Ann Rehabil Med.
2014 Jun;38(3):317-326. 10.5535/arm.2014.38.3.317.
Ultrasonographic Measurement of Transverse Abdominis in Stroke Patients
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. amaro-te@hanmail.net
- KMID: 2165748
- DOI: http://doi.org/10.5535/arm.2014.38.3.317
Abstract
OBJECTIVE
To compare transverse abdominis (TrA) contractility in stroke patients with hemiparesis and healthy adults using musculoskeletal ultrasonography.
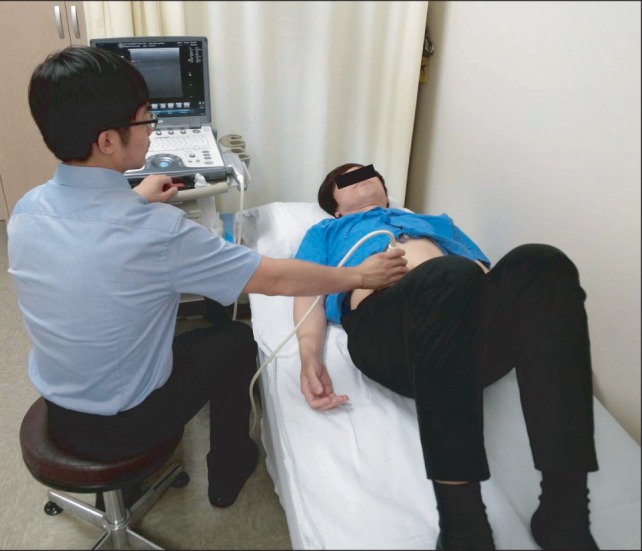
METHODS
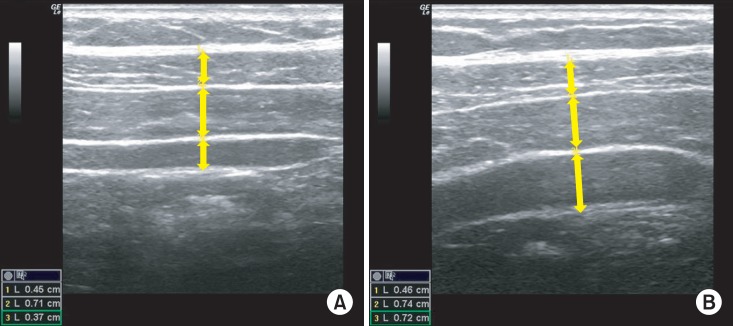
Forty-seven stroke patients with hemiparesis and 25 age-matched healthy control subjects participated in this study. Stroke patients were divided into three groups on the basis of their degree of ambulation. Group A consisted of 9 patients with wheelchair ambulation, group B of 23 patients with assisted ambulation, and group C of 15 patients with independent ambulation. Inter-rater reliability regarding ultrasonographic measurement of abdominal muscle thickness in the control group was assessed by two examiners. The TrA contraction ratio (TrA contracted thickness/TrA resting thickness) was measured during abdominal drawing-in maneuver and was compared between the patients and the control group and between the ambulation groups.
RESULTS
The inter-rater reliability ranged from 0.900 to 0.947. The TrA contraction ratio was higher in the non-paretic side than in the paretic side (1.40+/-0.62 vs. 1.14+/-0.35, p<0.01). The TrA contraction ratio of the patient group was lower in the non-paretic side as well as in the paretic side than that of the control group (right 1.85+/-0.29, left 1.92+/-0.42; p<0.001). No difference was found between the ambulation regarding the TrA contraction ratio.
CONCLUSION
The TrA contractility in hemiparetic stroke patients is significantly decreased in the non-paretic side as well as in the paretic side compared with that of healthy adults. Ultrasonographic measurement can be clinically used in the evaluation of deep abdominal muscles in stroke patients.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Muscle Thickness and Echo Intensity of the Abdominal and Lower Extremity Muscles in Stroke Survivors
Hiroki Monjo, Yoshihiro Fukumoto, Tsuyoshi Asai, Hisato Shuntoh
J Clin Neurol. 2018;14(4):549-554. doi: 10.3988/jcn.2018.14.4.549.Ultrasound Imaging of the Trunk Muscles in Acute Stroke Patients and Relations With Balance Scales
Yunho Kim, Jeeyoung Kim, Heesung Nam, Hyun Dong Kim, Mi Ja Eom, Sang Hoon Jung, Nami Han
Ann Rehabil Med. 2020;44(4):273-283. doi: 10.5535/arm.19125.
Reference
-
1. Hodges PW, Cresswell AG, Daggfeldt K, Thorstensson A. In vivo measurement of the effect of intraabdominal pressure on the human spine. J Biomech. 2001; 34:347–353. PMID: 11182126.
Article2. Hodges PW, Richardson CA. Feedforward contraction of transversus abdominis is not influenced by the direction of arm movement. Exp Brain Res. 1997; 114:362–370. PMID: 9166925.
Article3. Hodges P, Kaigle Holm A, Holm S, Ekstrom L, Cresswell A, Hansson T, et al. Intervertebral stiffness of the spine is increased by evoked contraction of transversus abdominis and the diaphragm: in vivo porcine studies. Spine (Phila Pa 1976). 2003; 28:2594–2601. PMID: 14652476.
Article4. Saliba SA, Croy T, Guthrie R, Grooms D, Weltman A, Grindstaff TL. Differences in transverse abdominis activation with stable and unstable bridging exercises in individuals with low back pain. N Am J Sports Phys Ther. 2010; 5:63–73. PMID: 21589663.5. Critchley DJ, Coutts FJ. Abdominal muscle function in chronic low back pain patients: measurement with real-time ultrasound scanning. Physiotherapy. 2002; 88:322–332.6. Ferreira PH, Ferreira ML, Hodges PW. Changes in recruitment of the abdominal muscles in people with low back pain: ultrasound measurement of muscle activity. Spine (Phila Pa 1976). 2004; 29:2560–2566. PMID: 15543074.7. Ferreira PH, Ferreira ML, Maher CG, Refshauge K, Herbert RD, Hodges PW. Changes in recruitment of transversus abdominis correlate with disability in people with chronic low back pain. Br J Sports Med. 2010; 44:1166–1172. PMID: 19474006.
Article8. Tanaka S, Hachisuka K, Ogata H. Muscle strength of trunk flexion-extension in post-stroke hemiplegic patients. Am J Phys Med Rehabil. 1998; 77:288–290. PMID: 9715916.9. Karatas M, Cetin N, Bayramoglu M, Dilek A. Trunk muscle strength in relation to balance and functional disability in unihemispheric stroke patients. Am J Phys Med Rehabil. 2004; 83:81–87. PMID: 14758293.
Article10. Dickstein R, Shefi S, Marcovitz E, Villa Y. Anticipatory postural adjustment in selected trunk muscles in post stroke hemiparetic patients. Arch Phys Med Rehabil. 2004; 85:261–267. PMID: 14966711.11. Juneja G, Czyrny JJ, Linn RT. Admission balance and outcomes of patients admitted for acute inpatient rehabilitation. Am J Phys Med Rehabil. 1998; 77:388–393. PMID: 9798829.12. Hsieh CL, Sheu CF, Hsueh IP, Wang CH. Trunk control as an early predictor of comprehensive activities of daily living function in stroke patients. Stroke. 2002; 33:2626–2630. PMID: 12411652.
Article13. Bohannon RW, Leary KM. Standing balance and function over the course of acute rehabilitation. Arch Phys Med Rehabil. 1995; 76:994–996. PMID: 7487452.
Article14. Sandin KJ, Smith BS. The measure of balance in sitting in stroke rehabilitation prognosis. Stroke. 1990; 21:82–86. PMID: 2300995.
Article15. Lee YJ, Lee GW, Yi CH, Cynn HS. Comparison of abdominal muscle thickness between the nonparetic and paretic side during quiet breathing in patients with chronic. J Korean Acad Univ Trained Phys Ther. 2011; 18:8–15.16. Park HJ, Oh DW, Shin WS. The study of asymmetrical contraction of the lateral abdominal muscles in stroke patients using ultrasound imaging. J Korean Soc Phys Med. 2012; 7:319–327.
Article17. Hodges PW, Pengel LH, Herbert RD, Gandevia SC. Measurement of muscle contraction with ultrasound imaging. Muscle Nerve. 2003; 27:682–692. PMID: 12766979.
Article18. McMeeken JM, Beith ID, Newham DJ, Milligan P, Critchley DJ. The relationship between EMG and change in thickness of transversus abdominis. Clin Biomech (Bristol, Avon). 2004; 19:337–342.
Article19. English CK, Thoirs KA, Fisher L, McLennan H, Bernhardt J. Ultrasound is a reliable measure of muscle thickness in acute stroke patients, for some, but not all anatomical sites: a study of the intra-rater reliability of muscle thickness measures in acute stroke patients. Ultrasound Med Biol. 2012; 38:368–376. PMID: 22266233.
Article20. Vasseljen O, Fladmark AM. Abdominal muscle contraction thickness and function after specific and general exercises: a randomized controlled trial in chronic low back pain patients. Man Ther. 2010; 15:482–489. PMID: 20621545.
Article21. Teyhen DS, Miltenberger CE, Deiters HM, Del Toro YM, Pulliam JN, Childs JD, et al. The use of ultrasound imaging of the abdominal drawing-in maneuver in subjects with low back pain. J Orthop Sports Phys Ther. 2005; 35:346–355. PMID: 16001906.
Article22. Ferreira PH, Ferreira ML, Nascimento DP, Pinto RZ, Franco MR, Hodges PW. Discriminative and reliability analyses of ultrasound measurement of abdominal muscles recruitment. Man Ther. 2011; 16:463–469. PMID: 21398167.
Article23. Goldman JM, Lehr RP, Millar AB, Silver JR. An electromyographic study of the abdominal muscles during postural and respiratory manoeuvres. J Neurol Neurosurg Psychiatry. 1987; 50:866–869. PMID: 2957469.
Article24. Urquhart DM, Hodges PW, Allen TJ, Story IH. Abdominal muscle recruitment during a range of voluntary exercises. Man Ther. 2005; 10:144–153. PMID: 15922235.
Article25. Strohl KP, Mead J, Banzett RB, Loring SH, Kosch PC. Regional differences in abdominal muscle activity during various maneuvers in humans. J Appl Physiol Respir Environ Exerc Physiol. 1981; 51:1471–1476. PMID: 6459311.
Article26. De Troyer A, Estenne M, Ninane V, Van Gansbeke D, Gorini M. Transversus abdominis muscle function in humans. J Appl Physiol (1985). 1990; 68:1010–1016. PMID: 2140344.
Article27. Teyhen DS, Rieger JL, Westrick RB, Miller AC, Molloy JM, Childs JD. Changes in deep abdominal muscle thickness during common trunk-strengthening exercises using ultrasound imaging. J Orthop Sports Phys Ther. 2008; 38:596–605. PMID: 18827329.
Article28. Bohannon RW, Cassidy D, Walsh S. Trunk muscle strength is impaired multidirectionally after stroke. Clin Rehabil. 1995; 9:47–51.
Article29. Tanaka S, Hachisuka K, Ogata H. Trunk rotatory muscle performance in post-stroke hemiplegic patients. Am J Phys Med Rehabil. 1997; 76:366–369. PMID: 9354489.30. Kuypers HG, Brinkman J. Precentral projections to different parts of the spinal intermediate zone in therhesus monkey. Brain Res. 1970; 24:29–48. PMID: 4099987.31. Carr LJ, Harrison LM, Stephens JA. Evidence for bilateral innervation of certain homologous motoneurone pools in man. J Physiol. 1994; 475:217–227. PMID: 8021829.
Article32. Muller F, Kunesch E, Binkofski F, Freund HJ. Residual sensorimotor functions in a patient after right-sided hemispherectomy. Neuropsychologia. 1991; 29:125–145. PMID: 1902915.
Article33. Hides JA, Richardson CA, Jull GA. Magnetic resonance imaging and ultrasonography of the lumbar multifidus muscle Comparison of two different modalities. Spine (Phila Pa 1976). 1995; 20:54–58. PMID: 7709280.34. Gwowdon JH, Fink JS. Paralysis and movement disorders. Harrison TR, Wilson JD, Isselbacher KJ. Harrison's principles of internal medicine. 12th ed. New York: McGraw-Hill;1991. p. 157–169.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Breast Reconstruction with Free Transverse Rectus Abdominis Myocutaneous Flap Complicated by Deep Vein Thrombosis-associated Pulmonary Thrombo-embolism
- Effect of Horse Riding Simulator Exercise on Thickness of Transverse Abdominis in Healthy Adults
- Ultrasound Imaging of the Trunk Muscles in Acute Stroke Patients and Relations With Balance Scales
- Functional & anatomic reconstruction of the donor site after the transverse rectus abdominis myocutaneous(TRAM) flap transfer
- Breast reconstruction using pedicled transverse rectus abdominis musculocutaneous (TRAM) flap