Chonnam Med J.
2009 Apr;45(1):55-59. 10.4068/cmj.2009.45.1.55.
Efficacy of Amniotic Membrane Transplantation on Corneal Graft Rejection with Epithelial Defects after Penetrating Keratoplasty
- Affiliations
-
- 1Department of Ophthalmology, Chonnam National University Medical School and Hospital, Gwangju, Korea. kcyoon@chonnam.ac.kr
- 2Department of Obstetrics and Gynecology, Chonnam National University Medical School and Hospital, Gwangju, Korea.
- 3Chonnam National University Research Institute of Medical Sciences, Gwangju, Korea.
- 4Department of Ophthalmology, Seonam Hospital, Seonam University, Gwangju, Korea.
- KMID: 2172284
- DOI: http://doi.org/10.4068/cmj.2009.45.1.55
Abstract
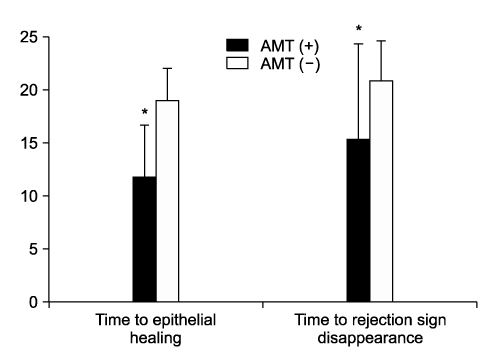
- We report the therapeutic effect of amniotic membrane transplantation (AMT) on corneal graft rejection with epithelial defects after penetrating keratoplasty (PKP). Twelve patients (12 eyes) who had epithelial and subepithelial graft rejection received human AMT, and they were compared with other 12 patients (12 eyes) who were treated with medication only. There were no differences in age, sex, time to rejection after PKP, and epithelial defect area between two groups. Time to epithelial healing and time to disappearance of rejection sign were significantly shorter in the AMT group (11.8+/-4.9 days and 15.5+/-6.3 days) than in the medical treatment group (19.0+/-3.7 days and 20.8+/-3.4 days)(p=0.01, p=0.02). AMT is effective in promoting epithelialization and improving inflammation of epithelial rejection after penetrating keratoplasty.
MeSH Terms
Figure
Reference
-
1. Foster CS, Azar DT, Dohlman CH. The cornea. 2005. 4th ed. Philadelphia: Lippincott Williams & Wilkins;1035–1061.2. Fraunfelder FW. Corneal toxicity from topical ocular and systemic medications. Cornea. 2006. 25:1133–1138.
Article3. Kim JC, Tseng SC. Transplantation of preserved human amniotic membrane for surface reconstruction in severely damaged rabbit corneas. Cornea. 1995. 14:473–484.
Article4. Hori J, Wang M, Kamiya K, Takahashi H, Sakuragawa N. Immunological characteristics of amniotic epithelium. Cornea. 2006. 25(10):Suppl 1. S53–S58.
Article5. Mayer DJ, Casey TA. Reducing the risk of corneal graft rejection. Acomparison of different methods. Cornea. 1987. 6:261–268.6. Alldredge OC, Krachmer JH. Clinical types of corneal transplant rejection. There manifestations, frequency, preoperative correlates and treatment. Arch Ophthalmol. 1981. 99:599–604.7. Figueiredo FC, Nicholls SM, Easty DL. Corneal epithelial rejection in the rat. Invest Ophthalmol Vis Sci. 2002. 43:729–736.8. Prabhasawat P, Tesavibul N, Komolsuradej W. Single and multilayer amniotic membrane transplantation for persistent corneal epithelial defect with and without stromal thinning and perforation. Br J Ophthalmol. 2001. 85:1455–1463.
Article9. Spigelman AV, Deutsch TA, Sugar J. Application of homologous fibronectin to persistent human corneal epithelial defect. Cornea. 1987. 6:128–130.
Article10. Lee SH, Tseng SC. Amniotic membrane transplantation for persistent epithelial defects with ulceration. Am J Ophthalmol. 1997. 123:303–312.
Article11. Dios E, Herreras JM, Mayo A, Blanco G. Efficacy of systemic cyclosporine A and amniotic membrane on rabbit conjunctival limbal allograft rejection. Cornea. 2005. 24:182–188.
Article12. Yao YF, Zhang YM, Zou P, Zhang B, Qiu WY, Tseng SC. Therapeutic penetrating keratoplasty in severe fungal keratitis using cryopreserved donor corneas. Br J Ophthalmol. 2003. 87:543–547.
Article13. Li DQ, Lee SB, Tseng SC. Differential expression and regulation of TGF-beta1, TGF-beta2, TGF-beta3, TGF-betaRI, TGF-betaRII and TGF-betaRIII in culture human corneal, limbal, and conjunctival fibroblasts. Curr Eye Res. 1999. 19:154–161.
Article14. Azuara-Blanco A, Pillai CT, Dua HS. Amniotic membrane transplantation for ocular surface reconstruction. Br J Ophathalmol. 1999. 83:399–402.
Article15. Hill JC. The use of cyclosporine in high-risk keratoplasty. Am J Ophthalmol. 1989. 107:506–510.
Article16. Lim BK, Tchah HW. Effect of topical FK506 at experimental corneal xenograft. J Korean Ophthalmol Soc. 1998. 39:847–854.17. Xu KP, Wu Y, Zhou J, Zhang X. Survival of rabbit limbal stem cell allografts after administration of cyclosporin A. Cornea. 1999. 18:459–465.
Article18. Dua HS, Azuara-Blanco A. Allo-limbal transplantation in patients with limbal stem cell deficiency. Br J Ophthalmol. 1999. 83:414–419.
Article19. Holland EF, Djalilian AR, Schwartz GS. Management of aniridic keratopathy with keratolimbal allograft: a limbal stem cell transplantation technique. Ophthalmology. 2003. 110:125–130.
Article20. Kim EC, Kim MS. Graft rejection in penetrating keratoplasty. J Korean Ophthalmol Soc. 2003. 44:289–295.21. Feldman ST. The effect of epidermal growth factor on corneal wound healing: practical considerations for therapeutic use. Refract Corneal Surg. 1991. 7:232–239.
Article22. Chen HC, Tan HY, Hsiao CH, Hyang SC, Lin KK, Ma DH. Amniotic membrane transplantation for persistent corneal ulcers and perforations in acute fungal keratitis. Cornea. 2006. 25:564–572.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Human Amniotic Membrane Transplantation for Treatment of Fungal Ulcer
- Amniotic Membrane Transplantation in Perforation or Impending Perforation of Cornea
- The Difference in Graft Rejection between Two Corneal Preservation Methods(Moist Chamber vs Optisol)
- Clinical Results of Graft Rejection Related to Graft Size after Keratoplasty in Keratoconus
- Amniotic Membrane Transplantation for Perforation and Impending Perforation of Cornea: Four Cases