J Bone Metab.
2016 May;23(2):63-77. 10.11005/jbm.2016.23.2.63.
Cost-effectiveness of Pharmaceutical Interventions to Prevent Osteoporotic Fractures in Postmenopausal Women with Osteopenia
- Affiliations
-
- 1College of Pharmacy and Research, Institute of Pharmaceutical Sciences, Kyungpook National University, Daegu, Korea.
- 2College of Pharmacy, Yonsei Institute of Pharmaceutical Sciences, Yonsei University, Seoul, Korea. hykang2@yonsei.ac.kr
- 3Department of Orthopaedic Surgery, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2165120
- DOI: http://doi.org/10.11005/jbm.2016.23.2.63
Abstract
- BACKGROUND
To assess the cost-effectiveness of drug therapy to prevent osteoporotic fractures in postmenopausal women with osteopenia in Korea.
METHODS
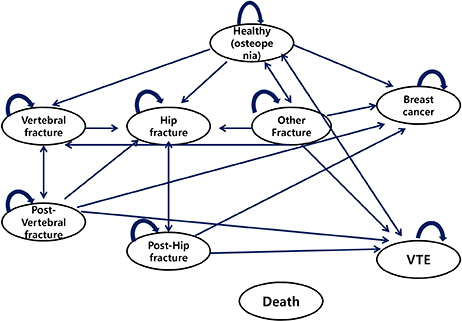
A Markov cohort simulation was conducted for lifetime with a hypothetical cohort of postmenopausal women with osteopenia and without prior fractures. They were assumed to receive calcium/vitamin D supplements only or drug therapy (i.e., raloxifene or risedronate) along with calcium/vitamin D for 5 years. The Markov model includes fracture-specific and non-fracture specific health states (i.e. breast cancer and venous thromboembolism), and all-cause death. Published literature was used to determine the model parameters. Local data were used to estimate the baseline incidence rates of fracture in those with osteopenia and the costs associated with each health state.
RESULTS
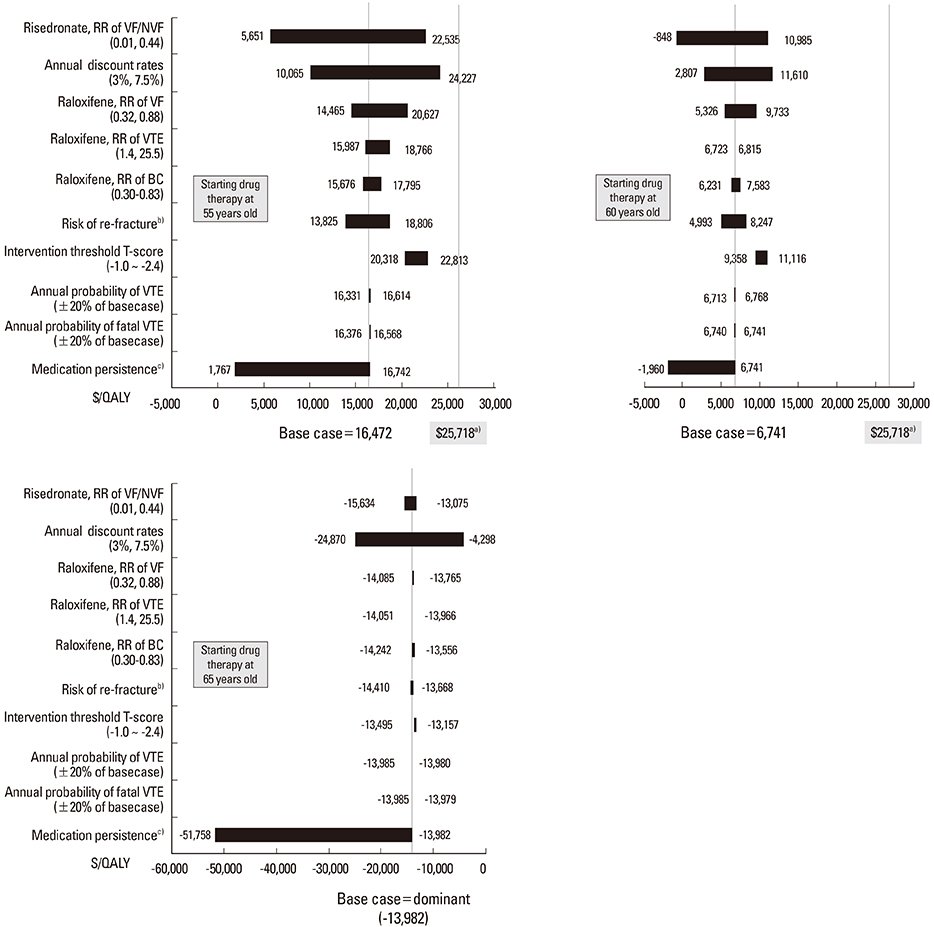
From a societal perspective, the estimated incremental cost-effectiveness ratios (ICERs) for the base cases that had T-scores between -2.0 and -2.4 and began drug therapy at the age of 55, 60, or 65 years were $16,472, $6,741, and -$13,982 per quality-adjusted life year (QALY) gained, respectively. Sensitivity analyses for medication compliance, risk of death following vertebral fracture, and relaxing definition of osteopenia resulted in ICERs reached to $24,227 per QALY gained.
CONCLUSIONS
ICERs for the base case and sensitivity analyses remained within the World Health Organization's willingness-to-pay threshold, which is less than per-capita gross domestic product in Korea (about $25,700). Thus, we conclude that drug therapy for osteopenia would be a cost-effective intervention, and we recommend that the Korean National Health Insurance expand its coverage to include drug therapy for osteopenia.
Keyword
MeSH Terms
-
Bone Diseases, Metabolic*
Breast Neoplasms
Cohort Studies
Cost-Benefit Analysis
Drug Therapy
Female
Global Health
Gross Domestic Product
Humans
Incidence
Korea
Medication Adherence
National Health Programs
Osteoporotic Fractures*
Postmenopause
Quality-Adjusted Life Years
Raloxifene Hydrochloride
Risedronate Sodium
Raloxifene Hydrochloride
Risedronate Sodium
Figure
Cited by 1 articles
-
Estimating the Fiscal Costs of Osteoporosis in Korea Applying a Public Economic Perspective
Mark P. Connolly, Saswat Panda, Ha Young Kim
J Bone Metab. 2019;26(4):253-261. doi: 10.11005/jbm.2019.26.4.253.
Reference
-
1. World Health Organization. Prevention and management of osteoporosis. 2003. cited by 2015 August 3. Available from: http://apps.who.int/iris/bitstream/10665/42841/1/WHO_TRS_921.pdf.2. Looker AC, Orwoll ES, Johnston CC Jr, et al. Prevalence of low femoral bone density in older U.S. adults from NHANES III. J Bone Miner Res. 1997; 12:1761–1768.
Article3. National Evidence-based Healthcare Collaborating Agency. Developing Korea-specific assessment criteria for osteoporosis. Seoul: National Evidence-based Healthcare Collaborating Agency;2011.4. Siris ES, Simon JA, Barton IP, et al. Effects of risedronate on fracture risk in postmenopausal women with osteopenia. Osteoporos Int. 2008; 19:681–686.
Article5. Siris ES, Miller PD, Barrett-Connor E, et al. Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment. JAMA. 2001; 286:2815–2822.
Article6. Schuit SC, van der Klift M, Weel AE, et al. Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam study. Bone. 2004; 34:195–202.
Article7. Lee JH, Lee YH, Moon SH. Association between bone mineral density and clinical consequences: cross-sectional study of Korean postmenopausal women in an orthopaedic outpatient clinic. J Korean Med Sci. 2014; 29:1152–1160.
Article8. Pasco JA, Seeman E, Henry MJ, et al. The population burden of fractures originates in women with osteopenia, not osteoporosis. Osteoporos Int. 2006; 17:1404–1409.
Article9. Siris ES, Chen YT, Abbott TA, et al. Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med. 2004; 164:1108–1112.
Article10. Kanis JA, Johnell O, Black DM, et al. Effect of raloxifene on the risk of new vertebral fracture in postmenopausal women with osteopenia or osteoporosis: a reanalysis of the Multiple Outcomes of Raloxifene Evaluation trial. Bone. 2003; 33:293–300.
Article11. Jolly EE, Bjarnason NH, Neven P, et al. Prevention of osteoporosis and uterine effects in postmenopausal women taking raloxifene for 5 years. Menopause. 2003; 10:337–344.
Article12. Ivergård M, Strom O, Borgström F, et al. Identifying cost-effective treatment with raloxifene in postmenopausal women using risk algorithms for fractures and invasive breast cancer. Bone. 2010; 47:966–974.
Article13. Kanis JA, Borgström F, Johnell O, et al. Cost-effectiveness of raloxifene in the UK: an economic evaluation based on the MORE study. Osteoporos Int. 2005; 16:15–25.
Article14. Wasserfallen JB, Krieg MA, Greiner RA, et al. Cost effectiveness and cost utility of risedronate for osteoporosis treatment and fracture prevention in women: a Swiss perspective. J Med Econ. 2008; 11:499–523.
Article15. Zethraeus N, Borgström F, Ström O, et al. Cost-effectiveness of the treatment and prevention of osteoporosis--a review of the literature and a reference model. Osteoporos Int. 2007; 18:9–23.
Article16. Kanis JA, Dawson A, Oden A, et al. Cost-effectiveness of preventing hip fracture in the general female population. Osteoporos Int. 2001; 12:356–361.
Article17. Borgström F, Johnell O, Kanis JA, et al. Cost effectiveness of raloxifene in the treatment of osteoporosis in Sweden: an economic evaluation based on the MORE study. Pharmacoeconomics. 2004; 22:1153–1165.
Article18. Kang HY, Yang KH, Kim YN, et al. Incidence and mortality of hip fracture among the elderly population in South Korea: a population-based study using the national health insurance claims data. BMC Public Health. 2010; 10:230.
Article19. Meadows ES, Klein R, Rousculp MD, et al. Cost-effectiveness of preventative therapies for postmenopausal women with osteopenia. BMC Womens Health. 2007; 7:6.
Article20. Klotzbuecher CM, Ross PD, Landsman PB, et al. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000; 15:721–739.
Article21. The Korea Central Cancer Registry, National Cancer Center. Annual report of cancer statistics in Korea in 2010. Sejong: Ministry of Health and Welfare;2012.22. Korean Breast Cancer Society. 2006-2008 Breast cancer facts & figures. 2008. cited by 2015 August 3. Available from: http://www.kbcs.or.kr/journal/file/2006_2008_Breast_Cancer_Facts_and_Figures_updated.pdf.23. Korean Breast Cancer Society. 2012 Breast cancer facts & figures. 2012. cited by 2015 August 3. Available from: http://www.kbcs.or.kr/journal/file/2012.pdf.24. Martino S, Cauley JA, Barrett-Connor E, et al. Continuing outcomes relevant to Evista: breast cancer incidence in postmenopausal osteoporotic women in a randomized trial of raloxifene. J Natl Cancer Inst. 2004; 96:1751–1761.
Article25. Grady D, Ettinger B, Moscarelli E, et al. Safety and adverse effects associated with raloxifene: multiple outcomes of raloxifene evaluation. Obstet Gynecol. 2004; 104:837–844.
Article26. Weycker D, Macarios D, Edelsberg J, et al. Compliance with drug therapy for postmenopausal osteoporosis. Osteoporos Int. 2006; 17:1645–1652.
Article27. Yoon SP, Lee SH, Ki CH, et al. Quality of life in patients with osteoporotic vertebral fractures. Asian Spine J. 2014; 8:653–658.
Article28. Kim JK, Kang JS. Evaluation of the Korean version of the patient-rated wrist evaluation. J Hand Ther. 2013; 26:238–243. quiz 44.
Article29. Guillemin F, Martinez L, Calvert M, et al. Fear of falling, fracture history, and comorbidities are associated with health-related quality of life among European and US women with osteoporosis in a large international study. Osteoporos Int. 2013; 24:3001–3010.
Article30. Korean Society for Bone and Mineral Research. Physician's guide for diagnosis & treatment of osteoporosis. Seoul: Korean Society for Bone and Mineral Research;2013.31. Kang HY, Park SE, Kang DR, et al. Estimating medical expenditure associated with osteoporotic hip fracture in elderly Korean women based on the National Health Insurance Claims Database 2002-2004. Value Health. 2009; 12:Suppl 3. S93–S96.
Article32. Health Insurance Review and Assessment Service. Cost estimation from diagnosis to death of cancer patients. Wonju: Health Insurance Review and Assessment Service;2010.33. Ministry for Health WaFA. Medical service utilization and cost among Korean elderly in the period of last twelve months of life. Seoul: Ministry for Health, Welfare and Family Affairs;2001.34. World Health Organization. Cost effectiveness and strategic planning (WHO-CHOICE). 2015. cited by 2015 August 3. Available from: http://www.who.int/choice/costs/CER_levels/en/.35. Müller D, Pulm J, Gandjour A. Cost-effectiveness of different strategies for selecting and treating individuals at increased risk of osteoporosis or osteopenia: a systematic review. Value Health. 2012; 15:284–298.
Article36. Schwenkglenks M, Lippuner K. Simulation-based cost-utility analysis of population screening-based alendronate use in Switzerland. Osteoporos Int. 2007; 18:1481–1491.
Article37. Schousboe JT, Bauer DC, Nyman JA, et al. Potential for bone turnover markers to cost-effectively identify and select post-menopausal osteopenic women at high risk of fracture for bisphosphonate therapy. Osteoporos Int. 2007; 18:201–210.
Article38. Schousboe JT, Ensrud KE, Nyman JA, et al. Cost-effectiveness of vertebral fracture assessment to detect prevalent vertebral deformity and select postmenopausal women with a femoral neck T-score>-2.5 for alendronate therapy: a modeling study. J Clin Densitom. 2006; 9:133–143.
Article39. Eisman JA, Bogoch ER, Dell R, et al. Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res. 2012; 27:2039–2046.
Article40. Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985; 14:32–38.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Osteopenia: When, How Long and Whom to Treat?
- Cost-Effectiveness of Denosumab for the Treatment of Postmenopausal Osteoporosis in South Korea
- Trabecular bone score as an additional therapeutic decision tool in osteoporosis and osteopenia
- Osteoporosis and Osteoporotic Fractures in Gastrointestinal Disease
- The Efficacy of Selective Estrogen Receptor Modulators Monotherapies in Postmenopausal Women with Osteopenia