Ann Surg Treat Res.
2014 Dec;87(6):336-339. 10.4174/astr.2014.87.6.336.
Axillary sparganosis which was misunderstood lymph node metastasis during neoadjuvant chemotheraphy in a breast cancer patient
- Affiliations
-
- 1Department of Surgery, Konkuk University Medical Center, Seoul, Korea. 0117652771@kuh.ac.kr
- KMID: 2167091
- DOI: http://doi.org/10.4174/astr.2014.87.6.336
Abstract
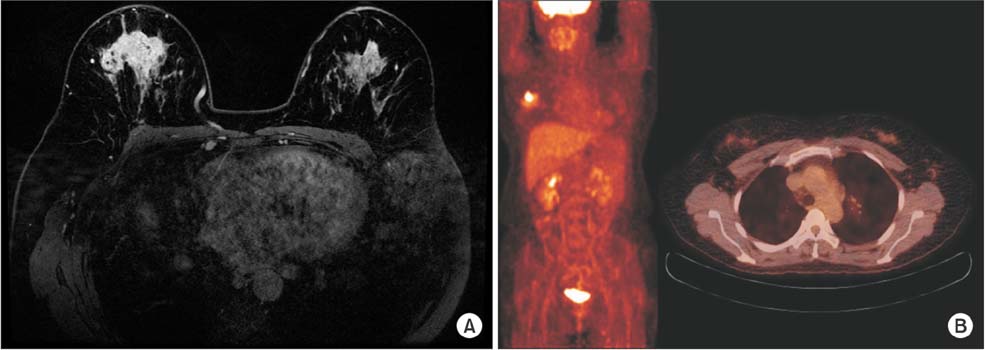
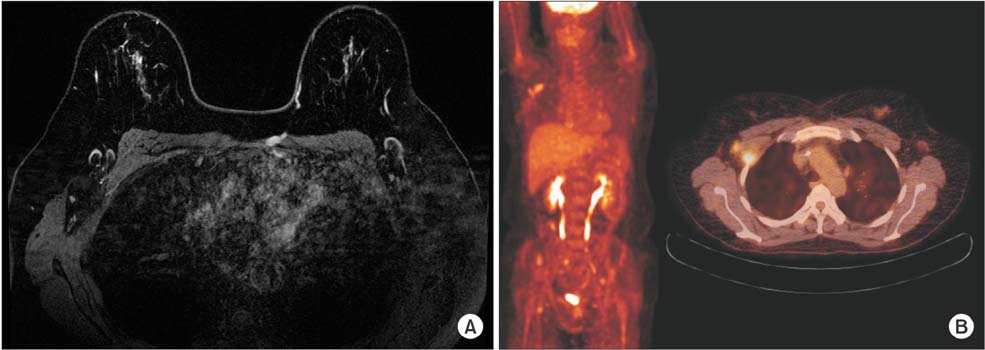
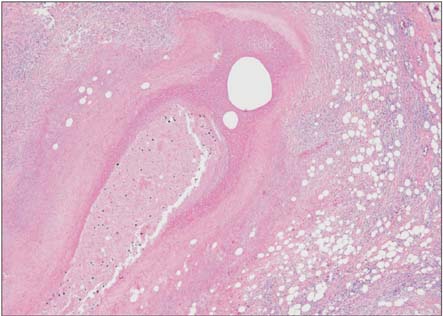
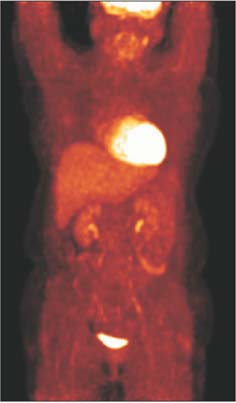
- Sparganosis of the breast is an uncommon disease, but should be considered in the differential diagnosis of unusual and suspicious breast masses. A history of ingesting contaminated water and direct ingestion of snakes and frogs may help in differential diagnosis of the mass. Complete surgical removal is the treatment of choice and provides a definite diagnosis. We report a case of multiple axillary lymph node sparganosis. It was first considered as an axillary metastasis of breast cancer because a newly axillary mass appeared in follow-up radiologic study after neoadjuvant chemotherapy. We performed curative breast cancer surgery and sparganosis was confirmed by extracting the worm during axillary dissection.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Human Sparganosis in Korea
Jeong-Geun Kim, Chun-Seob Ahn, Woon-Mok Sohn, Yukifumi Nawa, Yoon Kong
J Korean Med Sci. 2018;33(44):. doi: 10.3346/jkms.2018.33.e273.
Reference
-
1. Park JH, Chai JW, Cho N, Paek NS, Guk SM, Shin EH, et al. A surgically confirmed case of breast sparganosis showing characteristic mammography and ultrasonography findings. Korean J Parasitol. 2006; 44:151–156.2. Kim HY, Kang CH, Kim JH, Lee SH, Park SY, Cho SW. Intramuscular and subcutaneous sparganosis: Sonographic findings. J Clin Ultrasound. 2008; 36:570–572.3. Cho JH, Lee KB, Yong TS, Kim BS, Park HB, Ryu KN, et al. Subcutaneous and musculoskeletal sparganosis: imaging characteristics and pathologic correlation. Skeletal Radiol. 2000; 29:402–408.4. Koo M, Kim JH, Kim JS, Lee JE, Nam SJ, Yang JH. Cases and literature review of breast sparganosis. World J Surg. 2011; 35:573–579.5. Chan AB, Wan SK, Leung SL, Law BK, Lai DP, Ip M, et al. Sparganosis of the breast. Histopathology. 2004; 44:510–511.6. Chang YK, Kim KC, Cho HJ. Sparganosis in the female breast. J Korean Surg Soc. 2000; 58:285–287.7. Sarukawa S, Kawanabe T, Yagasaki A, Shimizu A, Shimada S. Case of subcutaneous sparganosis: use of imaging in definitive preoperative diagnosis. J Dermatol. 2007; 34:654–657.8. Yoon HS, Jeon BJ, Park BY. Multiple sparganosis in an immunosuppressed patient. Arch Plast Surg. 2013; 40:479–481.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of the Role of Axillary Lymph Node Fine-Needle Aspiration Cytology in Early Breast Cancer With or Without Neoadjuvant Chemotherapy
- Ipsilateral Breast Tumor Recurrence with Metachronous Contralateral Axillary Lymph Node Metastasis after Breast-Conserving Surgery with Axillary Lymph Node Dissection
- Ultrasonography for Staging Axillary Lymph Node in Breast Cancer Patients
- Sentinel Lymph Node Biopsy in Breast Cancer: A Clinical Review and Update
- Metachronous Contralateral Axillary Lymph Node Metastasis from Invasive Breast Carcinoma: A Case Report with Imaging Findings