J Korean Soc Radiol.
2019 Jan;80(1):47-58. 10.3348/jksr.2019.80.1.47.
Use of Abbreviated Magnetic Resonance Imaging in Breast Cancer Screening
- Affiliations
-
- 1Department of Radiology, Seoul National University Hospital, Seoul, Korea. suhyune82@gmail.com
- KMID: 2442463
- DOI: http://doi.org/10.3348/jksr.2019.80.1.47
Abstract
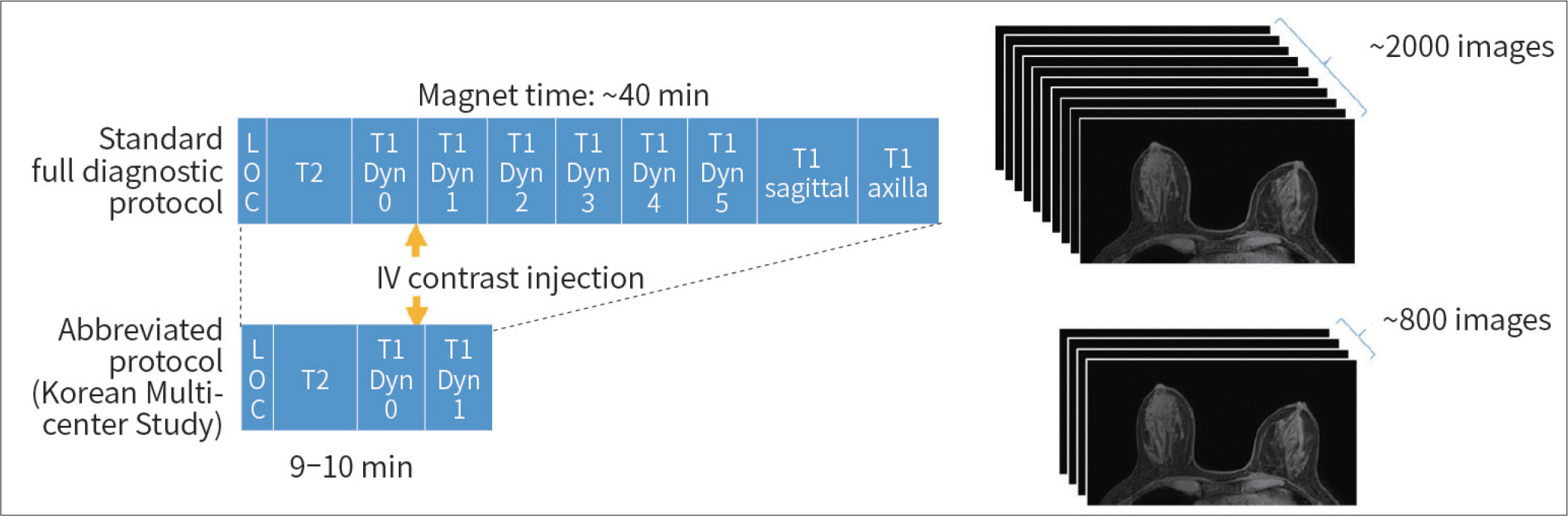
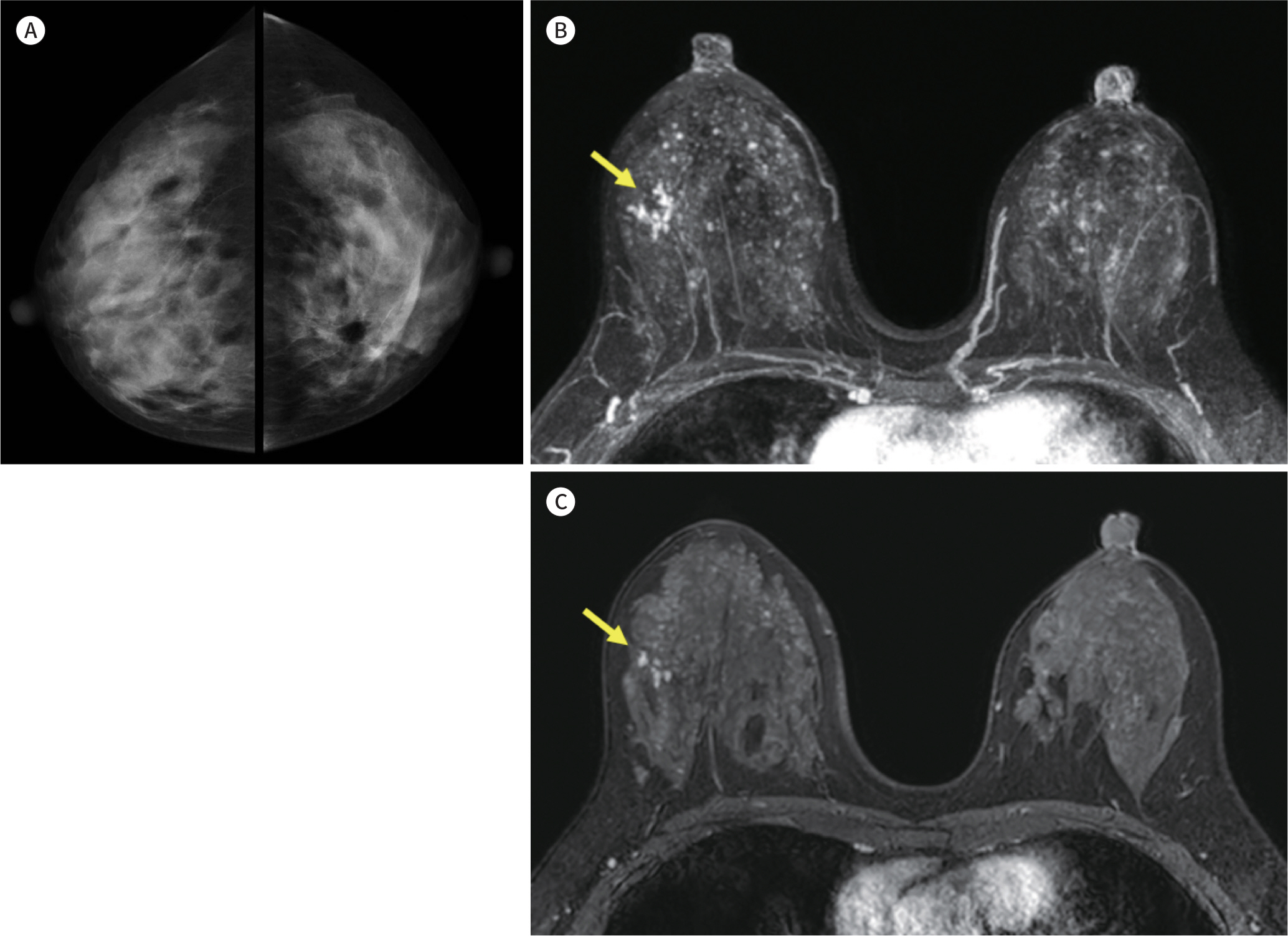
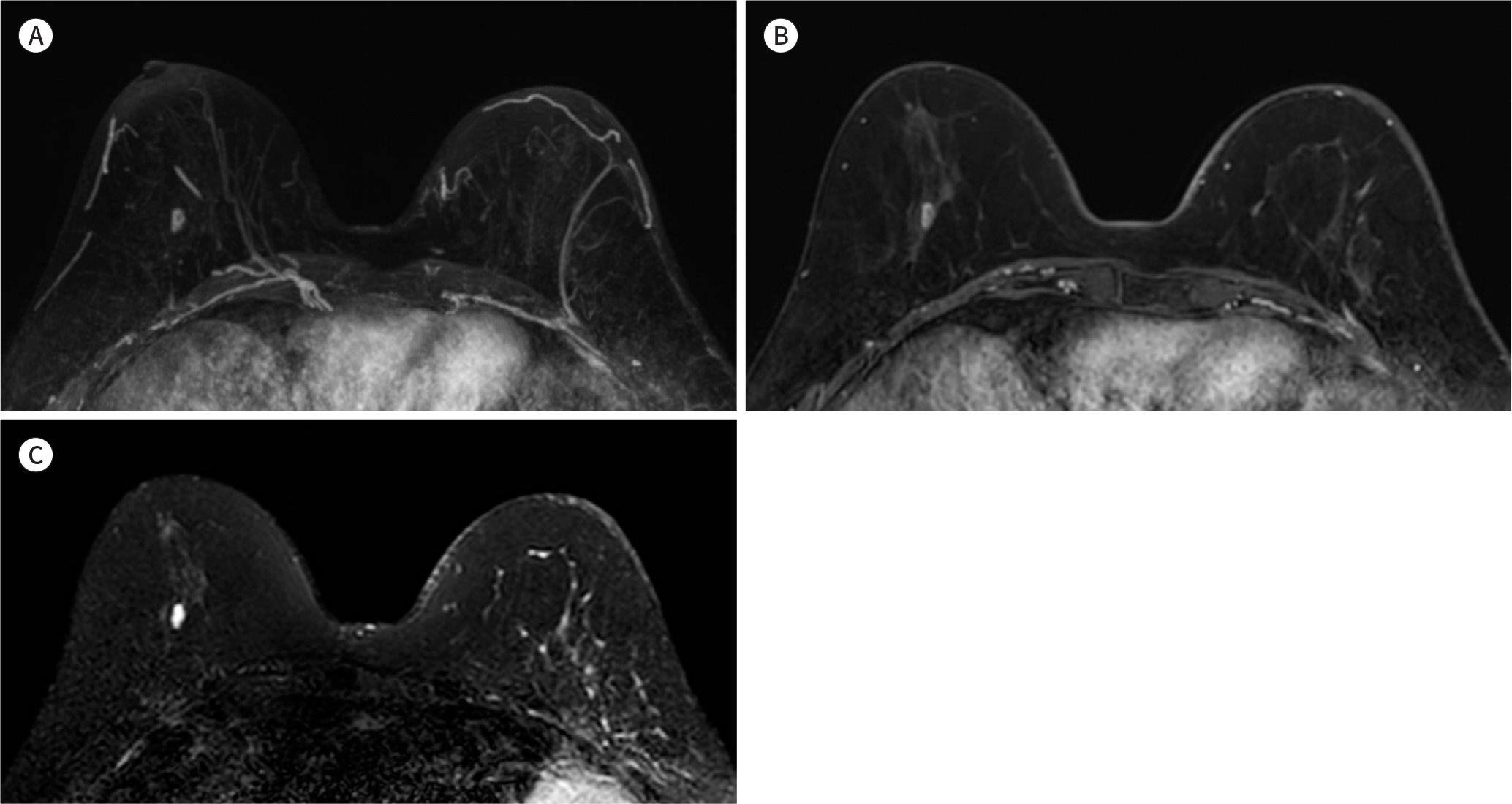
- Magnetic resonance imaging (MRI) is the most sensitive modality used for breast cancer screening, and is known to detect biologically significant cancers and few interval cancers. Application of standard breast MRI examination is not economical for screening due to the high costs associated with long interpretation and reading times. However, abbreviated breast MRI can reduce time and cost while maintaining diagnostic accuracy, and improve cost-effectiveness in breast cancer screening. A multi-center clinical trial on breast cancer screening using abbreviated breast MRI in high-risk women in Korea is being conducted. Another multicenter clinical trial has been conducted in the USA and Europe to investigate the efficacy of abbreviated breast MRI in women with average to intermediate cancer risk. Furthermore, when performed simultaneously with ultrafast MRI, the accuracy of abbreviated breast MRI can be enhanced. However, since abbreviated breast MRI uses contrast agents, it is important to consider the possibility of residual gadolinium in the body.
MeSH Terms
Figure
Reference
-
References
1. de Koning HJ. Mammographic screening: evidence from randomised controlled trials.Ann Oncol. 2003; 14:1185–1189.2. Tabár L, Vitak B, Chen TH, Yen AM, Cohen A, Tot T, et al. Swedish two-county trial: impact of mammographic screening on breast cancer mortality during 3 decades. Radiology. 2011; 260:658–663.
Article3. Feig S. Cost-effectiveness of mammography, MRI, and ultrasonography for breast cancer screening. Radiol Cl/iin North Am. 2010; 48:879–891.
Article4. Kolb TM, Lichy J, Newhouse JH. Comparison of the performance of screening mammography, physical examination, and breast US and evaluation of factors that influence them: an analysis of 27,825 patient evaluations.Radiology. 2002; 225:165–175.5. Houssami N, Hunter K. The epidemiology, radiology and biological characteristics of interval breast cancers in population mammography screening. NPJ Breast Cancer. 2017; 3:12.
Article6. Sung JS, Stamler S, Brooks J, Kaplan J, Huang T, Dershaw DD, et al. Breast cancers detected at screening MR imaging and mammography in patients at high risk: method of detection reflects tumor histopathologic results. Radiology. 2016; 280:716–722.
Article7. Kuhl C. The current status of breast MR imaging. Part I. choice of technique, image interpretation, diagnostic accuracy, and transfer to clinical practice. Radiology. 2007; 244:356–378.
Article8. Kuhl CK, Schrading S, Strobel K, Schild HH, Hilgers RD, Bieling HB. Abbreviated breast magnetic resonance imaging (MRI): first postcontrast subtracted images and maximum-intensity projection-a novel approach to breast cancer screening with MRI. J Clin Oncol. 2014; 32:2304–2310.
Article9. Haygood TM, Wang J, Atkinson EN, Lane D, Stephens TW, Patel P, et al. Timed efficiency of interpretation of digital and film-screen screening mammograms. AJR Am J Roentgenol. 2009; 192:216–220.
Article10. Berns EA, Hendrick RE, Solari M, Barke L, Reddy D, Wolfman J, et al. Digital and screen-film mammography: comparison of image acquisition and interpretation times. AJR Am J Roentgenol. 2006; 187:38–41.
Article11. Mango VL, Morris EA, David Dershaw D, Abramson A, Fry C, Moskowitz CS, et al. Abbreviated protocol for breast MRI: are multiple sequences needed for cancer detection? Eur J Radiol. 2015; 84:65–70.
Article12. Grimm LJ, Soo MS, Yoon S, Kim C, Ghate SV, Johnson KS. Abbreviated screening protocol for breast MRI: a feasibility study. Acad Radiol. 2015; 22:1157–1162.13. Harvey SC, Di Carlo PA, Lee B, Obadina E, Sippo D, Mullen L. An abbreviated protocol for high-risk screening breast MRI saves time and resources. J Am Coll Radiol. 2016; 13:R74–R80.
Article14. Heacock L, Melsaether AN, Heller SL, Gao Y, Pysarenko KM, Babb JS, et al. Evaluation of a known breast cancer using an abbreviated breast MRI protocol: Correlation of imaging characteristics and pathology with lesion detection and conspicuity.Eur J Radiol. 2016; 85:815–823.15. Moschetta M, Telegrafo M, Rella L, Stabile Ianora AA, Angelelli G. Abbreviated combined MR protocol: a new faster strategy for characterizing breast lesions.Clin Breast Cancer. 2016; 16:207–211.16. Kuhl CK. Abbreviated breast MRI for screening women with dense breast: the EA1141 trial.Br J Radiol. 2018; 91:20170441.17. Lee SH, Moon WK. Screening using low-cost abbreviated MRI in women with high-risk for breast cancer. Journal of the Korean Soc/iiety for Breast Screening. 2017; 14:73–79.18. Saslow D, Boetes C, Burke W, Harms S, Leach MO, Lehman CD, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Cl/iin. 2007; 57:75–89.
Article19. Kriege M, Brekelmans CT, Boetes C, Besnard PE, Zonderland HM, Obdeijn IM, et al. Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition.N Engl J Med. 2004; 351:427–437.20. Warner E, Plewes DB, Hill KA, Causer PA, Zubovits JT, Jong RA, et al. Surveillance of BRCA1 and BRCA2 mutation carriers with magnetic resonance imaging, ultrasound, mammography, and clinical breast examination.JAMA. 2004; 292:1317–1325.21. Kuhl CK, Schrading S, Leutner CC, Morakkabati-Spitz N, Wardelmann E, Fimmers R, et al. Mammography, breast ultrasound, and magnetic resonance imaging for surveillance of women at high familial risk for breast cancer. J Clin Oncol. 2005; 23:8469–8476.
Article22. Leach MO, Boggis CR, Dixon AK, Easton DF, Eeles RA, Evans DG, et al. Screening with magnetic resonance imaging and mammography of a UK population at high familial risk of breast cancer: a prospective multi-centre cohort study (MARIBS). Lancet. 2005; 365:1769–1778.23. Sardanelli F, Podo F, D'Agnolo G, Verdecchia A, Santaquilani M, Musumeci R, et al. Multicenter comparative multimodality surveillance of women at genetic-familial high risk for breast cancer (HIBCRIT study): interim results.Rad/iiology. 2007; 242:698–715.24. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Genetic/Familial High-Risk Assessment: Breast and Ovarian Version 3.2019 Available at. http://www.nccn.org/professionals/physician_gls/pdf/genetics_screening.pdf. Published 2019. Accessed Jan 22,. 2019.25. Cho N, Han W, Han BK, Bae MS, Ko ES, Nam SJ, et al. Breast cancer screening with mammography plus ultrasonography or magnetic resonance imaging in women 50 years or younger at diagnosis and treated with breast conservation therapy. JAMA Oncol. 2017; 3:1495–1502.
Article26. Kang E, Seong MW, Park SK, Lee JW, Lee J, Kim LS, et al. The prevalence and spectrum of BRCA1 and BRCA2 mutations in Korean population: recent update of the Korean Hereditary Breast Cancer (KOHBRA) study. Breast Cancer Res Treat. 2015; 151:157–168.
Article27. Korean Breast Cancer Society. The 7th Korean Clinical Practice Guideline for Breast Cancer 2017. Seoul: Korean Breast Cancer Society;2017.28. Kuhl CK, Strobel K, Bieling H, Leutner C, Schild HH, Schrading S. Supplemental breast MR imaging screening of women with average risk of breast cancer. Radiology. 2017; 283:361–370.29. Houssami N, Ciatto S, Martinelli F, Bonardi R, Duffy SW. Early detection of second breast cancers improves prognosis in breast cancer survivors.Ann Oncol. 2009; 20:1505–1510.30. Gweon HM, Cho N, Han W, Yi A, Moon HG, Noh DY, et al. Breast MR imaging screening in women with a history of breast conservation therapy. Radiology. 2014; 272:366–373.
Article31. Kim EJ, Kang BJ, Kim SH, Youn IK, Baek JE, Lee HS. Diagnostic performance of and breast tissue changes at early breast MR imaging surveillance in women after breast conservation therapy. Radiology. 2017; 284:656–666.
Article32. Choi BH, Choi N, Kim MY, Yang JH, Yoo YB, Jung HK. Usefulness of abbreviated breast MRI screening for women with a history of breast cancer surgery.Breast Cancer Res Treat. 2018; 167:495–502.33. Vreemann S, Rodriguez-Ruiz A, Nickel D, Heacock L, Appelman L, van Zelst J, et al. Compressed sensing for breast MRI: resolving the trade-off between spatial and temporal resolution. Invest Radiol. 2017; 52:574–582.
Article34. Chhor CM, Mercado CL. Abbreviated MRI protocols: wave of the future for breast cancer screening.AJR Am J Roentgenol. 2017; 208:284–289.35. McDonald RJ, McDonald JS, Kallmes DF, Jentoft ME, Murray DL, Thielen KR, et al. Intracranial gadolinium deposition after contrast-enhanced MR imaging.Radiology. 2015; 275:772–782.36. Kanda T, Oba H, Toyoda K, Kitajima K, Furui S. Brain gadolinium deposition after administration of gadolinium-based contrast agents. Jpn J Radiol. 2016; 34:3–9.
Article37. Gulani V, Calamante F, Shellock FG, Kanal E, Reeder SB; International Society for Magnetic Resonance in Medicine. Gadolinium deposition in the brain: summary of evidence and recommendations.Lancet Neurol. 2017; 16:564–570.38. Kanda T, Osawa M, Oba H, Toyoda K, Kotoku J, Haruyama T, et al. High signal intensity in dentate nucleus on unenhanced T1-weighted MR images: association with linear versus macrocyclic gadolinium chelate administration. Radiology. 2015; 275:803–809.
Article39. Pullicino R, Radon M, Biswas S, Bhojak M, Das K. A review of the current evidence on gadolinium deposition in the brain.Clin Neuroradiol. 2018; 28:159–169.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Abbreviated Magnetic Resonance Imaging for Breast Cancer Screening: Concept, Early Results, and Considerations
- Abbreviated Breast Magnetic Resonance Imaging: Background, Evidence From Studies, and Future Considerations
- A Systematic Review on Radiologists' Knowledge of Breast Cancer Screening
- Recent Updates of Abbreviated MRI for Hepatocellular Carcinoma Screening
- Current opinion for breast cancer screening