J Cardiovasc Ultrasound.
2016 Mar;24(1):40-47. 10.4250/jcu.2016.24.1.40.
Myocardial Tissue Doppler Velocity in Child Growth
- Affiliations
-
- 1Division of Pediatric Cardiology, Department of Pediatrics, Yonsei University College of Medicine, Seoul, Korea. lucyeun@yuhs.ac
- KMID: 2160994
- DOI: http://doi.org/10.4250/jcu.2016.24.1.40
Abstract
- BACKGROUND
In adults, tissue Doppler imaging (TDI) is a recommended component of routine echocardiography. However, TDI velocities are less accepted in pediatrics, due to their strong variability and age dependence in children. This study examines the distribution of myocardial tissue Doppler velocities in healthy children to assess the effect of age with cardiac growth on the various echocardiographic measurements.
METHODS
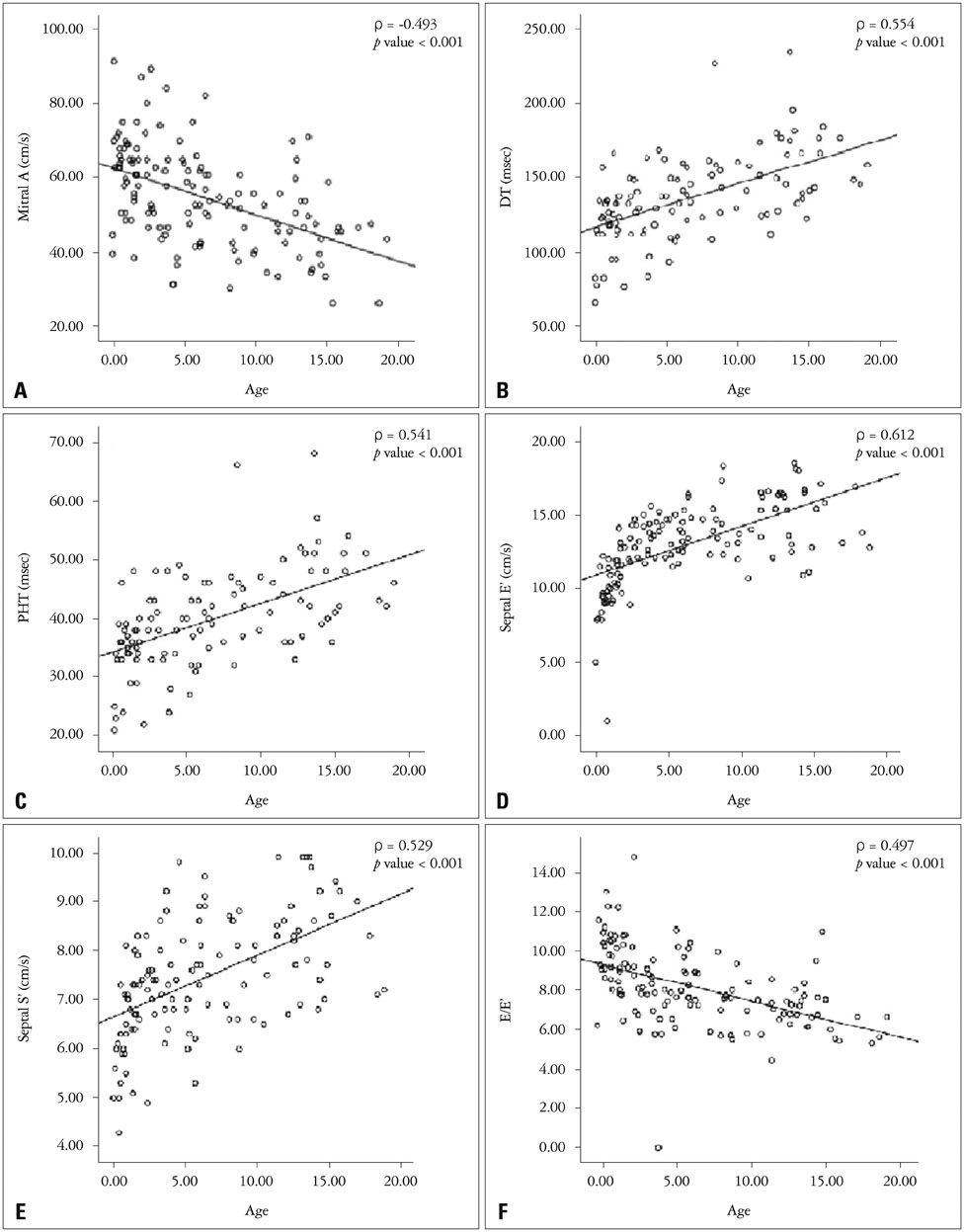
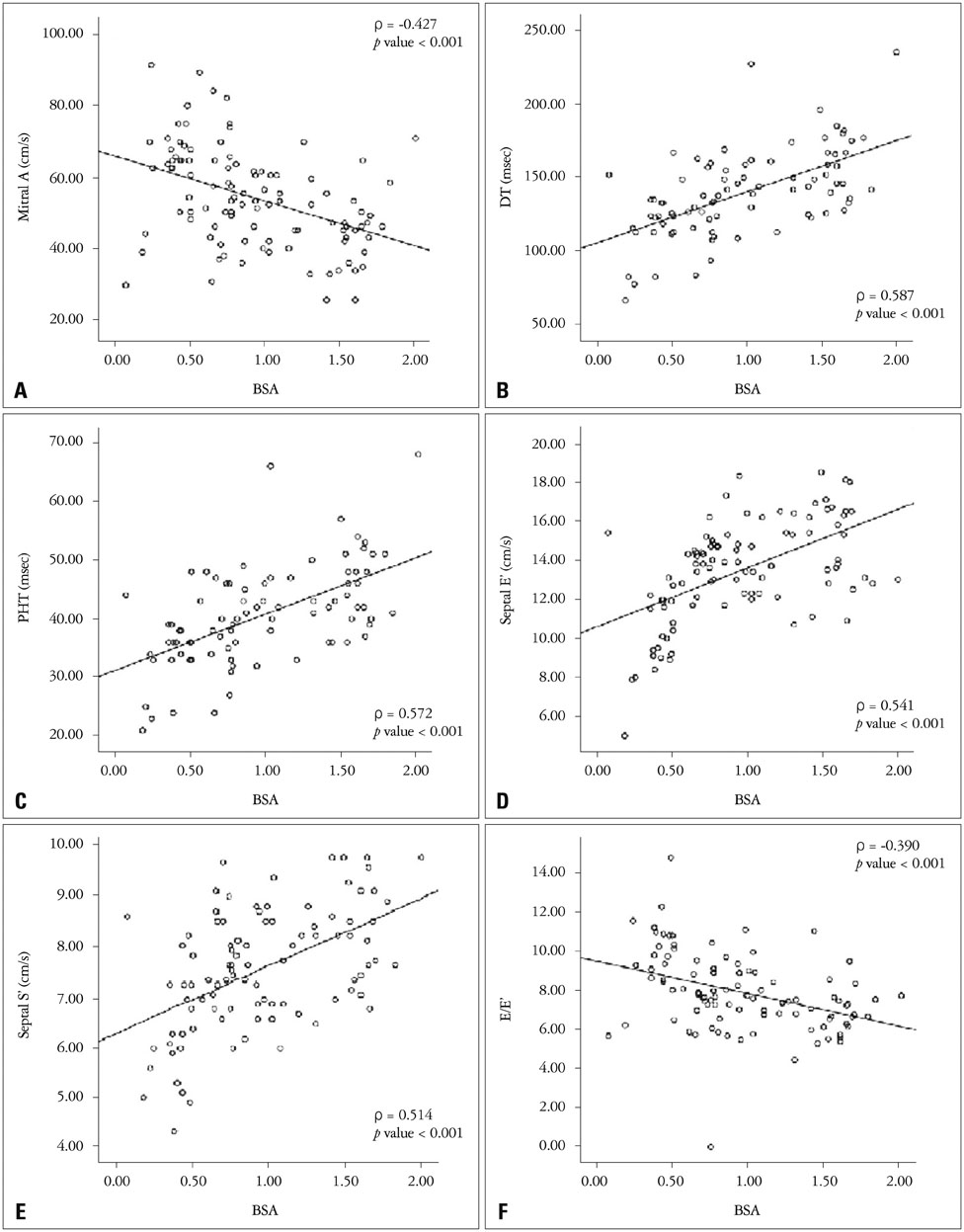
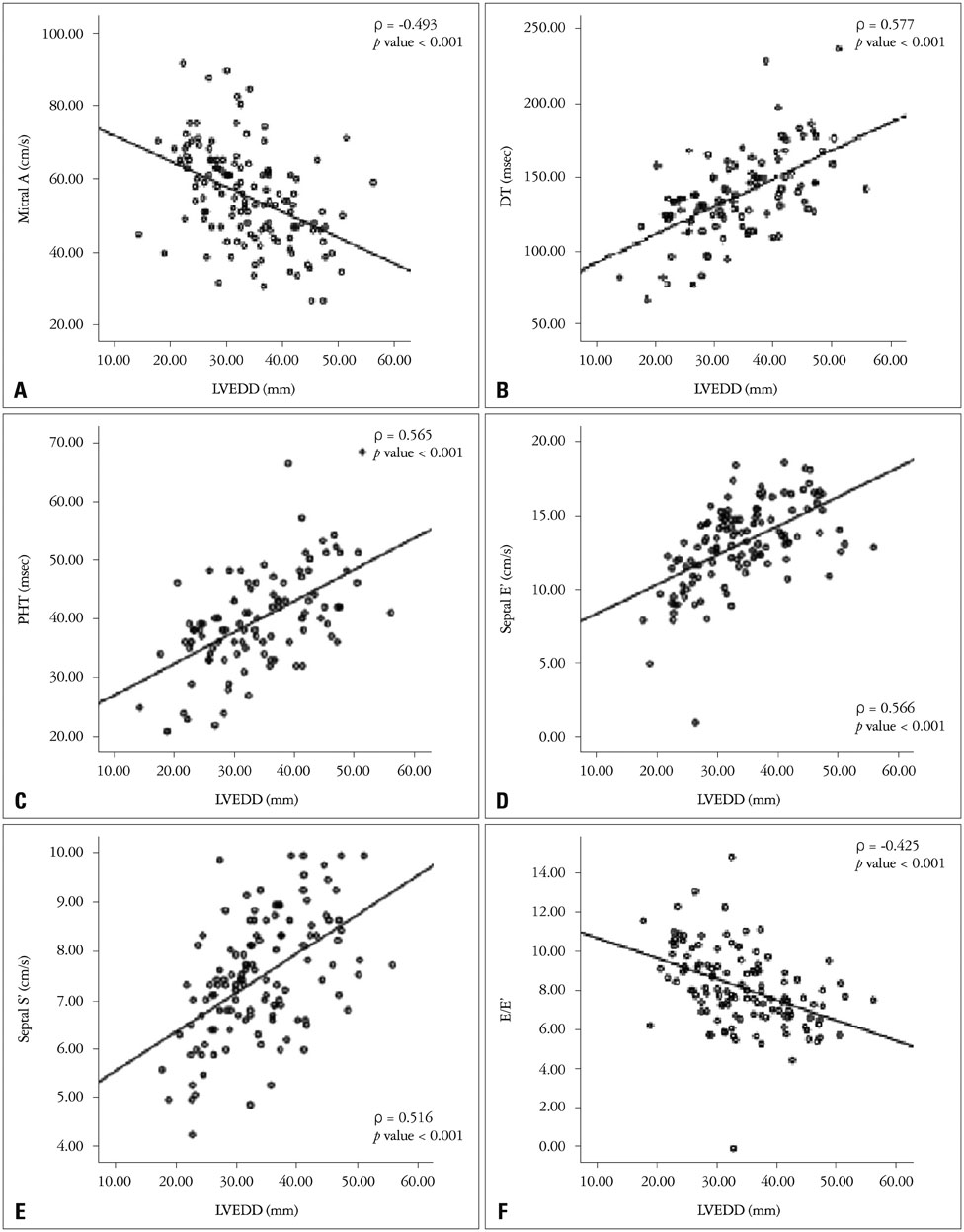
Total 144 healthy children were enrolled in this study. They were recruited from the pediatric outpatient clinic for routine well-child visits. The statistical relationships between age and TDI values were analyzed. Also, the statistical relationships between body surface area (BSA) and TDI values, left ventricle end-diastolic dimension (LVEDD) and TDI values were analyzed. Also, we conducted multivariate analysis of cardiac growth parameters such as, age, BSA, LVEDD and TDI velocity data.
RESULTS
All of the age, BSA, and LVEDD had positive correlations with deceleration time (DT), pressure half-time (PHT), peak early diastolic myocardial velocity, peak systolic myocardial velocity, and had negative correlations with peak late diastolic velocity (A) and the ratio of trans-mitral inflow velocity to early diastolic velocity of mitral annulus (E/E'). In the multivariate analysis, all of the age, BSA, and LVEDD had positive correlations with DT, PHT, and negative correlations with A and E/E'.
CONCLUSION
The cardiac growth parameters related alterations of E/E' may suggest that diastolic myocardial velocities are cardiac growth dependent, and diastolic function has positive correlation with cardiac growth in pediatric group. This cardiac growth related myocardial functional variation would be important for assessment of cardiac involvement either in healthy and sick child.
MeSH Terms
Figure
Reference
-
1. Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelista A. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009; 22:107–133.2. Mottram PM, Marwick TH. Assessment of diastolic function: what the general cardiologist needs to know. Heart. 2005; 91:681–695.3. Pauliks L. Tissue Doppler myocardial velocity imaging in infants and children--a window into developmental changes of myocardial mechanics. Echocardiography. 2013; 30:439–446.4. Kim SY, Hyun MC, Lee SB. Quantitative assessment of myocardial tissue velocity in normal children with Doppler tissue imaging: reference values, growth and heart rate related change. Korean J Pediatr. 2005; 48:846–856.5. Kapusta L, Thijssen JM, Cuypers MH, Peer PG, Daniëls O. Assessment of myocardial velocities in healthy children using tissue Doppler imaging. Ultrasound Med Biol. 2000; 26:229–237.6. Hiarada K, Orino T, Yasuoka K, Tamura M, Takada G. Tissue Doppler imaging of left and right ventricles in normal children. Tohoku J Exp Med. 2000; 191:21–29.7. Mori K, Hayabuchi Y, Kuroda Y, Nii M, Manabe T. Left ventricular wall motion velocities in healthy children measured by pulsed wave Doppler tissue echocardiography: normal values and relation to age and heart rate. J Am Soc Echocardiogr. 2000; 13:1002–1011.8. Eidem BW, McMahon CJ, Cohen RR, Wu J, Finkelshteyn I, Kovalchin JP, Ayres NA, Bezold LI, O'Brian Smith E, Pignatelli RH. Impact of cardiac growth on Doppler tissue imaging velocities: a study in healthy children. J Am Soc Echocardiogr. 2004; 17:212–221.9. Swaminathan S, Ferrer PL, Wolff GS, Gómez-Marín O, Rusconi PG. Usefulness of tissue Doppler echocardiography for evaluating ventricular function in children without heart disease. Am J Cardiol. 2003; 91:570–574.10. Medvedofsky D, Addetia K, Patel AR, Sedlmeier A, Baumann R, Mor-Avi V, Lang RM. Novel approach to three-dimensional echocardiographic quantification of right ventricular volumes and function from focused views. J Am Soc Echocardiogr. 2015; 28:1222–1231.11. Kim H, Yoon HJ, Park HS, Cho YK, Nam CW, Hur SH, Kim YN, Kim KB. Usefulness of tissue Doppler imaging-myocardial performance index in the evaluation of diastolic dysfunction and heart failure with preserved ejection fraction. Clin Cardiol. 2011; 34:494–499.12. Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, Tajik AJ. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation. 2000; 102:1788–1794.13. Bahler RC, Mohyuddin T, Finkelhor RS, Jacobs IB. Contribution of Doppler tissue imaging and myocardial performance index to assessment of left ventricular function in patients with Duchenne's muscular dystrophy. J Am Soc Echocardiogr. 2005; 18:666–673.14. Koestenberger M, Friedberg MK, Ravekes W, Nestaas E, Hansmann G. Non-invasive imaging for congenital heart disease: recent innovations in transthoracic echocardiography. J Clin Exp Cardiolog. 2012; Suppl 8. 2.15. Kiraly P, Kapusta L, Thijssen JM, Daniëls O. Left ventricular myocardial function in congenital valvar aortic stenosis assessed by ultrasound tissuevelocity and strain-rate techniques. Ultrasound Med Biol. 2003; 29:615–620.16. Vogel M, Sponring J, Cullen S, Deanfield JE, Redington AN. Regional wall motion and abnormalities of electrical depolarization and repolarization in patients after surgical repair of tetralogy of Fallot. Circulation. 2001; 103:1669–1673.17. Donazzan L, Stellin G, Rauhe WG, Bonazza L, Stuefer J, Romeo C, Crepaz R. Cardiac resynchronisation therapy associated with pulmonary artery banding in an adult with severe right ventricular dysfunction after Mustard repair for complete transposition of the great arteries: results after 2 years of follow-up. Cardiol Young. 2014; 24:99–104.18. Ahn HM, Jung SO, Kwon JH, Hong YM. Left ventricular dysfunction measured by tissue Doppler imaging and strain rate imaging in hypertensive adolescents. Korean J Pediatr. 2010; 53:72–79.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Peak Myocardial Velocity by Tissue Doppler Imaging in the Children with Myocarditis and Dilated Cardiomyopathy
- Myocardial Function in Infant Kawasaki Disease with Tissue Doppler Imaging
- The Usefulness of Doppler Tissue Image in Evaluation of Left Ventricular Systolic and Diastolic Dysfunction
- Blood flow velocity in the ascending aorta and main pulmonary artery of children by doppler echocardiography
- Evaluation of Left Ventricular Diastolic Function by Measurement of Posterior Myocardial Wall Velocity