J Korean Med Sci.
2015 Apr;30(4):442-449. 10.3346/jkms.2015.30.4.442.
One-year Prognosis and the Role of Brain Natriuretic Peptide Levels in Patients with Chronic Cor Pulmonale
- Affiliations
-
- 1Division of Pulmonary, Allergy and Critical Care Medicine, Kangdong Sacred Heart Hospital, Seoul, Korea.
- 2Division of Pulmonary, Allergy and Critical Care Medicine, Chuncheon Sacred Heart Hospital, Chuncheon, Korea.
- 3Division of Pulmonary, Allergy and Critical Care Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 4Division of Pulmonary, Allergy and Critical Care Medicine, Kangnam Sacred Heart Hospital, Seoul, Korea. dongyu@hallym.or.kr
- KMID: 2164452
- DOI: http://doi.org/10.3346/jkms.2015.30.4.442
Abstract
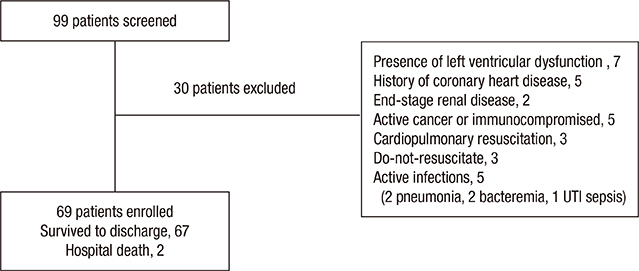
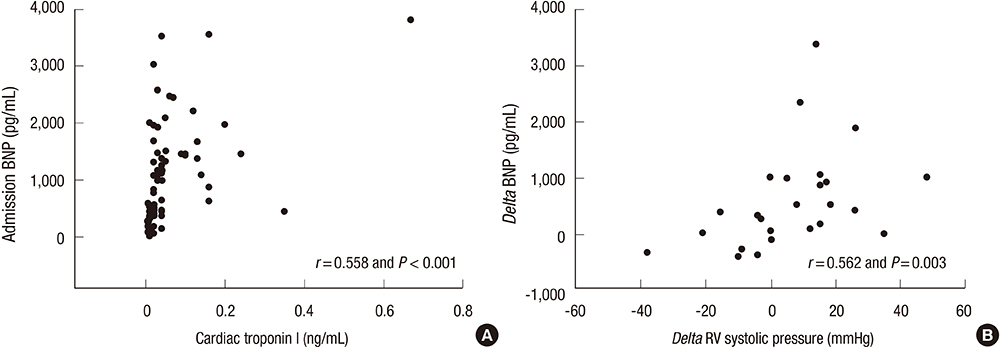
- Data on the clinical outcomes and role of brain natriuretic peptide (BNP) levels in patients with chronic cor pulmonale are limited. A total of 69 patients with chronic cor pulmonale, admitted for dyspnea (January 2007 to September 2011) to three university hospitals, were retrospectively reviewed. All of the patients had right ventricular (RV) dysfunction on echocardiography. The median age was 70.0 yr, and chronic obstructive pulmonary disease (40.6%) and tuberculosis-destroyed lung (TDL, 27.5%) were the leading causes of chronic cor pulmonale. At the 1-yr follow-up, the mortality rate was 15.9%, and the readmission rate was 53.7%; patients with TDL had higher mortality (31.6% vs. 10.0%; P = 0.059) and readmission rates (78.9% vs. 43.8%; P = 0.009) than those with non-TDL diseases. The area under the receiver operating characteristic curve for admission BNP levels to predict readmission was 0.788 (95% confidence interval [CI], 0.673-0.904), and the sensitivity and specificity of the cut-off value were 80.6% and 77.4%, respectively. In multivariate analysis, high admission BNP levels were a significant risk factor for subsequent readmission (hazard ratio, 1.049; 95% CI, 1.005-1.094). Additionally, admission BNP levels were well correlated with cardiac troponin I (r = 0.558), and delta BNP also correlated with delta RV systolic pressure (n = 25; r = 0.562). In conclusion, among hospitalized patients with chronic cor pulmonale, admission high BNP levels are a significant risk factor for subsequent readmission. Therefore, more intensive monitoring and treatment are needed in patients with higher BNP levels.
MeSH Terms
Figure
Cited by 1 articles
-
Predicting Mortality in Patients with Tuberculous Destroyed Lung Receiving Mechanical Ventilation
Won-Young Kim, Mi-Hyun Kim, Eun-Jung Jo, Jung Seop Eom, Jeongha Mok, Ki Uk Kim, Hye-Kyung Park, Min Ki Lee, Kwangha Lee
Tuberc Respir Dis. 2018;81(3):247-255. doi: 10.4046/trd.2017.0126.
Reference
-
1. Weitzenblum E. Chronic cor pulmonale. Heart. 2003; 89:225–230.2. Budev MM, Arroliga AC, Wiedemann HP, Matthay RA. Cor pulmonale: an overview. Semin Respir Crit Care Med. 2003; 24:233–244.3. Campo A, Mathai SC, Le Pavec J, Zaiman AL, Hummers LK, Boyce D, Housten T, Lechtzin N, Chami H, Girgis RE, et al. Outcomes of hospitalisation for right heart failure in pulmonary arterial hypertension. Eur Respir J. 2011; 38:359–367.4. Song JW, Song JK, Kim DS. Echocardiography and brain natriuretic peptide as prognostic indicators in idiopathic pulmonary fibrosis. Respir Med. 2009; 103:180–186.5. Mukoyama M, Nakao K, Hosoda K, Suga S, Saito Y, Ogawa Y, Shirakami G, Jougasaki M, Obata K, Yasue H, et al. Brain natriuretic peptide as a novel cardiac hormone in humans. Evidence for an exquisite dual natriuretic peptide system, atrial natriuretic peptide and brain natriuretic peptide. J Clin Invest. 1991; 87:1402–1412.6. Chaouat A, Naeije R, Weitzenblum E. Pulmonary hypertension in COPD. Eur Respir J. 2008; 32:1371–1385.7. Nagaya N, Nishikimi T, Uematsu M, Satoh T, Kyotani S, Sakamaki F, Kakishita M, Fukushima K, Okano Y, Nakanishi N, et al. Plasma brain natriuretic peptide as a prognostic indicator in patients with primary pulmonary hypertension. Circulation. 2000; 102:865–870.8. Benza RL, Miller DP, Gomberg-Maitland M, Frantz RP, Foreman AJ, Coffey CS, Frost A, Barst RJ, Badesch DB, Elliott CG, et al. Predicting survival in pulmonary arterial hypertension: insights from the Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management (REVEAL). Circulation. 2010; 122:164–172.9. Bozkanat E, Tozkoparan E, Baysan O, Deniz O, Ciftci F, Yokusoglu M. The significance of elevated brain natriuretic peptide levels in chronic obstructive pulmonary disease. J Int Med Res. 2005; 33:537–544.10. Jurcut R, Giusca S, La Gerche A, Vasile S, Ginghina C, Voigt JU. The echocardiographic assessment of the right ventricle: what to do in 2010? Eur J Echocardiogr. 2010; 11:81–96.11. Berger M, Haimowitz A, Van Tosh A, Berdoff RL, Goldberg E. Quantitative assessment of pulmonary hypertension in patients with tricuspid regurgitation using continuous wave Doppler ultrasound. J Am Coll Cardiol. 1985; 6:359–365.12. Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, Barnes PJ, Fabbri LM, Martinez FJ, Nishimura M, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013; 187:347–365.13. Park JH, Na JO, Kim EK, Lim CM, Shim TS, Lee SD, Kim WS, Kim DS, Kim WD, Koh Y. The prognosis of respiratory failure in patients with tuberculous destroyed lung. Int J Tuberc Lung Dis. 2001; 5:963–967.14. Mongia SK, La'ulu SL, Apple FS, Ler R, Murakami MM, Roberts WL. Performance characteristics of the Architect brain natriuretic peptide (BNP) assay: a two site study. Clin Chim Acta. 2008; 391:102–105.15. Arcasoy SM, Christie JD, Ferrari VA, Sutton MS, Zisman DA, Blumenthal NP, Pochettino A, Kotloff RM. Echocardiographic assessment of pulmonary hypertension in patients with advanced lung disease. Am J Respir Crit Care Med. 2003; 167:735–740.16. Miniati M, Monti S, Basta G, Cocci F, Fornai E, Bottai M. Soluble receptor for advanced glycation end products in COPD: relationship with emphysema and chronic cor pulmonale: a case-control study. Respir Res. 2011; 12:37.17. Agrawal BV, Jain PK, Somani PN, Jha VK. Cor pulmonale in pulmonary tuberculosis. J Indian Med Assoc. 1978; 71:4–7.18. Ueda E. Treatment of cor pulmonale as a sequela of pulmonary tuberculosis. Kekkaku. 1989; 64:810–814.19. Rhee CK, Yoo KH, Lee JH, Park MJ, Kim WJ, Park YB, Hwang YI, Kim YS, Jung JY, Moon JY, et al. Clinical characteristics of patients with tuberculosis-destroyed lung. Int J Tuberc Lung Dis. 2013; 17:67–75.20. World health organization. Global tuberculosis report 2013. accessed on 30 December 2013. Available at http://www.Who.Int/tb/publications/global_report/en/.21. Bishop JM, Cross KW. Physiological variables and mortality in patients with various categories of chronic respiratory disease. Bull Eur Physiopathol Respir. 1984; 20:495–500.22. Almagro P, Barreiro B, Ochoa de Echaguen A, Quintana S, Rodriguez Carballeira M, Heredia JL, Garau J. Risk factors for hospital readmission in patients with chronic obstructive pulmonary disease. Respiration. 2006; 73:311–317.23. Ciapponi A, Alison L, Agustina M, Demian G, Silvana C, Edgardo S. The epidemiology and burden of COPD in Latin America and the Caribbean: systematic review and meta-analysis. COPD. 2014; 11:339–350.24. Chen YH, Yao WZ, Cai BQ, Wang H, Deng XM, Gao HL, Huang JS, Wang XM. Economic analysis in admitted patients with acute exacerbation of chronic obstructive pulmonary disease. Chin Med J (Engl). 2008; 121:587–591.25. Filipowski M, Bozek A, Kozlowska R, Czyzewski D, Jarzab J. The influence of hospitalizations due to exacerbations or spontaneous pneumothoraxes on the quality of life, mental function and symptoms of depression and anxiety in patients with COPD or asthma. J Asthma. 2014; 51:294–298.26. Koekkoek D, Bayley KB, Brown A, Rustvold DL. Hospitalists assess the causes of early hospital readmissions. J Hosp Med. 2011; 6:383–388.27. Inoue Y, Kawayama T, Iwanaga T, Aizawa H. High plasma brain natriuretic peptide levels in stable COPD without pulmonary hypertension or cor pulmonale. Intern Med. 2009; 48:503–512.28. Kruger S, Graf J, Merx MW, Koch KC, Kunz D, Hanrath P, Janssens U. Brain natriuretic peptide predicts right heart failure in patients with acute pulmonary embolism. Am Heart J. 2004; 147:60–65.29. Stolz D, Breidthardt T, Christ-Crain M, Bingisser R, Miedinger D, Leuppi J, Mueller B, Tamm M, Mueller C. Use of B-type natriuretic peptide in the risk stratification of acute exacerbations of COPD. Chest. 2008; 133:1088–1094.30. Torbicki A, Kurzyna M, Kuca P, Fijalkowska A, Sikora J, Florczyk M, Pruszczyk P, Burakowski J, Wawrzynska L. Detectable serum cardiac troponin T as a marker of poor prognosis among patients with chronic precapillary pulmonary hypertension. Circulation. 2003; 108:844–848.31. Filusch A, Giannitsis E, Katus HA, Meyer FJ. High-sensitive troponin T: a novel biomarker for prognosis and disease severity in patients with pulmonary arterial hypertension. Clin Sci (Lond). 2010; 119:207–213.32. Heresi GA, Tang WH, Aytekin M, Hammel J, Hazen SL, Dweik RA. Sensitive cardiac troponin I predicts poor outcomes in pulmonary arterial hypertension. Eur Respir J. 2012; 39:939–944.33. Bando M, Ishii Y, Sugiyama Y, Kitamura S. Elevated plasma brain natriuretic peptide levels in chronic respiratory failure with cor pulmonale. Respir Med. 1999; 93:507–514.34. Chaouat A, Bugnet AS, Kadaoui N, Schott R, Enache I, Ducoloné A, Ehrhart M, Kessler R, Weitzenblum E. Severe pulmonary hypertension and chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005; 172:189–194.35. Scharf SM, Iqbal M, Keller C, Criner G, Lee S, Fessler HE. National Emphysema Treatment Trial (NETT) Group. Hemodynamic characterization of patients with severe emphysema. Am J Respir Crit Care Med. 2002; 166:314–322.36. Keller CA, Shepard JW Jr, Chun DS, Vasquez P, Dolan GF. Pulmonary hypertension in chronic obstructive pulmonary disease. Multivariate analysis. Chest. 1986; 90:185–192.37. Nathan SD, Shlobin OA, Ahmad S, Urbanek S, Barnett SD. Pulmonary hypertension and pulmonary function testing in idiopathic pulmonary fibrosis. Chest. 2007; 131:657–663.38. Fisher MR, Criner GJ, Fishman AP, Hassoun PM, Minai OA, Scharf SM, Fessler HE. NETT Research Group. Estimating pulmonary artery pressures by echocardiography in patients with emphysema. Eur Respir J. 2007; 30:914–921.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of Brain Natriuretic Peptide as a Prognostic Marker in Non-Cardiac Surgery
- Clinical Implication of B-type Natriuretic Peptide in the Elderly
- Echocardiographic Evaluation of Right Ventricular Diastolic Function in Patients with Chronic Obstructive Pulmonary Disease
- B-type natriuretic peptide may have a role in the management of patent ductus arteriosus
- Biomarkers in Heart Failure: Focus on B-type Natriuretic Peptide