Investig Magn Reson Imaging.
2015 Mar;19(1):37-46. 10.13104/imri.2015.19.1.37.
Diagnostic Effectiveness of USPIO versus Gadolinium Based MRI for Axillary Metastasis in Breast Cancer: A Meta-analysis
- Affiliations
-
- 1Department of Surgery, Kosin University Gospel Hospital, Busan, Korea.
- 2Department of Obstetrics and Gynecology, Mirae Woman's Hospital, Busan, Korea.
- 3Department of Radiology, Kosin University Gospel Hospital, Busan, Korea. mammomaster@naver.com
- KMID: 2175575
- DOI: http://doi.org/10.13104/imri.2015.19.1.37
Abstract
- PURPOSE
This report compared the diagnostic effectiveness between ultrasmall superparamagnetic iron oxide (USPIO) and gadolinium (Gd) based magnetic resonance imaging (MRI) for differentiation of axillary status in breast cancer patients.
MATERIALS AND METHODS
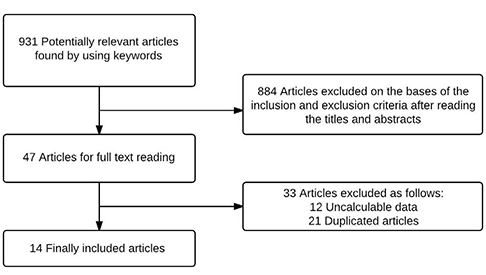
The present authors performed a meta-analysis of previous studies that compared USPIO or Gd based MRI with histological diagnosis after surgery or biopsy. We searched PubMed, EMBASE, Cochrane Library, ScienceDirect, SpringerLink, Ovid databases and references of articles to identify studies reporting data until December 2013. Pooled sensitivity and specificity were calculated for every study; summary receiver operating characteristic and subgroup analysis was done. Analyses of study quality and heterogeneity were also assessed.
RESULTS
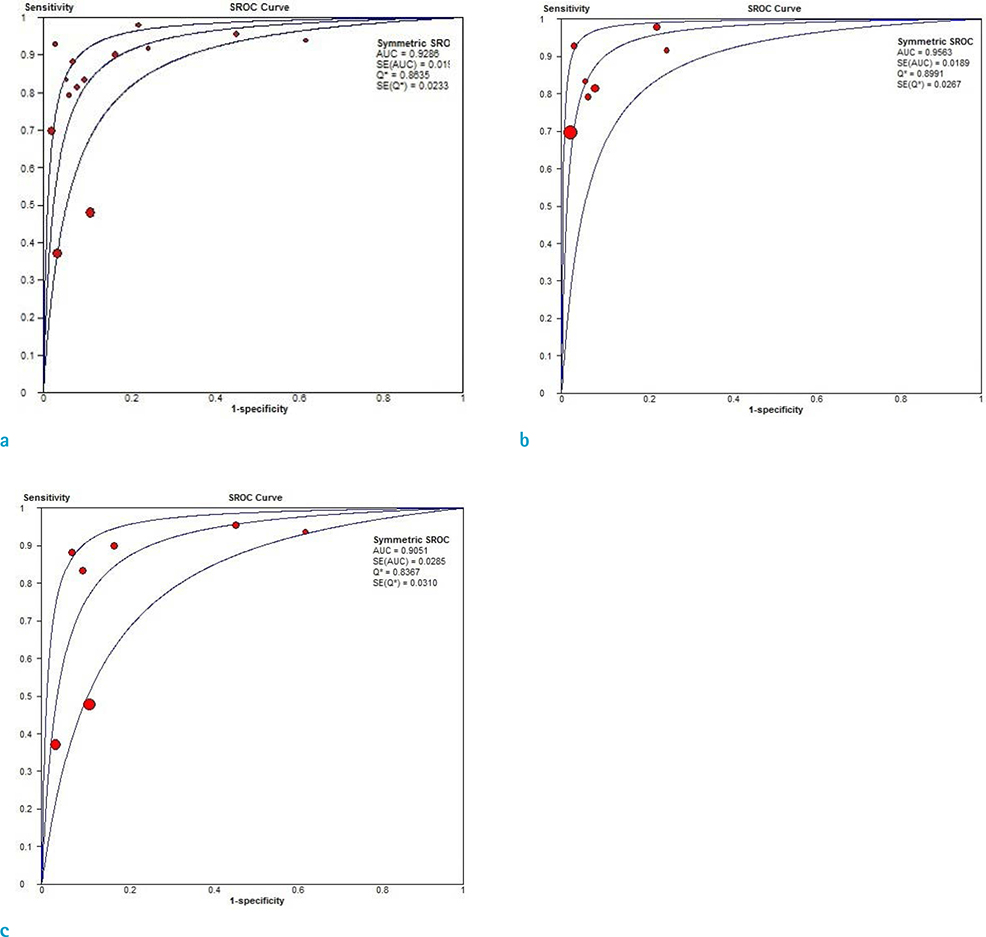
There were 14 publications that met the criteria for inclusion in our metaanalysis. USPIO based MRI showed 0.83 (95% CI: 0.75-0.89) and 0.97 (95% CI: 0.94-0.98) for pooled sensitivity and specificity, respectively. Gd based MRI represented pooled sensitivity and specificity of 0.61 (95% CI: 0.55-0.67) and 0.90 (95% CI: 0.87-0.92) for each. Overall weighted area under the curve for USPIO and Gd based MRI were 0.9563 and 0.9051, respectively.
CONCLUSION
USPIO based MRI had a tendency toward high pooled sensitivity and specificity in detection of axillary metastases for breast cancer. This result may mean that USPIO based MRI could be used as complementary modality to differentiate axillary status more precisely, and assist in the decision-making process regarding possible invasive procedures, such as sentinel node biopsy.
MeSH Terms
Figure
Reference
-
1. Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014; 64:9–29.2. Wiechmann L, Sampson M, Stempel M, et al. Presenting features of breast cancer differ by molecular subtype. Ann Surg Oncol. 2009; 16:2705–2710.3. Wilking N, Rutqvist LE, Carstensen J, Mattsson A, Skoog L. Stockholm Breast Cancer Study Group. Prognostic significance of axillary nodal status in primary breast cancer in relation to the number of resected nodes. Acta Oncol. 1992; 31:29–35.4. Mansel RE, Fallowfield L, Kissin M, et al. Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: the ALMANAC Trial. J Natl Cancer Inst. 2006; 98:599–609.5. Purushotham AD, Upponi S, Klevesath MB, et al. Morbidity after sentinel lymph node biopsy in primary breast cancer: results from a randomized controlled trial. J Clin Oncol. 2005; 23:4312–4321.6. Robertson IJ, Hand F, Kell MR. FDG-PET/CT in the staging of local/regional metastases in breast cancer. Breast. 2011; 20:491–494.7. Taylor K, O'Keeffe S, Britton PD, et al. Ultrasound elastography as an adjuvant to conventional ultrasound in the preoperative assessment of axillary lymph nodes in suspected breast cancer: a pilot study. Clin Radiol. 2011; 66:1064–1071.8. Cooper KL, Meng Y, Harnan S, et al. Positron emission tomography (PET) and magnetic resonance imaging (MRI) for the assessment of axillary lymph node metastases in early breast cancer: systematic review and economic evaluation. Health Technol Assess. 2011; 15:iii–iv. 1–134.9. Deserno WM, Harisinghani MG, Taupitz M, et al. Urinary bladder cancer: preoperative nodal staging with ferumoxtran-10-enhanced MR imaging. Radiology. 2004; 233:449–456.10. Keller TM, Michel SC, Frohlich J, et al. USPIO-enhanced MRI for preoperative staging of gynecological pelvic tumors: preliminary results. Eur Radiol. 2004; 14:937–944.11. Koh DM, Brown G, Temple L, et al. Rectal cancer: mesorectal lymph nodes at MR imaging with USPIO versus histopathologic findings--initial observations. Radiology. 2004; 231:91–99.12. Harisinghani MG, Barentsz J, Hahn PF, et al. Noninvasive detection of clinically occult lymph-node metastases in prostate cancer. N Engl J Med. 2003; 348:2491–2499.13. Hudgins PA, Anzai Y, Morris MR, Lucas MA. Ferumoxtran-10, a superparamagnetic iron oxide as a magnetic resonance enhancement agent for imaging lymph nodes: a phase 2 dose study. AJNR Am J Neuroradiol. 2002; 23:649–656.14. Weissleder R, Elizondo G, Wittenberg J, Rabito CA, Bengele HH, Josephson L. Ultrasmall superparamagnetic iron oxide: characterization of a new class of contrast agents for MR imaging. Radiology. 1990; 175:489–493.15. Fleiss JL. Analysis of data from multiclinic trials. Control Clin Trials. 1986; 7:267–275.16. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560.17. Memarsadeghi M, Riedl CC, Kaneider A, et al. Axillary lymph node metastases in patients with breast carcinomas: assessment with nonenhanced versus uspio-enhanced MR imaging. Radiology. 2006; 241:367–377.18. Nakai G, Matsuki M, Harada T, et al. Evaluation of axillary lymph nodes by diffusion-weighted MRI using ultrasmall superparamagnetic iron oxide in patients with breast cancer: initial clinical experience. J Magn Reson Imaging. 2011; 34:557–562.19. Kimura K, Tanigawa N, Matsuki M, et al. High-resolution MR lymphography using ultrasmall superparamagnetic iron oxide (USPIO) in the evaluation of axillary lymph nodes in patients with early stage breast cancer: preliminary results. Breast Cancer. 2010; 17:241–246.20. Harada T, Tanigawa N, Matsuki M, Nohara T, Narabayashi I. Evaluation of lymph node metastases of breast cancer using ultrasmall superparamagnetic iron oxide-enhanced magnetic resonance imaging. Eur J Radiol. 2007; 63:401–407.21. Michel SC, Keller TM, Frohlich JM, et al. Preoperative breast cancer staging: MR imaging of the axilla with ultrasmall superparamagnetic iron oxide enhancement. Radiology. 2002; 225:527–536.22. Stadnik TW, Everaert H, Makkat S, Sacre R, Lamote J, Bourgain C. Breast imaging. Preoperative breast cancer staging: comparison of USPIO-enhanced MR imaging and 18F-fluorodeoxyglucose (FDC) positron emission tomography (PET) imaging for axillary lymph node staging--initial findings. Eur Radiol. 2006; 16:2153–2216.23. Stets C, Brandt S, Wallis F, Buchmann J, Gilbert FJ, Heywang-Kobrunner SH. Axillary lymph node metastases: a statistical analysis of various parameters in MRI with USPIO. J Magn Reson Imaging. 2002; 16:60–68.24. Schipper RJ, Smidt ML, van Roozendaal LM, et al. Noninvasive nodal staging in patients with breast cancer using gadofosveset-enhanced magnetic resonance imaging: a feasibility study. Invest Radiol. 2013; 48:134–139.25. Mumtaz H, Hall-Craggs MA, Davidson T, et al. Staging of symptomatic primary breast cancer with MR imaging. AJR Am J Roentgenol. 1997; 169:417–424.26. Baltzer PA, Dietzel M, Burmeister HP, et al. Application of MR mammography beyond local staging: is there a potential to accurately assess axillary lymph nodes? Evaluation of an extended protocol in an initial prospective study. AJR Am J Roentgenol. 2011; 196:W641–W647.27. Hwang SO, Lee SW, Kim HJ, Kim WW, Park HY, Jung JH. The comparative study of ultrasonography, contrast-enhanced MRI, and (18)F-FDG PET/CT for detecting axillary lymph node metastasis in T1 breast cancer. J Breast Cancer. 2013; 16:315–321.28. Kvistad KA, Rydland J, Smethurst HB, Lundgren S, Fjosne HE, Haraldseth O. Axillary lymph node metastases in breast cancer: preoperative detection with dynamic contrast-enhanced MRI. Eur Radiol. 2000; 10:1464–1471.29. Murray AD, Staff RT, Redpath TW, et al. Dynamic contrast enhanced MRI of the axilla in women with breast cancer: comparison with pathology of excised nodes. Br J Radiol. 2002; 75:220–228.30. Valente SA, Levine GM, Silverstein MJ, et al. Accuracy of predicting axillary lymph node positivity by physical examination, mammography, ultrasonography, and magnetic resonance imaging. Ann Surg Oncol. 2012; 19:1825–1830.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnostic value of magnetic resonance imaging using superparamagnetic iron oxide for axillary node metastasis in patients with breast cancer: a meta-analysis
- Use of Abbreviated Magnetic Resonance Imaging in Breast Cancer Screening
- Breast Cancer Screening with MRI
- Carcinoma of the Axillary Tail of Spence: A Case Report with Imaging Findings
- A Recurrence of Ovarian Carcinoma Presenting as Only Axillary Lymphatic Metastasis: A Case Report