Ann Rehabil Med.
2014 Aug;38(4):568-574. 10.5535/arm.2014.38.4.568.
Medical Management for Intractable Pain Arising From Primary Sjogren Syndrome Involving Both Brain and Spinal Cord: A Case Report
- Affiliations
-
- 1Department of Rehabilitation Medicine, Chungbuk National University College of Medicine, Cheongju, Korea. pum78@naver.com
- KMID: 2165742
- DOI: http://doi.org/10.5535/arm.2014.38.4.568
Abstract
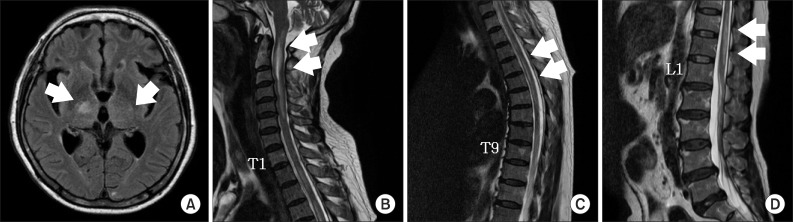
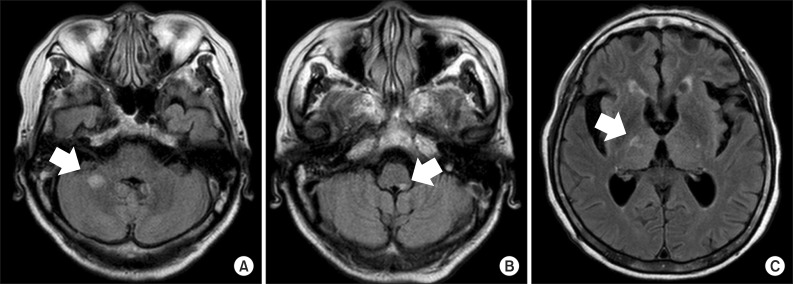
- Primary Sjogren syndrome, which involves lesions in both the brain and spinal cord, is rarely reported. Related symptoms, such as intractable pain due to central nervous system involvement, are very rare. A 73-year-old woman diagnosed with primary Sjogren syndrome manifested with subacute encephalopathy and extensive transverse myelitis. She complained of severe whole body neuropathic pain. Magnetic resonance imaging demonstrated a non-enhancing ill-defined high intensity signal involving the posterior limb of the both internal capsule and right thalamus on a T2 fluid-attenuated inversion recovery image. Additionally, multifocal intramedullary ill-defined contrast-enhancing lesion with cord swelling from the C-spine to L-spine was also visible on the T2-weighted image. Her intractable pain remarkably improved after administration of concomitant oral doses of gabapentin, venlafaxine, and carbamazepine.
MeSH Terms
Figure
Reference
-
1. Govoni M, Padovan M, Rizzo N, Trotta F. CNS involvement in primary Sjögren's syndrome: prevalence, clinical aspects, diagnostic assessment and therapeutic approach. CNS Drugs. 2001; 15:597–607. PMID: 11524032.2. Choi HJ, Shin K, Kang EH, Im CH, Lee YJ, Lee EB, et al. Primary Sjögren's syndrome presenting as acute transverse myelitis. Korean J Med. 2005; 68:463–466.3. Kim HA, Ma EJ, Lee J, Ha CK. The Primary Sjögren's syndrome involving central and peripheral nervous system. J Korean Neurol Assoc. 2007; 25:108–111.4. Tennant F, Hermann L. Intractable or chronic pain: there is a difference. West J Med. 2000; 173:306. PMID: 11069861.
Article5. Dworkin RH, O'Connor AB, Backonja M, Farrar JT, Finnerup NB, Jensen TS, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain. 2007; 132:237–251. PMID: 17920770.
Article6. Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, et al. Classification criteria for Sjögren's syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis. 2002; 61:554–558. PMID: 12006334.7. Delalande S, de Seze J, Fauchais AL, Hachulla E, Stojkovic T, Ferriby D, et al. Neurologic manifestations in primary Sjögren syndrome: a study of 82 patients. Medicine (Baltimore). 2004; 83:280–291. PMID: 15342972.8. Finnerup NB, Otto M, McQuay HJ, Jensen TS, Sindrup SH. Algorithm for neuropathic pain treatment: an evidence based proposal. Pain. 2005; 118:289–305. PMID: 16213659.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- High-Level Cervical Spinal Cord Stimulation Used to Treat Intractable Pain Arising from Transverse Myelitis Caused by Schistosomiasis
- Experience of Right Leg Pain Control by Left Epidural Space Inserted Spinal Cord Stimulator: A case report
- Spinal Cauda Equina Stimulation for Alternative Location of Spinal Cord Stimulation in Intractable Phantom Limb Pain Syndrome: A Case Report
- Spinal cord stimulation for intractable post-thoracotomy pain syndrome: A case report
- A Case of Primary Sjogren's Syndrome Associated with Acute Transverse Myelitis