestations that include the classic triad of severe headache, palpitations and diaphoresis. In addition, hyperglycemia can be caused by overproduction of catecholamines, which are secreted by a catecholamine-secreting neoplasm of adrenal or extra-adrenal chromaffin tissue. We encountered a case of diabetes with an occult malignant adrenal pheochromocytoma, who did not have any classic manifestations. A 37-year-old male was admitted because of polydipsia, polyuria, and weight loss. Fasting blood glucose level was 497 mg/dL, hemoglobin A1c level was 15%, and diabetic retinopathy and peripheral polyneuropathy were also accompanied. Incidentally, right adrenal mass was detected by ultrasonography of abdomen. Urinary excretion of total metanephrine and epinephrine were elevated. Adrenal CT showed a 7.1 cm sized right adrenal cystic mass with enhancing solid portion and hemorrhagic content. The scan with 123I-MIBG revealed the cystic mass with increased rim uptake in the region of right adrenal gland. After removal of the tumor, the increased levels of catecholamine were normalized. Moreover, blood glucose level was normalized without administration of insulin or oral hypoglycemic agents. The pathologic examination showed that the neoplasm was a malignant adrenal pheochromocytoma. We report this case that diabetes was cured after removal of malignant tumor with literature review at first in Korea.
MeSH Terms
-
Abdomen
Adrenal Glands
Adult
Blood Glucose
Catecholamines
Diabetes Mellitus*
Diabetic Retinopathy
Epinephrine
Fasting
Headache
Humans
Hyperglycemia
Hypoglycemic Agents
Insulin
Korea
Male
Metanephrine
Pheochromocytoma*
Polydipsia
Polyneuropathies
Polyuria
Ultrasonography
Weight Loss
Blood Glucose
Catecholamines
Epinephrine
Hypoglycemic Agents
Insulin
Metanephrine
Figure
Reference
-
1. Bravo EL. Pheochromocytoma: New concepts and future trends. Kidney Int. 1991. 40:544–556.2. Reisch N, Peczkowska M, Januszewicz A, Neumann HP. Pheochromocytoma: presentation, diagnosis and treatment. J Hypertens. 2006. 24:2331–2339.4. La Batide-Alanore A, Chatellier G, Plouin PF. Diabetes as a marker of pheochromocytoma in hypertensive patients. J Hypertens. 2003. 21:1703–1707.8. Yamashita S, Dohi Y, Kinoshita M, Kojima M, Mivagawa K, Sato K. Occult extraadrenal pheochromocytoma treated as diabetes mellitus. Am J Med Sci. 1997. 314:276–278.9. Saito T, Satoh S, Kawasaki S, Mukasa K, Itoh S, Yamakawa T, Sekihara H. Three patients with adrenal tumors having been treated simply for diabetes mellitus. Biomed Pharmacother. 2000. 54:Suppl 1. 198s–202s.10. Rizza RA, Cryer PE, Haymond MW, Gerich JE. Adrenergic mechanisms of catecholamine action on glucose homeostasis in man. Metabolism. 1980. 29:1155–1163.11. Turnbull DM, Johnston DG, Alberti KG, Hall R. Hormonal and metabolic studies in a patient with a pheochromocytoma. J Clin Endocrinol Metab. 1980. 51:930–933.12. Saccà L, Morrone G, Cicala M, Corso G, Ungaro B. Influence of epinephrine, norepinephrine, and isoproterenol on glucose homeostasis in normal man. J Clin Endocrinol Metab. 1980. 50:680–684.14. Wiesner TD, Bluher M, Windgassen M, Paschke R. Improvement of insulin sensitivity after adrenalectomy in patients with pheochromocytoma. J Clin Endocrinol Metab. 2003. 88:3632–3636.15. Emmer M, Gorden P, Roth J. Diabetes in association with other endocrine disorders. Symposium on diabetes. Med Clin North Am. 1971. 55:1057–1064.16. Stenström G, Sjöström L, Smith U. Diabetes mellitus in phaeochromocytoma. Fasting blood glucose levels before and after surgery in 60 patients with phaeochromocytoma. Acta Endocrinol (Copenh). 1984. 106:511–515.17. Spergel G, Bleicher SJ, Ertel NH. Carbohydrate and fat metabolism in patients with pheochromocytoma. N Engl J Med. 1968. 278:803–809.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Malignant Pheochromocytoma
- A Case of Cured Diabetes Mellitus after Pheochromocytoma Removal
- A Case of Improved Diabetes Mellitus After Removal of Nonfunctioning Adrenal Incidentaloma Diagnosed as Pheochromocytoma
- Pheochromocytoma associated with cyanotic congenital heart disease
- Clinical evaluation of 12 cases of pheochromocytoma