Endocrinol Metab.
2013 Dec;28(4):335-340. 10.3803/EnM.2013.28.4.335.
Papillary Thyroid Carcinoma: Four Cases Required Caution during Long-Term Follow-Up
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Research Institute of Clinical Medicine, Eulji University Hospital, Eulji University School of Medicine, Daejeon, Korea.
- 2Division of Endocrinology and Metabolism, Department of Internal Medicine, Research Institute of Clinical Medicine, Chonbuk National University Hospital, Chonbuk National University Medical School, Jeonju, Korea. mdjinhy@jbnu.ac.kr
- KMID: 2169313
- DOI: http://doi.org/10.3803/EnM.2013.28.4.335
Abstract
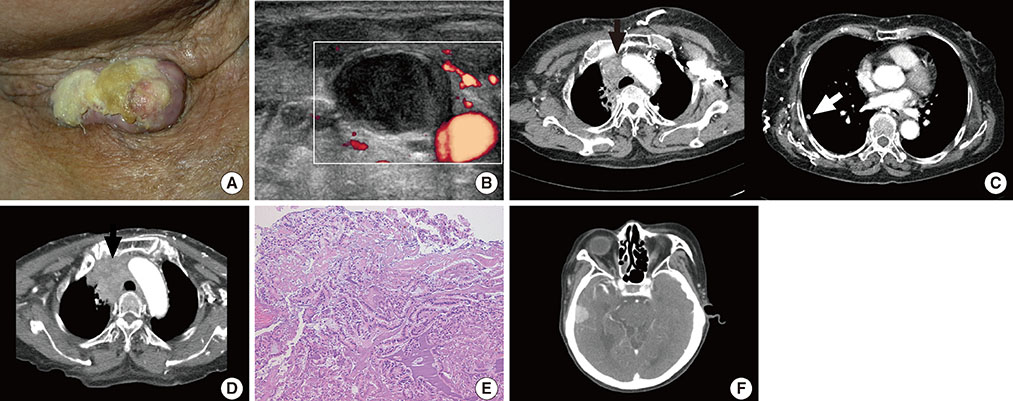
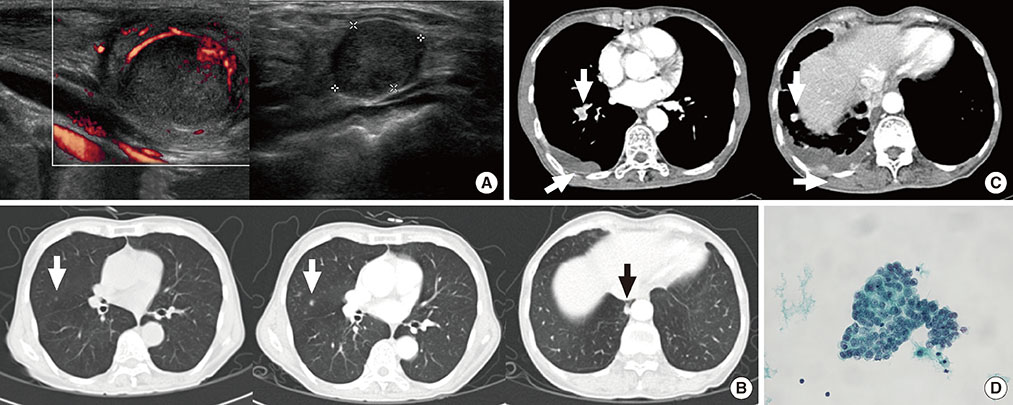
- Due to the increased prevalence of papillary thyroid carcinoma (PTC), difficult cases and unexpected events have become more common during long-term follow-up. Herein we reported four cases that exhibited poor progress during long-term follow-up. All the cases were diagnosed with PTC and treated with total thyroidectomy before several years, and the patients had been newly diagnosed with recurrent and metastatic PTC. These four cases included recurred PTC with invasion of large blood vessels, a concomitant second malignancy, malignant transformation, and refractoriness to treatment. Physicians should closely monitor patients to promptly address unforeseen circumstances during PTC follow-up, including PTC recurrence and metastasis. Furthermore, we suggest that the development of a management protocol for refractory or terminal PTC is also warranted.
MeSH Terms
Figure
Cited by 1 articles
-
Brief Review of Articles in '
Endocrinology and Metabolism ' in 2013
Won-Young Lee
Endocrinol Metab. 2014;29(3):251-256. doi: 10.3803/EnM.2014.29.3.251.
Reference
-
1. Emerson CH. Guidelines for guidelines: content, accountability, peer review, and intellectual ownership. Thyroid. 2009; 19:1137–1138.2. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19:1167–1214.3. Mallick UK. American Thyroid Association. The revised American Thyroid Association management guidelines 2009 for patients with differentiated thyroid cancer: an evidence-based risk-adapted approach. Clin Oncol (R Coll Radiol). 2010; 22:472–474.4. Mazzaferri EL, Young RL, Oertel JE, Kemmerer WT, Page CP. Papillary thyroid carcinoma: the impact of therapy in 576 patients. Medicine (Baltimore). 1977; 56:171–196.5. Wada N, Masudo K, Hirakawa S, Woo T, Arai H, Suganuma N, Iwaki H, Yukawa N, Uchida K, Imoto K, Rino Y, Masuda M. Superior vena cava (SVC) reconstruction using autologous tissue in two cases of differentiated thyroid carcinoma presenting with SVC syndrome. World J Surg Oncol. 2009; 7:75.6. Miranda ER, Padrao EL, Silva BC, De Marco L, Sarquis MS. Papillary thyroid carcinoma with brain metastases: an unusual 10-year-survival case. Thyroid. 2010; 20:657–661.7. Al-Dhahri SF, Al-Amro AS, Al-Shakwer W, Terkawi AS. Cerebellar mass as a primary presentation of papillary thyroid carcinoma: case report and literature review. Head Neck Oncol. 2009; 1:23.8. Roscoe KJ, Raja S, Tronic B, Dou Y. Single F-18 fluorodeoxyglucose positron emission tomography hypermetabolic focus containing metastatic papillary thyroid cancer within a primary scarring adenocarcinoma lung cancer. Clin Nucl Med. 2006; 31:359–360.9. Ogawa M, Hori H, Hirayama M, Kobayashi M, Shiraishi T, Watanabe Y, Komada Y. Anaplastic transformation from papillary thyroid carcinoma with increased serum CA19-9. Pediatr Blood Cancer. 2005; 45:64–67.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Concurrent Medullay and Papillary Carcinoma of the Thyroid
- Coexistence of Parathyroid and Papillary Thyroid Carcinoma
- Clnicopathologic Features of Warthin-like Papillary Carcinoma of the Thyroid
- A Case of Mixed Follicular-Papillary Thyroid Carcinoma
- A Case of Ectopic Thyroid Papillary Carcinoma with Incidental Papillary Thyroid Microcarcinoma