Endocrinol Metab.
2011 Sep;26(3):263-267. 10.3803/EnM.2011.26.3.263.
A Case of Central Pontine Myelinolysis in a Type 2 Diabetic Patient without Electrolyte Changes
- Affiliations
-
- 1Department of Internal Medicine, Maryknoll Medical Center, Busan, Korea. Jihyesuk@gmail.com
- 2Department of Neurology, Maryknoll Medical Center, Busan, Korea.
- 3Department of Radiology, Maryknoll Medical Center, Busan, Korea.
- KMID: 2169180
- DOI: http://doi.org/10.3803/EnM.2011.26.3.263
Abstract
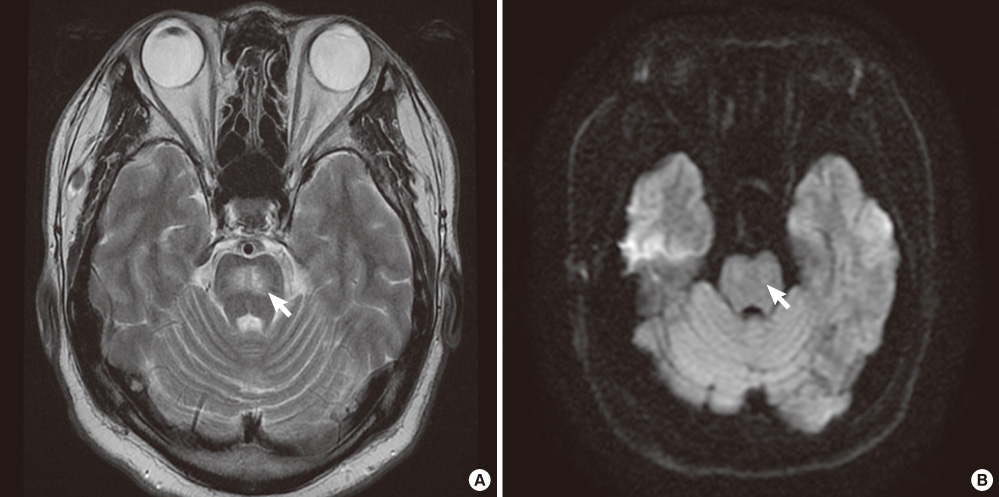
- Central pontine myelinolysis (CPM) by complicating rapid correction of severe hyponatremia has been widely reported. Additionally, CPM was occasionally reported among patients with post-liver transplantation, burns, chronic renal failure with dialysis, or other diseases associated with or not associated with other electrolyte changes or hyperosmolarity. However, there have been a few reports of CPM occurring in diabetic patients without documented electrolyte changes. This report is, to the best of our knowledge, the first report of CPM in type 2 diabetic patients without electrolyte changes in Korea. A 40-year-old man with type 2 diabetes mellitus with abruptly developed dysarthria and ataxia was admitted to our facility. He suffered from poor glucose control and multiple diabetic complications. Brain magnetic resonance imaging (MRI) revealed a well-defined bilateral symmetric hyperintense lesion in the central portion of the pons on T2- and diffusion-weighted images, which was consistent with CPM. After the patient's blood glucose and blood pressure normalized, his dysarthria and ataxia improved. Six months after discharge, follow-up MRI showed a persistent, but greatly reduced symmetric lesion in the central pons. It is certainly possible for CPM to be overlooked clinically in diabetic patients, but more cases could be diagnosed if careful attention was paid to this syndrome.
MeSH Terms
Figure
Reference
-
1. Adams RD, Victor M, Mancall EL. Central pontine myelinolysis: a hitherto undescribed disease occurring in alcoholic and malnourished patients. AMA Arch Neurol Psychiatry. 1959. 81:154–172.2. Norenberg MD, Leslie KO, Robertson AS. Association between rise in serum sodium and central pontine myelinolysis. Ann Neurol. 1982. 11:128–135.3. Laureno R. Central pontine myelinolysis following rapid correction of hyponatremia. Ann Neurol. 1983. 13:232–242.4. Messert B, Orrison WW, Hawkins MJ, Quaglieri CE. Central pontine myelinolysis. Considerations on etiology, diagnosis, and treatment. Neurology. 1979. 29:147–160.5. McKee AC, Winkelman MD, Banker BQ. Central pontine myelinolysis in severely burned patients: relationship to serum hyperosmolality. Neurology. 1988. 38:1211–1217.6. McComb RD, Pfeiffer RF, Casey JH, Wolcott G, Till DJ. Lateral pontine and extrapontine myelinolysis associated with hypernatremia and hyperglycemia. Clin Neuropathol. 1989. 8:284–288.7. Bonham CA, Dominguez EA, Fukui MB, Paterson DL, Pankey GA, Wagener MM, Fung JJ, Singh N. Central nervous system lesions in liver transplant recipients: prospective assessment of indications for biopsy and implications for management. Transplantation. 1998. 66:1596–1604.8. Tarhan NC, Agildere AM, Benli US, Ozdemir FN, Aytekin C, Can U. Osmotic demyelination syndrome in end-stage renal disease after recent hemodialysis: MRI of the brain. AJR Am J Roentgenol. 2004. 182:809–816.9. Jeong HK, Gwak MS, Kim GS. Central pontine myelinolysis after liver transplantation: a case report. Korean J Anesthesiol. 2006. 50:469–473.10. Jang SW, Kim IY, Kim JH, Song SH, Lee DW, Lee SB, Lee SJ, Kwak IS. A case of central pontine and extrapontine myelinolysis in a patient with maintenance hemodialysis. Korean J Nephrol. 2006. 25:327–331.11. Lim KH, Kim S, Lee YS, Kim KH, Kim J, Rhee J, Kim HJ, Yi HG, Oh SY, Lim JH, Han SW, Lee S, Kim I, Yoon SS, Park S, Kim BK. Central pontine myelinolysis in a patient with acute lymphoblastic leukemia after hematopoietic stem cell transplantation: a case report. J Korean Med Sci. 2008. 23:324–327.12. Casey E, Evans A, Krentz A, Watkins P, Hopkins D. Central pontine myelinolysis. An unusual complication of diabetes. Diabetes Care. 1999. 22:998–1000.13. Ichikawa H, Murakami H, Katoh H, Hieda S, Kawamura M. Central pontine lesions observed with MRI in four diabetic patients. Intern Med. 2008. 47:1425–1430.14. Koh CO, Yoon HS, Kim HK, Kim DM, Yoon DY, Lee JH, Kim WK. A case of extrapontine myelinolysis associated with hyperosmolar hyperglycemic syndrome. Korean J Med. 2005. 68:320–324.15. Skinhoj E, Strandgaard S. Pathogenesis of hypertensive encephalopathy. Lancet. 1973. 1:461–462.16. Iwata A, Koike F, Arasaki K, Tamaki M. Blood brain barrier destruction in hyperglycemic chorea in a patient with poorly controlled diabetes. J Neurol Sci. 1999. 163:90–93.17. Miller GM, Baker HL Jr, Okazaki H, Whisnant JP. Central pontine myelinolysis and its imitators: MR findings. Radiology. 1988. 168:795–802.18. Menger H, Jorg J. Outcome of central pontine and extrapontine myelinolysis (n = 44). J Neurol. 1999. 246:700–705.19. Laubenberger J, Schneider B, Ansorge O, Gotz F, Haussinger D, Volk B, Langer M. Central pontine myelinolysis: clinical presentation and radiologic findings. Eur Radiol. 1996. 6:177–183.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of central pontine and extrapontine myelinolysis with early hypermetabolism on 18FDG-PET scan
- A Case of Asymptomatic Central Pontine Myelinolysis after Severe Hypoglycemia in a Patient with Diabetic Nephropathy
- Central Pontine and Extrapontine Myelinolysis in a Patient with Traumatic Brain Injury Following Not Rapid Correction of Hyponatremia: A Case Report
- A Case of Subacute Onset Choreoathetosis as Sequelae of Central Pontine and Extrapontine Myelinolysis
- Neuropsychological Findings of Extrapontine Myelinolysis without Central Pontine Myelinolysis: Initial and Follow-up Evaluation