J Adv Prosthodont.
2013 Nov;5(4):452-456. 10.4047/jap.2013.5.4.452.
White light scanner-based repeatability of 3-dimensional digitizing of silicon rubber abutment teeth impressions
- Affiliations
-
- 1Department of Dental Laboratory Science and Engineering, College of Health Science, Korea University, Seoul, Republic of Korea. kuc2842@korea.ac.kr
- 2Department of Public Health Sciences, Graduate School, Korea University, Seoul, Republic of Korea.
- 3BK21+ Program in Public Health Sciences, Korea University, Seoul, Republic of Korea.
- KMID: 2176538
- DOI: http://doi.org/10.4047/jap.2013.5.4.452
Abstract
- PURPOSE
The aim of this study was to evaluate the repeatability of the digitizing of silicon rubber impressions of abutment teeth by using a white light scanner and compare differences in repeatability between different abutment teeth types.
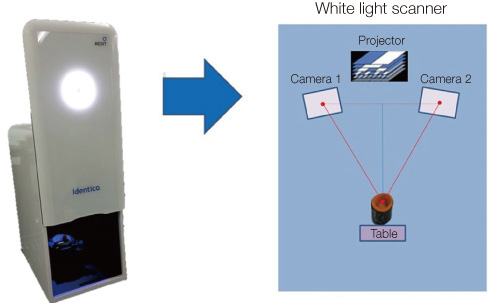
MATERIALS AND METHODS
Silicon rubber impressions of a canine, premolar, and molar tooth were each digitized 8 times using a white light scanner, and 3D surface models were created using the point clouds. The size of any discrepancy between each model and the corresponding reference tooth were measured, and the distribution of these values was analyzed by an inspection software (PowerInspect 2012, Delcamplc., Birmingham, UK). Absolute values of discrepancies were analyzed by the Kruskal-Wallis test and multiple comparisons (alpha=.05).
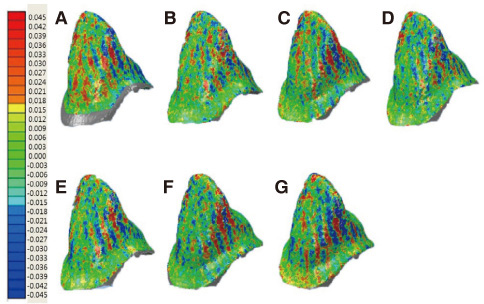
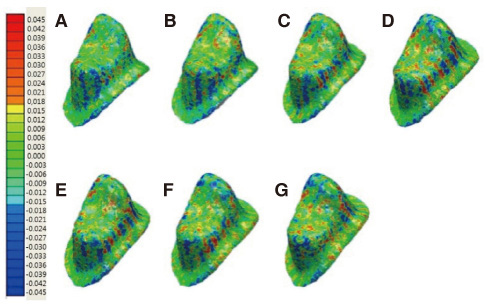
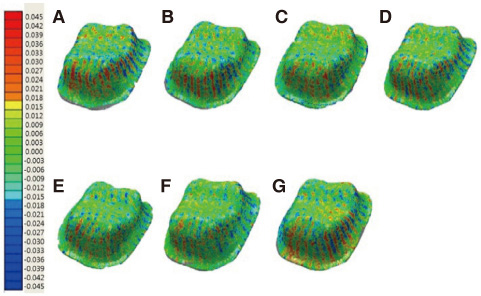
RESULTS
The discrepancy between the impressions for the canine, premolar, and molar teeth were 6.3 microm (95% confidence interval [CI], 5.4-7.2), 6.4 microm (95% CI, 5.3-7.6), and 8.9 microm (95% CI, 8.2-9.5), respectively. The discrepancy of the molar tooth impression was significantly higher than that of other tooth types. The largest variation (as mean [SD]) in discrepancies was seen in the premolar tooth impression scans: 26.7 microm (95% CI, 19.7-33.8); followed by canine and molar teeth impressions, 16.3 microm (95% CI, 15.3-17.3), and 14.0 microm (95% CI, 12.3-15.7), respectively.
CONCLUSION
The repeatability of the digitizing abutment teeth's silicon rubber impressions by using a white light scanner was improved compared to that with a laser scanner, showing only a low mean discrepancy between 6.3 microm and 8.9 microm, which was in an clinically acceptable range. Premolar impression with a long and narrow shape showed a significantly larger discrepancy than canine and molar impressions. Further work is needed to increase the digitizing performance of the white light scanner for deep and slender impressions.
Figure
Cited by 2 articles
-
Trueness and precision of scanning abutment impressions and stone models according to dental CAD/CAM evaluation standards
Jin-Hun Jeon, Seong-Sig Hwang, Ji-Hwan Kim, Woong-Chul Kim
J Adv Prosthodont. 2018;10(5):335-339. doi: 10.4047/jap.2018.10.5.335.Evaluation of the reproducibility of various abutments using a blue light model scanner
Dong-Yeon Kim, Kyung-Eun Lee, Jin-Hun Jeon, Ji-Hwan Kim, Woong-Chul Kim
J Adv Prosthodont. 2018;10(4):328-334. doi: 10.4047/jap.2018.10.4.328.
Reference
-
1. Persson A, Andersson M, Oden A, Sandborgh-Englund G. A three-dimensional evaluation of a laser scanner and a touch-probe scanner. J Prosthet Dent. 2006; 95:194–200.2. Schaefer O, Kuepper H, Sigusch BW, Thompson GA, Hefti AF, Guentsch A. Three-dimensional fit of lithium disilicate partial crowns in vitro. J Dent. 2013; 41:271–277.3. Schaefer O, Watts DC, Sigusch BW, Kuepper H, Guentsch A. Marginal and internal fit of pressed lithium disilicate partial crowns in vitro: a three-dimensional analysis of accuracy and reproducibility. Dent Mater. 2012; 28:320–326.4. Hewlett ER, Orro ME, Clark GT. Accuracy testing of three-dimensional digitizing systems. Dent Mater. 1992; 8:49–53.5. Luthardt RG, Sandkuhl O, Herold V, Walter MH. Accuracy of mechanical digitizing with a CAD/CAM system for fixed restorations. Int J Prosthodont. 2001; 14:146–151.6. Dahlmo KI, Andersson M, Gellerstedt M, Karlsson S. On a new method to assess the accuracy of a CAD program. Int J Prosthodont. 2001; 14:276–283.7. Kuroda T, Motohashi N, Tominaga R, Iwata K. Three-dimensional dental cast analyzing system using laser scanning. Am J Orthod Dentofacial Orthop. 1996; 110:365–369.8. Persson AS, Odén A, Andersson M, Sandborgh-Englund G. Digitization of simulated clinical dental impressions: virtual three-dimensional analysis of exactness. Dent Mater. 2009; 25:929–936.9. Lee KT, Kim JH, Kim WC, Kim JH. Three-dimensional evaluation on the repeatability and reproducibility of dental scanner-based digital models. J Korean Acad Dent Technol. 2012; 34:213–220.10. Quaas S, Rudolph H, Luthardt RG. Direct mechanical data acquisition of dental impressions for the manufacturing of CAD/CAM restorations. J Dent. 2007; 35:903–908.11. DeLong R, Pintado MR, Ko CC, Hodges JS, Douglas WH. Factors influencing optical 3D scanning of vinyl polysiloxane impression materials. J Prosthodont. 2001; 10:78–85.12. Luthardt RG, Kühmstedt P, Walter MH. A new method for the computer-aided evaluation of three-dimensional changes in gypsum materials. Dent Mater. 2003; 19:19–24.13. Nazzal R. CAD scanners and design software. Inside Dent Tech. 2012; 3:7.14. Blais F. Review of 20 years of range sensor development. J Electron Imaging. 2004; 13:231–240.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Repeatability and reproducibility of individual abutment impression, assessed with a blue light scanner
- Accuracy of 3D white light scanning of abutment teeth impressions: evaluation of trueness and precision
- Evaluation of the effect of abutment preparation angles on the repeatability and reproducibility using a blue light model scanner
- Evaluation of the reproducibility of various abutments using a blue light model scanner
- THE EFFECT OF IMMERSION DISINFECTION ON THE DIMENSIONAL STABILITY OF RUBBER IMPRESSION MATERIALS