Allergy Asthma Immunol Res.
2016 Jan;8(1):32-40. 10.4168/aair.2016.8.1.32.
GIS-based Association Between PM10 and Allergic Diseases in Seoul: Implications for Health and Environmental Policy
- Affiliations
-
- 1The Environmental Health Center for Asthma, Korea University, Seoul, Korea.
- 2School of Economic, Political and Policy Sciences, the University of Texas at Dallas, Richardson, TX, United States. dohyeong.kim@utdallas.edu
- 3Duke Global Health Institute, Duke University, Durham, NC, United States.
- 4Department of Pediatrics, College of Medicine, Korea University, Seoul, Korea.
- KMID: 2166647
- DOI: http://doi.org/10.4168/aair.2016.8.1.32
Abstract
- PURPOSE
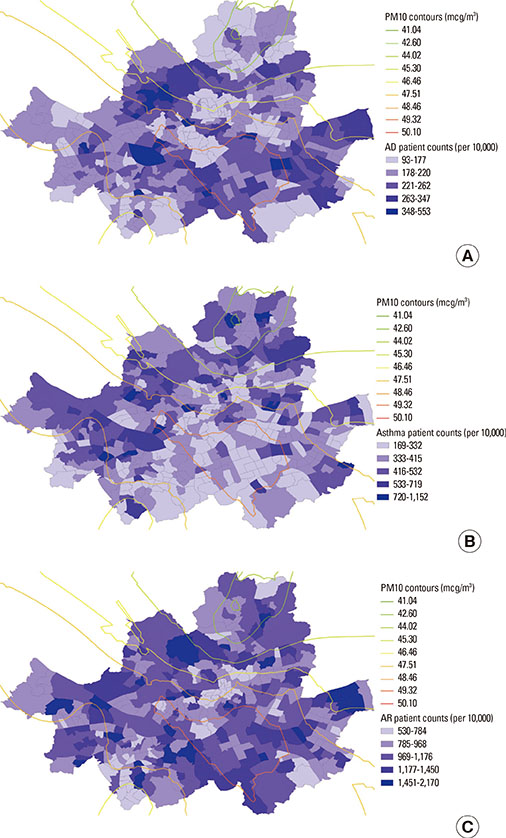
The role of PM10 in the development of allergic diseases remains controversial among epidemiological studies, partly due to the inability to control for spatial variations in large-scale risk factors. This study aims to investigate spatial correspondence between the level of PM10 and allergic diseases at the sub-district level in Seoul, Korea, in order to evaluate whether the impact of PM10 is observable and spatially varies across the subdistricts.
METHODS
PM10 measurements at 25 monitoring stations in the city were interpolated to 424 sub-districts where annual inpatient and outpatient count data for 3 types of allergic diseases (atopic dermatitis, asthma, and allergic rhinitis) were collected. We estimated multiple ordinary least square regression models to examine the association of the PM10 level with each of the allergic diseases, controlling for various sub-district level covariates. Geographically weighted regression (GWR) models were conducted to evaluate how the impact of PM10 varies across the sub-districts.
RESULTS
PM10 was found to be a significant predictor of atopic dermatitis patient count (P<0.01), with greater association when spatially interpolated at the sub-district level. No significant effect of PM10 was observed on allergic rhinitis and asthma when socioeconomic factors were controlled for. GWR models revealed spatial variation of PM10 effects on atopic dermatitis across the sub-districts in Seoul. The relationship of PM10 levels to atopic dermatitis patient counts is found to be significant only in the Gangbuk region (P<0.01), along with other covariates including average land value, poverty rate, level of education and apartment rate (P<0.01).
CONCLUSIONS
Our findings imply that PM10 effects on allergic diseases might not be consistent throughout Seoul. GIS-based spatial modeling techniques could play a role in evaluating spatial variation of air pollution impacts on allergic diseases at the sub-district level, which could provide valuable guidelines for environmental and public health policymakers.
MeSH Terms
Figure
Cited by 3 articles
-
Food deserts in Korea? A GIS analysis of food consumption patterns at sub-district level in Seoul using the KNHANES 2008-2012 data
Dohyeong Kim, Chang Kil Lee, Dong Yeon Seo
Nutr Res Pract. 2016;10(5):530-536. doi: 10.4162/nrp.2016.10.5.530.Air pollution and childhood allergic disease
Young Yoo
Allergy Asthma Respir Dis. 2016;4(4):248-256. doi: 10.4168/aard.2016.4.4.248.Effect of TiO2 Nanoparticles on Inflammasome-Mediated Airway Inflammation and Responsiveness
Byeong-Gon Kim, Pureun-Haneul Lee, Sun-Hye Lee, Moo-Kyun Park, An-Soo Jang
Allergy Asthma Immunol Res. 2017;9(3):257-264. doi: 10.4168/aair.2017.9.3.257.
Reference
-
1. Ministry of Environment (KR). Plans for the prevention and control of allergic diseases. Seoul: Ministry of Environment;2011.2. Jenerowicz D, Silny W, Dańczak-Pazdrowska A, Polańska A, Osmola-Mańkowska A, Olek-Hrab K. Environmental factors and allergic diseases. Ann Agric Environ Med. 2012; 19:475–481.3. Nickmilder M, Bernard A. Ecological association between childhood asthma and availability of indoor chlorinated swimming pools in Europe. Occup Environ Med. 2007; 64:37–46.4. Zock JP, Jarvis D, Luczynska C, Sunyer J, Burney P. European Community Respiratory Health Survey. Housing characteristics, reported mold exposure, and asthma in the European Community Respiratory Health Survey. J Allergy Clin Immunol. 2002; 110:285–292.5. Seo S, Kim D, Paul C, Yoo Y, Choung JT. Exploring household-level risk factors for self-reported prevalence of allergic diseases among low-income households in Seoul, Korea. Allergy Asthma Immunol Res. 2014; 6:421–427.6. Morgenstern V, Zutavern A, Cyrys J, Brockow I, Koletzko S, Krämer U, et al. Atopic diseases, allergic sensitization, and exposure to traffic-related air pollution in children. Am J Respir Crit Care Med. 2008; 177:1331–1337.7. Suárez-Varela MM, Gallardo-Juan A, García-Marcos L, Gimeno-Clemente N, Silvarrey-Varela ÁL, Miner-Canflanca I, et al. The impact of atmospheric pollutants on the prevalence of atopic eczema in 6-7-year-old schoolchildren in Spain; ISAAC Phase III. Iran J Allergy Asthma Immunol. 2013; 12:220–227.8. Zmirou D, Gauvin S, Pin I, Momas I, Sahraoui F, Just J, et al. Traffic related air pollution and incidence of childhood asthma: results of the Vesta case-control study. J Epidemiol Community Health. 2004; 58:18–23.9. Gauderman WJ, Avol E, Lurmann F, Kuenzli N, Gilliland F, Peters J, et al. Childhood asthma and exposure to traffic and nitrogen dioxide. Epidemiology. 2005; 16:737–743.10. Pénard-Morand C, Charpin D, Raherison C, Kopferschmitt C, Caillaud D, Lavaud F, et al. Long-term exposure to background air pollution related to respiratory and allergic health in schoolchildren. Clin Exp Allergy. 2005; 35:1279–1287.11. McConnell R, Islam T, Shankardass K, Jerrett M, Lurmann F, Gilliland F, et al. Childhood incident asthma and traffic-related air pollution at home and school. Environ Health Perspect. 2010; 118:1021–1026.12. Krämer U, Koch T, Ranft U, Ring J, Behrendt H. Traffic-related air pollution is associated with atopy in children living in urban areas. Epidemiology. 2000; 11:64–70.13. Hajat S, Haines A, Atkinson RW, Bremner SA, Anderson HR, Emberlin J. Association between air pollution and daily consultations with general practitioners for allergic rhinitis in London, United Kingdom. Am J Epidemiol. 2001; 153:704–714.14. Heinrich J, Wichmann HE. Traffic related pollutants in Europe and their effect on allergic disease. Curr Opin Allergy Clin Immunol. 2004; 4:341–348.15. Kim J, Kim EH, Oh I, Jung K, Han Y, Cheong HK, et al. Symptoms of atopic dermatitis are influenced by outdoor air pollution. J Allergy Clin Immunol. 2013; 132:495–498.e1.16. Lipsett M, Hurley S, Ostro B. Air pollution and emergency room visits for asthma in Santa Clara County, California. Environ Health Perspect. 1997; 105:216–222.17. Donaldson K, Gilmour MI, MacNee W. Asthma and PM10. Respir Res. 2000; 1:12–15.18. Lee JT, Kim H, Song H, Hong YC, Cho YS, Shin SY, et al. Air pollution and asthma among children in Seoul, Korea. Epidemiology. 2002; 13:481–484.19. Pénard-Morand C, Charpin D, Raherison C, Kopferschmitt C, Caillaud D, Lavaud F, et al. Long-term exposure to background air pollution related to respiratory and allergic health in schoolchildren. Clin Exp Allergy. 2005; 35:1279–1287.20. Oh IB, Lee JH, Sim CS, Kim Y, Yoo CI. An association between air pollution and the prevalence of allergic rhinitis in the Ulsan metropolitan region. J Environ Health Sci. 2010; 36:465–471.21. Lee YL, Shaw CK, Su HJ, Lai JS, Ko YC, Huang SL, et al. Climate, traffic-related air pollutants and allergic rhinitis prevalence in middle-school children in Taiwan. Eur Respir J. 2003; 21:964–970.22. Baek M, Jung J, Jang T, Kim S, Ko K, Kim Y. The effect of PM10 on the symptoms of allergic rhinitis during spring. Otolaryngol Head Neck Surg. 2013; 149:P257–P258.23. Lee JT, Kim H, Song H, Hong YC, Cho YS, Shin SY, et al. Air pollution and asthma among children in Seoul, Korea. Epidemiology. 2002; 13:481–484.24. Goldhagen J, Remo R, Bryant T 3rd, Wludyka P, Dailey A, Wood D, et al. The health status of southern children: a neglected regional disparity. Pediatrics. 2005; 116:e746–e753.25. Maantay J. Asthma and air pollution in the Bronx: methodological and data considerations in using GIS for environmental justice and health research. Health Place. 2007; 13:32–56.26. Ayres-Sampaio D, Teodoro AC, Sillero N, Santos C, Fonseca J, Freitas A. An investigation of the environmental determinants of asthma hospitalizations: an applied spatial approach. Appl Geogr. 2014; 47:10–19.27. Akçakaya N, Kulak K, Hassanzadeh A, Camcioğlu Y, Cokuğraş H. Prevalence of bronchial asthma and allergic rhinitis in Istanbul school children. Eur J Epidemiol. 2000; 16:693–699.28. Byun H, Bae H, Kim D, Shin H, Yoon C. Effects of socioeconomic factors and human activities on children's PM(10) exposure in inner-city households in Korea. Int Arch Occup Environ Health. 2010; 83:867–878.29. Lee JT, Son JY, Kim H, Kim SY. Effect of air pollution on asthma-related hospital admissions for children by socioeconomic status associated with area of residence. Arch Environ Occup Health. 2006; 61:123–130.30. Bergmann RL, Edenharter G, Bergmann KE, Lau S, Wahn U. Socioeconomic status is a risk factor for allergy in parents but not in their children. Clin Exp Allergy. 2000; 30:1740–1745.31. Statistics Korea. Korean standard classification of diseases [Internet]. Daejeon: Statistics Korea;2011. cited 2015 Apr 28. Available from: http://kostat.go.kr/kssc/main/MainAction.do?method=sub&catgrp=ekssc&catid1=ekssc03.32. Hwang SH, Jung SY, Lim DH, Son BK, Kim JH, Yang JM, et al. Epidemiology of allergic rhinitis in Korean children. Allergy Asthma Respir Dis. 2013; 1:321–332.33. McLean I, McMillan A. The concise Oxford dictionary of politics. 3rd ed. New York (NY): Oxford University Press;2009.34. Plummer M, Clayton D. Estimation of population exposure in ecological studies. J R Stat Soc Series B Methodol. 1996; 58:113–126.35. Connor MJ, Gillings D. An empiric study of ecological inference. Am J Public Health. 1984; 74:555–559.36. Piantadosi S, Byar DP, Green SB. The ecological fallacy. Am J Epidemiol. 1988; 127:893–904.37. Guthrie KA, Sheppard L. Overcoming biases and misconceptions in ecological studies. J R Stat Soc Ser A Stat Soc. 2001; 164:141–154.38. Lasserre V, Guihenneuc-Jouyaux C, Richardson S. Biases in ecological studies: utility of including within-area distribution of confounders. Stat Med. 2000; 19:45–59.39. Breslin FC, Smith P, Dunn JR. An ecological study of regional variation in work injuries among young workers. BMC Public Health. 2007; 7:91.40. Rezaeian M, Dunn G, St Leger S, Appleby L. Ecological association between suicide rates and indices of deprivation in the north west region of England: the importance of the size of the administrative unit. J Epidemiol Community Health. 2006; 60:956–961.41. Joseph J, Sharif HO, Sunil T, Alamgir H. Application of validation data for assessing spatial interpolation methods for 8-h ozone or other sparsely monitored constituents. Environ Pollut. 2013; 178:411–418.42. Son JY, Bell ML, Lee JT. Individual exposure to air pollution and lung function in Korea: spatial analysis using multiple exposure approaches. Environ Res. 2010; 110:739–749.43. Liao D, Peuquet DJ, Duan Y, Whitsel EA, Dou J, Smith RL, et al. GIS approaches for the estimation of residential-level ambient PM concentrations. Environ Health Perspect. 2006; 114:1374–1380.44. Cummins S, Clary C, Lewis D, Flint E, Smith N, Kestens Y. PP39 Relative versus absolute measures of the neighbourhood food environment and diet in the ORiEL Study: a geographically weighted regression approach. J Epidemiol Community Health. 2014; 68:A63.45. Yang TC, Matthews SA. Understanding the non-stationary associations between distrust of the health care system, health conditions, and self-rated health in the elderly: a geographically weighted regression approach. Health Place. 2012; 18:576–585.46. Carrel M, Escamilla V, Messina J, Giebultowicz S, Winston J, Yunus M, et al. Diarrheal disease risk in rural Bangladesh decreases as tubewell density increases: a zero-inflated and geographically weighted analysis. Int J Health Geogr. 2011; 10:41.47. Ali K, Partridge MD, Olfert MR. Can geographically weighted regressions improve regional analysis and policy making? Int Reg Sci Rev. 2007; 30:300–329.48. Shim E, Yu J. Relationship between duration of disease and bronchial responsiveness in 6-8 years old children with asthma. Allergy Asthma Respir Dis. 2014; 2:23–29.49. Park HB, Kim YH, Kim MJ, Kim HS, Lee HS, Han YK, et al. Forced expiratory flow between 25% and 75% of vital capacity as a predictor for bronchial hyperresponsiveness in children with allergic rhinitis. Allergy Asthma Respir Dis. 2013; 1:60–66.50. Kim HS, Jung JI, Suh SB, Jung JA. Characteristics between IgE mediated and non-IgE mediated atopic dermatitis in children. Allergy Asthma Respir Dis. 2013; 1:339–343.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship Between Air Pollutants and Prevalence of Allergic Disease/Pulmonary Function in Students in Incheon
- Genetic studies of allergic disease and their clinical implications
- Health Promotion and Prevention of Allergic Disease
- Spatial analysis of PM10 and cardiovascular mortality in the Seoul metropolitan area
- Environmental Health Surveillance of Low Birth Weight in Seoul using Air Monitoring and Birth Data