J Korean Med Sci.
2015 Aug;30(8):1078-1084. 10.3346/jkms.2015.30.8.1078.
Prevalence of Atrial Fibrillation and Relation to Echocardiographic Parameters in a Healthy Asymptomatic Rural Korean Population
- Affiliations
-
- 1Department of Cardiology, Hanyang University Guri Hospital, Guri city, Korea.
- 2Department of Cardiology, Hanyang University Seoul Hospital, Seoul, Korea. jhs2003@hanyang.ac.kr
- 3Department of Preventive Medicine, College of Medicine, Hanyang University, Seoul, Korea.
- KMID: 2164502
- DOI: http://doi.org/10.3346/jkms.2015.30.8.1078
Abstract
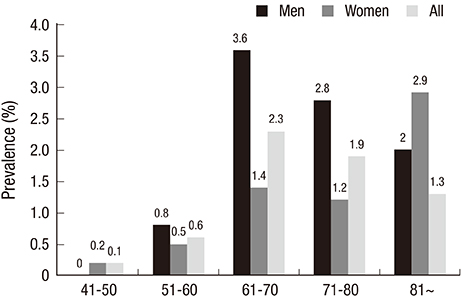
- Atrial fibrillation (AF) is the most common arrhythmia worldwide and a potent independent risk factor for stroke. This study aimed to determine the prevalence of AF in a population-based sample of adults in a rural region of Korea. Between January 2005 and December 2009, 4,067 individuals (60.2 +/- 11.2 yr old, M: F = 1,582:2,485) over 21 who were residents of the county of Yangpyeong, Korea, participated in the study. AF was assessed on a resting 12-lead electrocardiogram (ECG) in 4,053 of the participants. Blood tests and transthoracic echocardiography (TTE) were also performed to investigate the relationship between left ventricular mass and AF in the study group. Fifty-four cases (32 men) were diagnosed as AF among the 4,053 subjects. The crude prevalence of AF was 1.3%. It was highest (2.3%) among sixty- and seventy- year olds, and higher in men than women in all age groups over 50. The prevalence in men was 2.0%, and in women 0.9%. In univariate analysis, age, male gender, body mass index, total serum cholesterol, alanine transaminase, serum creatinine, adiponectin level, and ischemic heart disease were associated with AF. Among the TTE parameters, systolic and diastolic left ventricular systolic internal dimension (LVID), and LV ejection fraction were associated with AF. In this relatively healthy population in a rural area of Korea, the prevalence of AF is 1.3%, and increases with age. Of the TTE parameters, systolic and diastolic LVID and left atrial diameter are related to prevalence of AF.
Keyword
MeSH Terms
-
Adult
Age Distribution
Aged
Aged, 80 and over
Asymptomatic Diseases/*epidemiology
Atrial Fibrillation/*epidemiology/*ultrasonography
Causality
Comorbidity
Echocardiography/*statistics & numerical data
Female
Humans
Male
Middle Aged
Prevalence
Reproducibility of Results
Republic of Korea/epidemiology
Risk Factors
Rural Population/*statistics & numerical data
Sensitivity and Specificity
Sex Distribution
Stroke/*epidemiology/ultrasonography
Stroke Volume
Figure
Cited by 1 articles
-
Is Right Atrial Remodeling an Additional Marker for the Progression of Atrial Fibrillation?
Jin-Kyu Park
Korean Circ J. 2023;53(5):344-346. doi: 10.4070/kcj.2023.0069.
Reference
-
1. Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, Seward JB, Tsang TS. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006; 114:119–125.2. Stefansdottir H, Aspelund T, Gudnason V, Arnar DO. Trends in the incidence and prevalence of atrial fibrillation in Iceland and future projections. Europace. 2011; 13:1110–1117.3. Majeed A, Moser K, Carroll K. Trends in the prevalence and management of atrial fibrillation in general practice in England and Wales, 1994-1998: analysis of data from the general practice research database. Heart. 2001; 86:284–288.4. Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001; 285:2370–2375.5. Ohsawa M, Okayama A, Sakata K, Kato K, Itai K, Onoda T, Ueshima H. Rapid increase in estimated number of persons with atrial fibrillation in Japan: an analysis from national surveys on cardiovascular diseases in 1980, 1990 and 2000. J Epidemiol. 2005; 15:194–196.6. Yap KB, Ng TP, Ong HY. Low prevalence of atrial fibrillation in community-dwelling Chinese aged 55 years or older in Singapore: a population-based study. J Electrocardiol. 2008; 41:94–98.7. Jeong JH. Prevalence of and risk factors for atrial fibrillation in Korean adults older than 40 years. J Korean Med Sci. 2005; 20:26–30.8. Lim YH, Kim YM, Shin J, Lee CH, Kim JH, Kim MK, Choi BY. Association of heart rate and left ventricular structure in a rural population in Korea. Clin Exp Hypertens. 2014; 36:165–172.9. Nicol MB, Thrift AG. Knowledge of risk factors and warning signs of stroke. Vasc Health Risk Manag. 2005; 1:137–147.10. Schnabel RB, Wilde S, Wild PS, Munzel T, Blankenberg S. Atrial fibrillation: its prevalence and risk factor profile in the German general population. Dtsch Arztebl Int. 2012; 109:293–299.11. Murphy NF, Simpson CR, Jhund PS, Stewart S, Kirkpatrick M, Chalmers J, MacIntyre K, McMurray JJ. A national survey of the prevalence, incidence, primary care burden and treatment of atrial fibrillation in Scotland. Heart. 2007; 93:606–612.12. Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, Stricker BH, Stijnen T, Lip GY, Witteman JC. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J. 2006; 27:949–953.13. Langenberg M, Hellemons BS, van Ree JW, Vermeer F, Lodder J, Schouten HJ, Knottnerus JA. Atrial fibrillation in elderly patients: prevalence and comorbidity in general practice. BMJ. 1996; 313:1534.14. Wheeldon NM, Tayler DI, Anagnostou E, Cook D, Wales C, Oakley GD. Screening for atrial fibrillation in primary care. Heart. 1998; 79:50–55.15. Djoussé L, Levy D, Benjamin EJ, Blease SJ, Russ A, Larson MG, Massaro JM, D'Agostino RB, Wolf PA, Ellison RC. Long-term alcohol consumption and the risk of atrial fibrillation in the Framingham Study. Am J Cardiol. 2004; 93:710–713.16. Feinberg WM, Blackshear JL, Laupacis A, Kronmal R, Hart RG. Prevalence, age distribution, and gender of patients with atrial fibrillation. Analysis and implications. Arch Intern Med. 1995; 155:469–473.17. Rosamond WD, Chambless LE, Folsom AR, Cooper LS, Conwill DE, Clegg L, Wang CH, Heiss G. Trends in the incidence of myocardial infarction and in mortality due to coronary heart disease, 1987 to 1994. N Engl J Med. 1998; 339:861–867.18. Brønnum-Hansen H, Jørgensen T, Davidsen M, Madsen M, Osler M, Gerdes LU, Schroll M. Survival and cause of death after myocardial infarction: the Danish MONICA study. J Clin Epidemiol. 2001; 54:1244–1250.19. Capewell S, Livingston BM, MacIntyre K, Chalmers JW, Boyd J, Finlayson A, Redpath A, Pell JP, Evans CJ, McMurray JJ. Trends in case-fatality in 117 718 patients admitted with acute myocardial infarction in Scotland. Eur Heart J. 2000; 21:1833–1840.20. Suzuki S, Sagara K, Otsuka T, Matsuno S, Funada R, Uejima T, Oikawa Y, Koike A, Nagashima K, Kirigaya H, et al. Gender-specific relationship between serum uric acid level and atrial fibrillation prevalence. Circ J. 2012; 76:607–611.21. Sinner MF, Wang N, Fox CS, Fontes JD, Rienstra M, Magnani JW, Vasan RS, Calderwood AH, Pencina M, Sullivan LM, et al. Relation of circulating liver transaminase concentrations to risk of new-onset atrial fibrillation. Am J Cardiol. 2013; 111:219–224.22. Iguchi Y, Kimura K, Kobayashi K, Aoki J, Terasawa Y, Sakai K, Uemura J, Shibazaki K. Relation of atrial fibrillation to glomerular filtration rate. Am J Cardiol. 2008; 102:1056–1059.23. Rienstra M, Sun JX, Lubitz SA, Frankel DS, Vasan RS, Levy D, Magnani JW, Sullivan LM, Meigs JB, Ellinor PT, et al. Plasma resistin, adiponectin, and risk of incident atrial fibrillation: the Framingham Offspring Study. Am Heart J. 2012; 163:119–124.e1.24. Benjamin EJ, Levy D, Vaziri SM, D'Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994; 271:840–844.25. Genovesi S, Pogliani D, Faini A, Valsecchi MG, Riva A, Stefani F, Acquistapace I, Stella A, Bonforte G, DeVecchi A, et al. Prevalence of atrial fibrillation and associated factors in a population of long-term hemodialysis patients. Am J Kidney Dis. 2005; 46:897–902.26. Karmazyn M, Purdham DM, Rajapurohitam V, Zeidan A. Signalling mechanisms underlying the metabolic and other effects of adipokines on the heart. Cardiovasc Res. 2008; 79:279–286.27. Ouchi N, Kihara S, Funahashi T, Nakamura T, Nishida M, Kumada M, Okamoto Y, Ohashi K, Nagaretani H, Kishida K, et al. Reciprocal association of C-reactive protein with adiponectin in blood stream and adipose tissue. Circulation. 2003; 107:671–674.28. Weikert C, Westphal S, Berger K, Dierkes J, Möhlig M, Spranger J, Rimm EB, Willich SN, Boeing H, Pischon T. Plasma resistin levels and risk of myocardial infarction and ischemic stroke. J Clin Endocrinol Metab. 2008; 93:2647–2653.29. Shimano M, Shibata R, Tsuji Y, Kamiya H, Uchikawa T, Harata S, Muto M, Ouchi N, Inden Y, Murohara T. Circulating adiponectin levels in patients with atrial fibrillation. Circ J. 2008; 72:1120–1124.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Left Atrial Size in Hypertensive Patients with Atrial Fibrillation
- Relation between Atrial Fibrillation and Echocardiographic Size of Left Atrium
- Atrial Fibrillation in a Patient with Left Ventricular Hypertrophy after Induction of General Anesthesia: A case report
- Correlation between N-Terminal Pro-Brain Natriuretic Peptide and Doppler Echocardiographic Parameters of Left Ventricular Filling Pressure in Atrial Fibrillation
- Relation of Right Atrial Pathology to Atrial Fibrillation in Mitral Valvular Disease