Infect Chemother.
2012 Oct;44(5):367-371. 10.3947/ic.2012.44.5.367.
Clinical and Epidemiologic Characteristics of Mycoplasma pneumoniae Pneumonia in Adults During 2011 Epidemic
- Affiliations
-
- 1Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea. heejinmd@korea.ac.kr
- KMID: 2170381
- DOI: http://doi.org/10.3947/ic.2012.44.5.367
Abstract
- BACKGROUND
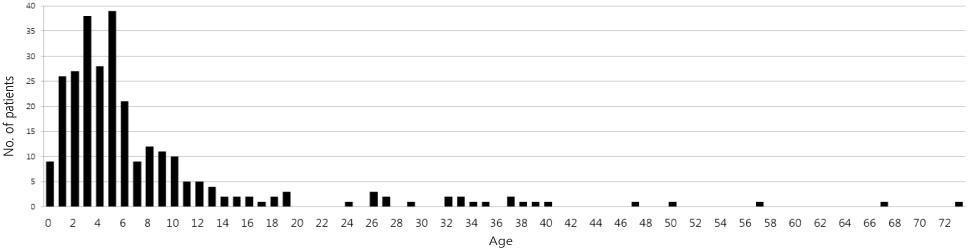
Recent data regarding the clinical epidemiologic characteristics of Mycoplasma pneumoniae pneumonia in Korean adults are insufficient. This study was conducted in order to compare epidemics in different ages and to identify the clinical characteristics in adults. MATERIAL AND METHODS: We investigated patients who visited Korea University Guro Hospital from January to December 2011 due to community acquired pneumonia and underwent mycoplasma antibody tests. M. pneumoniae pneumonia was diagnosed if mycoplasma antibody titer was > or =1:320 at any time, seroconversion or 4-fold rise was seen at convalescent phase. Patients under the age of 19 were classified as child and adolescent, otherwise adult. We investigated the number of monthly cases in all patients and reviewed the medical records of adult patients.
RESULTS
A total of 249 young patients aged < or =18 years and 29 adults were diagnosed with M. pneumoniae pneumonia. Among young patients, 75.5% were concentrated in the 0-6 years age group and 58.6% of adults belonged to the 26-40 years age group. The number of young patients began to increase in July and continued to increase in December, while the number of adult patients began to increase in August and occurred continuously until December. The correlation coefficient of the epidemic trend between the two groups was 0.682 (P=0.015). Median age of adult patients was 33.3 years. Fever was observed in all patients and 25 patients (86.2%) complained of purulent sputum. The average white blood cell count was 7,066/mm3. The average values for aspartate aminotransferase, alanine aminotransferase, creatinine, and sodium were within the normal range. In chest X-ray study, ipsilateral lower patchy consolidation was found in 24 patients (82.8%). Twenty one adult patients (72.4%) were hospitalized. The mean duration of hospitalization was 7.3 days. Twenty three patients (79.3%) were initially treated with combinations of third generation cephalosporin and macrolide. Among them, five patients (17.2%) showed poor responses. Six cases (20.7%) were initially treated with quinolone, and treatment was maintained until the end without changing antibiotics. Development of cryptogenic organizing pneumonia occurred in one case and there was no occurrence of death.
CONCLUSIONS
When M. pneumoniae pneumonia is epidemic among children and adolescents, it should also be suspected in adult patients with community-acquired pneumonia. Some patients showed poor responses to macrolide. Overall, it appears that additional studies are needed for evaluation of the effectiveness of macrolide in treatment of M. pneumoniae pneumonia in adults.
Keyword
MeSH Terms
-
Adolescent
Adult
Aged
Alanine Transaminase
Anti-Bacterial Agents
Aspartate Aminotransferases
Child
Creatinine
Cryptogenic Organizing Pneumonia
Fever
Hospitalization
Humans
Korea
Leukocyte Count
Macrolides
Medical Records
Mycoplasma
Mycoplasma pneumoniae
Pneumonia
Pneumonia, Mycoplasma
Reference Values
Sodium
Sputum
Thorax
Alanine Transaminase
Anti-Bacterial Agents
Aspartate Aminotransferases
Creatinine
Macrolides
Sodium
Figure
Reference
-
1. Denny FW, Clyde WA Jr, Glezen WP. Mycoplasma pneumoniae disease: clinical spectrum, pathophysiology, epidemiology, and control. J Infect Dis. 1971. 123:74–92.
Article2. Kim JW, Seo HK, Yoo EG, Park SJ, Yoon SH, Jung HY, Han MY. Mycoplasma pneumoniae pneumonia in Korean children, from 1979 to 2006-a meta-analysis. Korean J Pediatr. 2009. 52:315–323.
Article3. Chong YP, Jung KS, Lee KH, Kim MN, Moon SM, Park S, Hur J, Kim DM, Jeon MH, Woo JH. The bacterial etiology of community-acquired pneumonia in Korea: a nationwide prospective multicenter study. Infect Chemother. 2010. 42:397–403.
Article4. Foy HM, Kenny GE, Cooney MK, Allan ID. Long-term epidemiology of infections with Mycoplasma pneumoniae. J Infect Dis. 1979. 139:681–687.
Article5. Mansel JK, Rosenow EC 3rd, Smith TF, Martin JW Jr. Mycoplasma pneumoniae pneumonia. Chest. 1989. 95:639–646.
Article6. Luby JP. Pneumonia caused by Mycoplasma pneumoniae infection. Clin Chest Med. 1991. 12:237–244.
Article7. Clyde WA Jr. Clinical overview of typical Mycoplasma pneumoniae infections. Clin Infect Dis. 1993. 17:Suppl 1. S32–S36.8. Marrie TJ. Mycoplasma pneumoniae pneumonia requiring hospitalization, with emphasis on infection in the elderly. Arch Intern Med. 1993. 153:488–494.
Article9. Isozumi R, Yoshimine H, Morozumi M, Ubukata K, Ariyoshi K. Adult community-acquired pneumonia caused by macrolide resistant Mycoplasma pneumoniae. Respirology. 2009. 14:1206–1208.
Article10. Liu Y, Ye X, Zhang H, Xu X, Li W, Zhu D, Wang M. Antimicrobial susceptibility of Mycoplasma pneumoniae isolates and molecular analysis of macrolide-resistant strains from Shanghai, China. Antimicrob Agents Chemother. 2009. 53:2160–2162.
Article11. Oh CE, Choi EH, Lee HJ. Detection of genetic mutations associated with macrolide resistance of Mycoplasma pneumoniae. Korean J Pediatr. 2010. 53:178–183.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidemic Pneumonia Caused by Mycoplasma Pneumoniae
- A Case of Cerebral Infarction Complicated by Mycoplasma pneumoniae Pneumonia
- Clinical Observation on Pneumonia due to Mycoplasma Pneumoniae in Children
- Mycoplasma pneumoniae Pneumonia in Children
- A clinical study of mycoplasma pneumonia in children during recent 5 years